Published online Feb 21, 2015. doi: 10.3748/wjg.v21.i7.2210
Peer-review started: July 12, 2014
First decision: August 6, 2014
Revised: September 5, 2014
Accepted: October 14, 2014
Article in press: October 15, 2014
Published online: February 21, 2015
Processing time: 215 Days and 12.2 Hours
Human papillomavirus (HPV) related squamous cell carcinoma (SCC) involving the anal canal is a well-known carcinoma associated with high-risk types of HPV. HPV-related SCC with papillary morphology (papillary SCC) has been described in the oropharynx. We describe, for the first time, a case of anal HPV-related squamous carcinoma with papillary morphology. The tumor arose from the anal mucosa. The biopsies revealed a superficially invasive SCC with prominent papillary features and associated in situ carcinoma. The tumor cells were positive for p16 and were also positive for high-risk types of HPV using chromogenic in situ hybridization. The findings are consistent with a HPV-related SCC of the anal canal with papillary features. This tumor shows histologic features similar to a papillary HPV-related SCC of the oropharynx. Additional studies are needed to characterize these lesions.
Core tip: Human papillomavirus (HPV)-related squamous cell carcinoma with papillary morphology has previously been reported in the oropharynx. Here, we describe the occurrence of such a tumor in the anal canal. The association with high risk HPV is demonstrated and poses the question of whether the HPV infection is responsible for this tumor phenotype.
- Citation: Leon ME, Shamekh R, Coppola D. Human papillomavirus-related squamous cell carcinoma of the anal canal with papillary features. World J Gastroenterol 2015; 21(7): 2210-2213
- URL: https://www.wjgnet.com/1007-9327/full/v21/i7/2210.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i7.2210
Papillary squamous cell carcinoma (SCC) is a SCC variant commonly present in the head and neck region frequently in the larynx, pharynx, tonsils and sinonasal tract[1,2].
We present a rare case of Human papillomavirus (HPV)-related papillary anal SCC; this morphology has not been previously described.
The patient, an 81-year-old female, presented with rectal bleeding, nausea and abdominal pain. A computed tomography (CT) scan showed a mass in the inferior rectum/anus which was poorly delineated. The regional lymph nodes were not enlarged; and there was no evidence of any distant metastatic disease. Her initial colonoscopy showed a 2 cm mass extending from the anal verge into the rectum. Her original biopsy showed a SCC in situ (anal intraepithelial neoplasia 3; not shown). At this point, the patient was referred to our institution. A PET-CT exam from the skull base to mid thigh demonstrated thickening and hypermetabolic activity along the distal rectum. No evidence of hypermetabolic distant metastatic disease from was seen.
As part of her additional work up, the patient underwent an endoscopic ultrasound evaluation with biopsies. The endoscopic ultrasound showed an exophytic anal mass extending 5 cm into the rectum. The mass was hypoechoic and hypervascular and measured 3 cm in largest diameter. This lesion extended through the anterior rectal wall into the perirectal adipose tissue, and involving the internal sphincter anteriorly. Multiple small biopsies were taken. The biopsy tissue was routinely processed for Hematoxylin and Eosin and was subjected to an immunohistochemical stain for p16 using a Ventana anti-p16 antibody (clone E6H4™; CINtec®/Tucson, AZ) and the Polymer detection system, on the Ventana Benchmark Ultra platform (Conditions: CC1 Standard, Ultra Wash, 32mins primary @ 37 C). A chromogenic in-situ hybridization (CISH) study for high-risk types of HPV (INFORM®III HPV assay; Ventana Medical Systems, Inc., AZ, United States) was also performed.
