Published online Feb 21, 2015. doi: 10.3748/wjg.v21.i7.2152
Peer-review started: June 3, 2014
First decision: July 9, 2014
Revised: July 18, 2014
Accepted: September 5, 2014
Article in press: September 5, 2014
Published online: February 21, 2015
Processing time: 256 Days and 2 Hours
AIM: To combine community and hospital services in order to enable improvements in patient management, an integrated gastroenterology service (IGS) was established.
METHODS: Referral patterns to specialist clinics were optimized; open access route for endoscopic procedures (including esophago-gastro-duodenoscopy, sigmoidoscopy and colonoscopy) was established; family physicians’ knowledge and confidence were enhanced; direct communication lines between experts and primary care physicians were opened. Continuing education, guidelines and agreed instructions for referral were promoted by the IGS. Six quality indicators were developed by the Delphi method, rigorously designed and regularly monitored. Improvement was assessed by comparing 2010, 2011 and 2012 indicators.
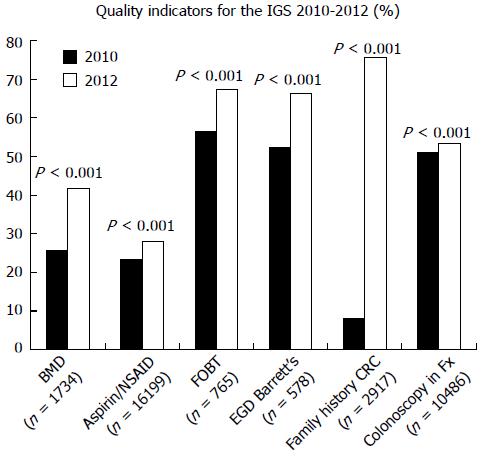
RESULTS: An integrated delivery system in a specific medical field may provide a solution to a fragmented healthcare system impaired by a lack of coordination. In this paper we describe a new integrated gastroenterology service established in April 2010. Waiting time for procedures decreased: 3 mo in April 30th 2010 to 3 wk in April 30th 2011 and stayed between 1-3 wk till December 30th 2012. Average cost for patient’s visit decreased from 691 to 638 NIS (a decrease of 7.6%). Six health indicators were improved significantly comparing 2010 to 2012, 2.5% to 67.5%: Bone densitometry for patients with inflammatory bowel disease, preventive medications for high risk patients on aspirin/NSAIDs, colonoscopy following positive fecal occult blood test, gastroscopy in Barrett’s esophagus, documentation of family history of colorectal cancer, and colonoscopy in patients with a family history of colorectal cancer.
CONCLUSION: Establishment of an IGS was found to effectively improve quality of care, while being cost-effective.
Core tip: We combined community and hospital services in order to improve patient management, and established an integrated gastroenterology service (IGS). Referral patterns to specialist clinics were optimized; open access route for endoscopic procedures was established; family physicians' knowledge was enhanced; direct communication lines between experts and primary care physicians were opened. Six quality indicators were developed and regularly monitored. Waiting time for procedures decreased significantly, the average cost for patient's visit decreased 7.6%. Six health indicators were improved significantly comparing, 2.5% to 67.5% of the goals. Establishment of an IGS was found to effectively improve quality of care, while being cost-effective.