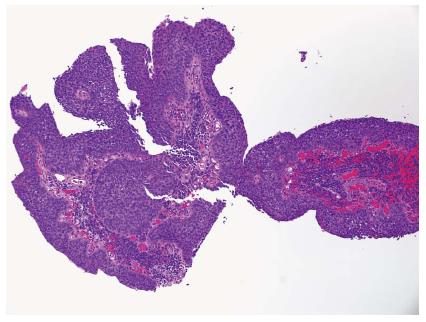
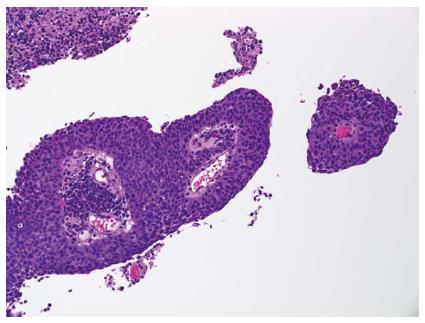
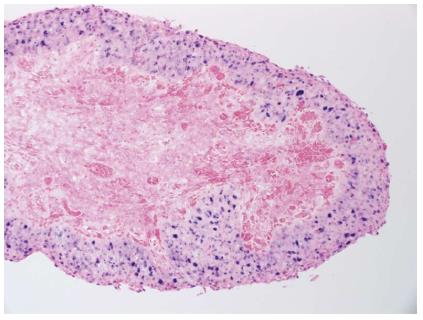
The biopsies taken during the endoscopic ultrasound procedure revealed a superficially invasive SCC with prominent papillary features (Figure 1). There was an associated anal intraepithelial neoplasia grade 3 (carcinoma-situ) (Figure 2). The p16 immunostain intensely decorated the cytoplasm of the tumor cells (Figure 3). Similarly, the chromogenic in situ hybridization for high-risk types of HPV showed epithelial neoplastic cells strongly and diffusely positive (Figure 4). After the diagnosis, the patient underwent treatment with definitive concurrent chemoradiation following the Nigro regimen using 5-fluorouracil and mitomycin and radiation. During her follow up, the patient developed mouth sores, fatigue, and upper chest and upper back rash. Additionally, she had a partial small bowel obstruction due to adhesions that required exploratory laparotomy and lysis of adhesions, a sacral pressure sore after a left-sided pelvic fracture, and Clostridium difficile colitis.
SCC of the anal canal usually occurs in the sixth or seventh decade of life. The incidence of these lesions is higher among human immunodeficiency virus positive homosexual men[3]. The current case shows a rare presentation of a HPV-related SCC with papillary features. Histologically, the phenotype of the tumor was a SCC with definite papillary features arising from a carcinoma in situ. The morphology consistent with SCC cells was characteristic; the tumor showed a stratified epithelium with basaloid to squamoid cells with high nuclear to cytoplasmic ratios. The nuclei were round to oval with irregular outlines. At this location, the differential diagnosis includes anal intraepithelial neoplasia, adenocarcinoma, and malignant melanoma. Adenocarcinomas are distinguished by the glandular appearance of the tumor cells and their cytologic characteristics. Adenocarcinoma tumor cells show an eccentrically located nucleus and cytoplasmic vacuoles. In poorly differentiated adenocarcinoma cases, immunohistochemistry may be helpful; the tumor cells of adenocarcinoma are negative for p40 and p63. Malignant melanomas arising in this location are rare; these cells may show pigmentation, marked pleomorphism with prominent nucleoli, binucleation, and eccentrically located nuclei. The tumor cells in melanoma are positive for S-100 protein, HMB-45, melan-A, and MiTF. In squamous carcinoma cases, the tumor cells are usually positive for CK 5/6, p40, and p63. HPV-related carcinomas are characteristically positive for p16. The identification of HPV is performed by CISH with probes specific for High-risk types of HPV. A CISH for HPV is usually positive with a focal to diffuse punctate pattern within the cell nuclei. In our case, the tumor cells were strongly and diffusely positive for p16 and high-risk HPV CISH. HPVs are detected in the majority of SCCs of the anus and the anal canal. Of the HPVs, the High-risk HPVs, particulary16 and 18, are known to cause cervical SCC and oropharyngeal SCC; however, both high and low risk HPVs (6, 16, 18, 31, 42) have been described in subtypes of SCCs subtypes of anogenital lesions[4].
Anal SCC shows the classic morphology involving the epithelium; the lesion may be accompanied and preceded by pre-neoplastic process, anal intraepithelial neoplasia (AIN1-3). Most anal SCCs show a condylomatous/exophytic growth; the definite papillary features seen in this case have not been previously described at this site. However, HPV-related SCC with papillary morphology, (papillary SCC), has been described in the oropharynx, specially the tonsil[2,5,6]. Our case showed features similar to those seen in these tonsillary tumors. To the best of our knowledge, this pattern has not been reported in HPV-related SCCs of the anal region. In the head and neck, papillary SCC often presents as solitary lesion characterized by an exophytic and papillary growth with immature-appearing severely dysplastic squamous epithelium[2]. Given the better prognosis of HPV associated papillary SCCs in the head and neck, it might be essential to report the p16 and HPV status of HPV-related tumors when they are encountered to better characterize this cohort. The modality of treatment of anal SCC is surgery for small and superficial lesions. Radiation alone, and definite treatment with chemoradiation are also employed; these later modality of treatment is the preferred one due to its better results.