- Citation: Niv Y, Dickman R, Levi Z, Neumann G, Ehrlich D, Bitterman H, Dreiher J, Cohen A, Comaneshter D, Halpern E. Establishing an integrated gastroenterology service between a medical center and the community. World J Gastroenterol 2015; 21(7): 2152-2158
- URL: https://www.wjgnet.com/1007-9327/full/v21/i7/2152.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i7.2152
Clalit Health Services (CHS) is a large health care provider for 4.6 million enrollees in Israel. This is the country’s largest health organization with an annual budget of approximately 17 billion New Israeli Shekel (NIS). The organization has two major medical branches; a community based service divided into eight geographical districts, each with a separate budget and regional director, and a hospital division comprising 14 hospitals providing acute care, chronic care and psychiatric care. The administrative structure has undergone a series of changes in the last three decades, to improve the function of this large organization. Under this system each community-based regional branch of CHS purchases essential services from hospitals. In effect, there is economic conflict of interest between the hospitals and the regional districts, even though both form integral parts of the same organization. In addition, the districts also provide specialist services in the community similar to that provided by the hospitals. The regions are not bound, as consumers, to buy medical services from CHS-owned hospitals, and can use economic criteria as the basis for their decisions. Thus, the regions can sign contracts with governmental, municipal or private hospitals. As a result, there is some competition between hospitals, although they belong to the same organization.
In most Western countries, the healthcare system is divided between family medicine and different levels of specialist medicine. Communication between various professionals is often ineffective, and there are often different patient files for different disciplines. Physicians are thus unable to obtain a comprehensive clinical picture for patients. This led to large healthcare organizations such as Kaiser Permanente to integrate patient care under one "umbrella" organization in order to provide all levels of patient care from family medicine to the most advanced hospital procedures. This framework allows for maximum coordination between various levels, usually using a computerized medical record. A program like this prevents the insured from obtaining non-essential treatment on the one hand, but provides all their real health needs on the other hand[1].
In 2009 it was decided to establish an integrated gastroenterology service (IGS) for one of the 8 regions of CHS (Dan-Petach Tikva region) with Rabin Medical Center (RMC) comprising Beilinson and Sharon hospitals. The IGS has a single management structure to administer gastroenterology services for 340000 individuals insured by CHS, including three endoscopy units. A one-time fee based on service levels in 2008 was transferred by community region to RMC at the beginning of the budget year 2010, as payment for patient gastroenterology services for a year. The IGS undertook to streamline and improve the quality of services and provide readily available gastroenterology clinic consultations and endoscopic procedures in the different units. IGS has also provided a gradual increase in endoscopic procedures with a gradual transition from clinics to endoscopy, for example, colonoscopy for early detection of colon cancer in the community unit, and the increased use of surgical endoscopic procedures in hospitals[2,3].
In this manuscript we describe the establishment of the IGS and evaluate its success. We hypothesized that by optimizing referral patterns to specialist clinics, establishing an open access route for endoscopic procedures, enhancing family physicians’ knowledge by continuing education and guidelines promotion we improved the quality of the gastroenterology service. Six quality indicators were developed and monitored. Improvement was assessed by comparing 2010, 2011 and 2012 indicators.
On 04/22/2010 the IGS was officially established, together with a number of organizational changes. The IGS is the product of cooperation between the regional authority, the medical centers and the general management of CHS. The project was encouraged by CHS’s CEO and deputy CEOs for community health services and hospitals. The vision was to promote the quality of community and hospital gastroenterology care for individuals insured by the health fund. The added value offered by the IGS derives from the fact that the family doctor, gastroenterologists in the community and hospital gastroenterologists belong to the same organization and this enables a more integrated approach to patient care. For example, simpler endoscopic procedures take place in the community unit, whereas more complex procedures and procedures in high risk patients are performed in the hospitals. The Sharon Hospital provides regional health care services and Beilinson Hospital is a tertiary hospital in which the highest level of services is available.
Clinical guidelines: In order to increasing the level of knowledge in gastroenterology among primary care physicians, simple clinical guidelines have been established in the IGS, covering the major topics in gastroenterology (e.g., neurogastroenterology, gastroesophageal reflux, peptic disease, functional diseases, malignant diseases of the gastrointestinal tract, inflammatory bowel disease and liver diseases). The guidelines have been distributed to all family physicians and are attached to the patient electronic file.
Clinical guidelines conference: A clinical guidelines conference is held every three months to promote accepted clinical practice and strengthen the link between family physicians and the gastroenterologist. At each conference three or four central issues are presented and discussed.
Direct contact between family physicians and consultants: A gastroenterologist from the IGS has been attached to each of the large clinics in the district. Each month the family physicians in the clinic hold a joint meeting with the referent gastroenterologist, where cases are presented and a certain topic is discussed. This meeting can save many referrals for unnecessary testing which can be performed in the clinic in the community.
Internet-based consultations: The availability to exchange emails via the CHS e-mail system or in urgent cases the possibility of consulting by telephone has created a new dimension for interaction between family physicians and gastroenterologists. Each side became familiar with their counterpart and a combined approach leads to improved patient care.
Internet portal: An internet portal has been created specifically for the IGS as an additional independent tool for use by gastroenterologists and family physicians in the district. There are sections for notifications, forms, presentations, articles, quality control, clinical guidelines and interactions between specialist clinic advisors and their primary care clinics (this was also used for the quality improvement assessment of referrals and answers to questions). Family physicians can print forms for patient referral, preparation for endoscopy, and open access endoscopy or complete them electronically and send them via the portal.
Joint patient file: The units comprising the IGS, i.e., hospital units and community based unit, all use a uniform electronic medical record ("Clicks" by Rosh Tov, Israel). Despite this, the program has been developed in different ways before the services were integrated. One of the first projects was establishing a unified format for electronic patient files in all of the units so that all the relevant information will be available no matter where the patient is seen.
Integration of the patient file into primary health care clinics: Family physicians use yet another version of the Clicks program and communication between the specialist and community version has been made possible. For example, a family physician is able to fill in a request for colonoscopy or a breath test for Helicobacter pylori and the form is received at the hospital.
Uniformity of instructions for endoscopy: It is important that instructions for endoscopy preparation and the relevant related forms be uniform to avoid confusion for family doctors and patients. These are the same no matter from which unit or primary clinic the patient receives them.
Direct referral by family physicians for endoscopy: A form has been designed for direct referral by family physicians for endoscopic procedures. The form includes the underlying medical problems, reason for referral and contraindications. The form has been approved by a risk management team, physicians' representatives and management. Family practitioners are authorized to refer patients directly for colonoscopy, sigmoidoscopy and gastroscopy but are also responsible for verifying the necessity of the procedure and excluding potential contraindications.
Call center for appointments: A joint call center for coordinating appointments for the IGS has been established. Patients can be given appointments for any one of the IGS units, depending on the nature of the procedure and availability.
In order to assess clinical quality and define whether the IGS archived the set targets in this area, the Chief Physician’s Office for CHS organized a quality indicator conference for IGS staff, family physicians and district management. Delphi process with plenary sessions and discussion groups helped to define 6 quality indicators which included procedures, service measurements, outcomes and were considered accountable[4,5]. Bone densitometry for patients with inflammatory bowel disease[6-11], preventive medications for high risk patients on aspirin/NSAIDs[12-15], colonoscopy following positive fecal occult blood test[16-18], gastroscopy in Barrett’s esophagus[19-22], documentation of family history of colorectal cancer[23-27], and colonoscopy in patients with a family history of colorectal cancer[28-30] (Table 1). Special projects such as enhancing compliance of patients with a positive result of fecal occult blood test (FOBT) to undergo colonoscopy or screening for occult hepatitis C infection were performed.