In summary, we presented an anal HPV-related SCC with papillary features. Whether, this is a distinctive pattern of tumor development, a phenotype that appears during the tumor growth, or whether this is a distinct type of HPV-related SCC of the anal canal is not apparent at this time. The characterization of this patten will help to identify these lesions. Additional studies are needed to further characterize these lesions.
We like to thank Jacki Hattle for helping with formatting and submission of this paper. We also thank Helen Molina, Supervisor of Histology and Moffitt Cancer Center for performing the Histological and immunohistochemical stains and CISH.
An 81-year-old female presented with nausea, rectal bleeding, and abdominal pain.
Anal lesion.
Anal squamous cell carcinoma (SCC), anal intraepithelial neoplasia, anal adenocarcinoma, and melanoma.
Laboratory diagnosis
WBC 6.86 k/uL; HGB 14.4 gm/dL; CEA 1.20 ng/mL; metabolic panel showed a high potassium 5.3 mmol/L; the remaining results were within normal limits. The liver function test were within normal limits.
PET-CT exam from the skull base to midthigh demonstrates thickening and hypermetabolic activity along the distal rectum. No evidence of viable distant metastatic disease otherwise from skull base to midthigh is noted.
The biopsies revealed a superficially invasive SCC with prominent papillary features and associated in situ carcinoma. The tumor cells were positive for p16 and were also positive for high-risk types of Human papillomavirus (HPV) using chromogenic in situ hybridization (CISH).
The patient underwent definitive concurrent chemoradiation following the Nigro regimen using 5-fluorouracil and mitomycin and radiation.
HPV-related SCCs have been reported in the oropharynx (tonsil); to our knowledge, a HPV anal squamous cell with papillary features has not been reported.
HPV is a DNA virus associated with cervical, vaginal, vulvar, anal, penile, and oropharyngeal cancer. CISH is a common technique that uses specific DNA probes attached to chromogenic substances that can be seen in a light microscope; this test is valuable in the identification of the HPV DNA in tissue sections.
This case report represents a newly described histopathologic feature in anal HPV-related SCC. This feature might be closely associated with HPV; further studies are needed to clarify this issue.
This is an interesting case to know. Share the following features: The occurrence of HPV-related SCC of the anal canal in a patient of 81 years HIV negative. The papillary features morphology and its relationship with high-risk HPV that are usually implicated in SCC of the oropharyngeal orophayngal region, especially the tonsils.he
P- Reviewer: Berkane S, Bove A S- Editor: Ma YJ L- Editor: A E- Editor: Liu XM
| 1. | Fletcher CDM. Diagnostic Histopathology of Tumors. 2007;. |
| 2. | Jo VY, Mills SE, Stoler MH, Stelow EB. Papillary squamous cell carcinoma of the head and neck: frequent association with human papillomavirus infection and invasive carcinoma. Am J Surg Pathol. 2009;33:1720-1724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 91] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 3. | Pernot S, Terme M, Zaanan A, Tartour E, Weiss L, Taieb J. Immunity and squamous cell carcinoma of the anus: epidemiological, clinical and therapeutic aspects. Clin Res Hepatol Gastroenterol. 2014;38:18-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Guimerà N, Lloveras B, Lindeman J, Alemany L, van de Sandt M, Alejo M, Hernandez-Suarez G, Bravo IG, Molijn A, Jenkins D. The occasional role of low-risk human papillomaviruses 6, 11, 42, 44, and 70 in anogenital carcinoma defined by laser capture microdissection/PCR methodology: results from a global study. Am J Surg Pathol. 2013;37:1299-1310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 5. | Bishop JA, Guo TW, Smith DF, Wang H, Ogawa T, Pai SI, Westra WH. Human papillomavirus-related carcinomas of the sinonasal tract. Am J Surg Pathol. 2013;37:185-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 204] [Article Influence: 17.0] [Reference Citation Analysis (0)] |