| Indicator | Denominator | Numerator |
| Bone densitometry for patients with IBD (6-11) | Patients > 20 yr old with Crohn’s disease or ulcerative colitis | Of those in the denominator, patients who underwent bone densitometry |
| Preventive medications for high risk patients on aspirin/NSAIDs (12-15) | High-risk patients (> 70 yr old, underlying comorbidity1 or concomitant medications2) on chronic aspirin/NSAIDs therapy | Of those in the denominator, patients who were purchased proton pump inhibitors |
| Colonoscopy following positive FOBT (16-18) | Patients with positive FOBT | Of those in the denominator, patients who underwent colonoscopy within 6 mo |
| EGD in Barrett's esophagus (19-22) | Patients with a diagnosis of Barret's esophagus | Of those in the denominator, patients who underwent EGD within the last 3 yr |
| Documentation of family history of CRC (positive or negative) (23-27) | Documentation of family history of CRC | Patients with a positive family history of CRC |
| Colonoscopy in-patients with a family history of CRC (28-30) | Patients who underwent colonoscopy | Of those in the denominator, patients who had a family history of CRC |
Flow charts have been created to improve the movement of patients in clinics and endoscopy units in the IGS and also incorporating the family physicians and gastroenterologists. This allows increased and more efficient planning and utilization of services.
During morning sessions, endoscopy rooms in the 3 units of the IGS are utilized by medical and nursing staff with the aim of maximizing availability and reduce waiting lists. However, it may be necessary from time to time to operate the service in the afternoons at the discretion of the Head of the IGS.
A steering committee to oversee the operation of the IGS has been formed with hospital and district managers, medical directors and director of the IGS. This committee meets quarterly and receives a report including activity, productivity and budget. The committee is committed to promoting the processes and aims of the IGS.
The number of endoscopic procedures performed in the 11 endoscopy rooms of the IGS was 18229, 20579 and 23394 in 2010, 2011 and 2012, respectively. In these periods consultations reached the number of 40300, 40253 and 43393. Thus, between the establishment year of the IGS in 2010 and 2012 there was a larger increase of 28.3% in endoscopic procedures than of 7.7% in the consultation numbers (P < 0.001). This outcome was well in line with our strategy to increase the number of endoscopic procedures and decrease the number of unnecessary consultations. While the number of consultations and procedures increased, the total cost decreased from 15030183 IS to 14235223 IS (-5.2%). The average individual cost decreased from 691 NIS per endoscopic procedure to 638 NIS (-7.6%).
The waiting time for consultation and endoscopic procedure decreased from 2 and 3 mo at the beginning of 2010, to 2 wk and 3 wk at the end of 2012, respectively.
Quality indicators monitored continuously are listed in Table 1. Modest improvements were seen in all six quality indicators (Figure 1). There were 5583, 6911, and 8201 entrances to the IGS portal on 2010, 2011 and 2012, respectively; an increase of 46.9% between 2010 and 2012.
Proactive detection projects of patients with a positive FOBT who refused colonoscopy, and patients with a positive serology for hepatitis C were established. Out of 1595 screenies with a positive FOBT on 2009, 570 (35.7%) did not underwent colonoscopy within 6 mo of getting the invitation. These patients were approached again by their family physician and by a gastroenterologist and referred again to the procedure. Two hundred and fifty eight asymptomatic patients with a positive serology to hepatitis C were diagnosed and referred to our liver clinic. Of these 159 (61.6%) had a positive PCR and were treated.
Inadequate access to specialty care is one of the main problem for utilization of specialty care, which cannot give answer to the rising number of referrals[31,32]. Waiting time for appointments is very long and sometimes unacceptable[33]. Routine follow-up care, such as appointment to receive biopsy results after endoscopic procedure, as well as unjustified referrals, may contribute to this problem[34]. Implementation of eReferral, an electronic system, may help in this regard, but this is only small part of a comprehensive integrative solution, with participation of the experts and the primary care providers[35]. Several solutions were suggested to shorten the waiting time for expert consultation or procedure: Increase personnel, strengthening primary care physician capacity via education, using telehealth technologies, improving communication between health providers, and more[35-44].
The IGS is the product of cooperation between CHS community district and Rabin Medical Center and was established in April 2010. The vision was to improve the quality of gastroenterology services in the community and hospitals for the benefit of the patients. Parameters to determine if the stated aims are being achieved are used to inform those involved as to their success.
Many efforts were directed toward the primary care physician, for performing better referrals and prevent unnecessary consultations and endoscopic procedures. Since the IGS establishment 7 conferences took place, dealing in depth with guidelines for diagnosis, treatment and referral patterns in the most prevalent gastroenterological diseases. In addition, very efficient communication pathways were established between the primary care physicians and the consultants, using e-mails, internet portal and telephone calls. In many cases the primary physician is consulting the expert before referral of the patients, and in many cases the message to the patients was: “I’m consulting with my specialist colleague to see what else we need to do, which may include sending you to the specialty clinic for a visit”. This approach was previously tried successfully[45].
After 3 years from the IGS establishment a significant improvement was observed in service availability. The average cost per procedure decreased even though the number of procedures increased. All quality indicators were improved.
In conclusion, an integrated gastroenterology service is important for quality improvement of the clinical service given to the population. Collaboration between the expert and the primary physician is the key factor for success of such a service. Continuous measuring quality of management will enable continuing improving our service while saving money and resources.
We thank Gerald Fraser, Ido lax, Yossi Barel, Yossi Meirovitch, Moshe Kostiner, Orit Bodner, Ehud Davidson, Eytan Wirtheim, Orit Jacobson, Nicky Lieberman, and Ran Balicer for their help establishing the integrated gastroenterology service.
In most Western countries, the healthcare system is divided between primary and specialist medicine. Communication between various professionals is often ineffective, and there are often different patient files for different disciplines. Physicians are thus unable to obtain a comprehensive clinical picture for patients.
An integrated gastroenterology service (IGS) was established, to combine community and hospital services, in order to enable improvements in patient management and treatment.
After 3 years IGS was found to effectively improve quality of care, while being cost-effective.
Establishing integrating professional service between hospitals and the community will improve communication, continuity of care, and patients’ safety.
Integrated Gastroenterology Service is a new professional modality, combined patient care in-hospital and in the community.
This article assesses the effectiveness of integrated gastroenterology service and concluded that integrated gastroenterology service improves quality of care. This article is well written and informative. It is worth for publishing.
P- Reviewer: Solinas A, Tamai N S- Editor: Ma YJ L- Editor: A E- Editor: Zhang DN
| 1. | Enthoven AC. Integrated delivery systems: the cure for fragmentation. Am J Manag Care. 2009;15:S284-S290. [PubMed] |
| 2. | Levin B, Lieberman DA, McFarland B, Andrews KS, Brooks D, Bond J, Dash C, Giardiello FM, Glick S, Johnson D. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134:1570-1595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1423] [Cited by in RCA: 1457] [Article Influence: 85.7] [Reference Citation Analysis (0)] |
| 3. | Sodergren MH, Clark J, Athanasiou T, Teare J, Yang GZ, Darzi A. Natural orifice translumenal endoscopic surgery: critical appraisal of applications in clinical practice. Surg Endosc. 2009;23:680-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Cohen AD, Dreiher J, Regev-Rosenberg S, Yakovson O, Lieberman N, Goldfracht M, Balicer RD. [The quality indigators program in Clalit Health Services: the first decade]. Harefuah. 2010;149:204-209, 265. [PubMed] |
| 5. | Chassin MR, Loeb JM, Schmaltz SP, Wachter RM. Accountability measures--using measurement to promote quality improvement. N Engl J Med. 2010;363:683-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 350] [Cited by in RCA: 342] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 6. | Miheller P, Lorinczy K, Lakatos PL. Clinical relevance of changes in bone metabolism in inflammatory bowel disease. World J Gastroenterol. 2010;16:5536-5542. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Schulte C, Dignass AU, Mann K, Goebell H. Reduced bone mineral density and unbalanced bone metabolism in patients with inflammatory bowel disease. Inflamm Bowel Dis. 1998;4:268-275. [PubMed] |
| 8. | Bjarnason I, Macpherson A, Mackintosh C, Buxton-Thomas M, Forgacs I, Moniz C. Reduced bone density in patients with inflammatory bowel disease. Gut. 1997;40:228-233. [PubMed] |
| 9. | Lewis NR, Scott BB. Guidelines for osteoporosis in inflammatory bowel disease and celiac disease. London: British Society of Gastroenterology 2007; . |
| 10. | Bishop N, Braillon P, Burnham J, Cimaz R, Davies J, Fewtrell M, Hogler W, Kennedy K, Mäkitie O, Mughal Z. Dual-energy X-ray aborptiometry assessment in children and adolescents with diseases that may affect the skeleton: the 2007 ISCD Pediatric Official Positions. J Clin Densitom. 2008;11:29-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 89] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 11. | Bernstein CN, Fried M, Krabshuis JH, Cohen H, Eliakim R, Fedail S, Gearry R, Goh KL, Hamid S, Khan AG. World Gastroenterology Organization Practice Guidelines for the diagnosis and management of IBD in 2010. Inflamm Bowel Dis. 2010;16:112-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 369] [Article Influence: 24.6] [Reference Citation Analysis (1)] |
| 12. | Pilotto A, Franceschi M, Leandro G, Paris F, Cascavilla L, Longo MG, Niro V, Andriulli A, Scarcelli C, Di Mario F. Proton-pump inhibitors reduce the risk of uncomplicated peptic ulcer in elderly either acute or chronic users of aspirin/non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther. 2004;20:1091-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 52] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Yilmaz S, Bayan K, Dursun M, Canoruç F, Kilinç N, Tüzün Y, Daniş R, Ertem M. Does adding misoprostol to standard intravenous proton pump inhibitor protocol improve the outcome of aspirin/NSAID-induced upper gastrointestinal bleeding?: a randomized prospective study. Dig Dis Sci. 2007;52:110-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Antman EM, Bennett JS, Daugherty A, Furberg C, Roberts H, Taubert KA. Use of nonsteroidal antiinflammatory drugs: an update for clinicians: a scientific statement from the American Heart Association. Circulation. 2007;115:1634-1642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 553] [Cited by in RCA: 543] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 15. | Abraham NS, Hlatky MA, Antman EM, Bhatt DL, Bjorkman DJ, Clark CB, Furberg CD, Johnson DA, Kahi CJ, Laine L. ACCF/ACG/AHA 2010 expert consensus document on the concomitant use of proton pump inhibitors and thienopyridines: a focused update of the ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use. A Report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. J Am Coll Cardiol. 2010;56:2051-2066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 164] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 16. | Smith RA, Cokkinides V, von Eschenbach AC, Levin B, Cohen C, Runowicz CD, Sener S, Saslow D, Eyre HJ. American Cancer Society guidelines for the early detection of cancer. CA Cancer J Clin. 2002;52:8-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 261] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 17. | U.S. Preventive Services Task Force. Screening for colorectal cancer: recommendation and rationale. Ann Intern Med. 2002;137:129-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 426] [Cited by in RCA: 424] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 18. | National Committee for Quality Assurance (NCQA) HEDIS® 2011: Healthcare Effectiveness Data and Information Set. Volume 1, narrative Washington (DC): National Committee for Quality Assurance (NCQA); 2010. Available from: http://www.ncqa.org/HEDISQualityMeasurement/HEDISMeasures/HEDIS2011.aspx. |
| 19. | American Gastroenterological Association Institute, Physician Consortium for Performance Improvement®, National Committee for Quality Assurance. Gastroesophageal reflux disease (GERD) physician performance measurement set. Chicago (IL): American Medical Association, National Committee for Quality Assurance; 2007; 9 Available from: http://www.qualitymeasures.ahrq.gov/popups/printView.aspx?id=28121. |
| 20. | Grover M, Strickland C, Kesler E, Crawford P. How should patients with Barrett’s esophagus be monitored? J Fam Pract. 2006;55:243-247. [PubMed] |
| 21. | Sampliner RE. Updated guidelines for the diagnosis, surveillance, and therapy of Barrett’s esophagus. Am J Gastroenterol. 2002;97:1888-1895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 567] [Cited by in RCA: 504] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 22. | Management of Barrett’s esophagus. The Society for Surgery of the Alimentary Tract (SSAT), American Gastroenterological Association (AGA), American Society for Gastrointestinal Endoscopy (ASGE) Consensus Panel. J Gastrointest Surg. 2000;4:115-116. [PubMed] |
| 23. | Sifri RD, Wender R, Paynter N. Cancer risk assessment from family history: gaps in primary care practice. J Fam Pract. 2002;51:856. [PubMed] |
| 24. | Emery J, Rose P. Expanding the role of the family history in primary care. Br J Gen Pract. 1999;49:260-261. [PubMed] |
| 25. | Smith RA, von Eschenbach AC, Wender R, Levin B, Byers T, Rothenberger D, Brooks D, Creasman W, Cohen C, Runowicz C. American Cancer Society guidelines for the early detection of cancer: update of early detection guidelines for prostate, colorectal, and endometrial cancers. Also: update 2001--testing for early lung cancer detection. CA Cancer J Clin. 2001;51:38-75; quiz 77-80. [PubMed] |
| 26. | Murff HJ, Greevy RA, Syngal S. The comprehensiveness of family cancer history assessments in primary care. Community Genet. 2007;10:174-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 27. | Qureshi N, Wilson B, Santaguida P, Carroll J, Allanson J, Culebro CR, Brouwers M, Raina P. Collection and use of cancer family history in primary care. Evid Rep Technol Assess (Full Rep). 2007;1-84. [PubMed] |
| 28. | Armelao F, Orlandi PG, Tasini E, Franceschini G, Franch R, Paternolli C, de Pretis G. High uptake of colonoscopy in first-degree relatives of patients with colorectal cancer in a healthcare region: a population-based, prospective study. Endoscopy. 2010;42:15-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Menges M, Fischinger J, Gärtner B, Georg T, Woerdehoff D, Maier M, Harloff M, Stegmaier C, Raedle J, Zeitz M. Screening colonoscopy in 40- to 50-year-old first-degree relatives of patients with colorectal cancer is efficient: a controlled multicentre study. Int J Colorectal Dis. 2006;21:301-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Hlavaty T, Lukac L, Huorka M, Bezayova T, Duris I. Positive family history promotes participation in colorectal cancer screening. Bratisl Lek Listy. 2005;106:318-323. [PubMed] |
| 31. | Barnett ML, Song Z, Landon BE. Trends in physician referrals in the United States, 1999-2009. Arch Intern Med. 2012;172:163-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 182] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 32. | Cook NL, Hicks LS, O’Malley AJ, Keegan T, Guadagnoli E, Landon BE. Access to specialty care and medical services in community health centers. Health Aff (Millwood). 2007;26:1459-1468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 204] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 33. | Felt-Lisk S, McHugh M, Thomas M; Examining Access to Specialty Care for California's Uninsured: Full report. June 2004. Available from: http://www.cpca.org/index.cfm/health-center-resources/clinical-quality-improvement/specialty-care/. |
| 34. | Hollingsworth JM, Saint S, Hayward RA, Rogers MA, Zhang L, Miller DC. Specialty care and the patient-centered medical home. Med Care. 2011;49:4-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 35. | Chen AH, Murphy EJ, Yee HF. eReferral--a new model for integrated care. N Engl J Med. 2013;368:2450-2453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 127] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 36. | Forrest CB. A typology of specialists’ clinical roles. Arch Intern Med. 2009;169:1062-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 77] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 37. | Marinopoulos SS, Dorman T, Ratanawongsa N, Wilson LM, Ashar BH, Magaziner JL, Miller RG, Thomas PA, Prokopowicz GP, Qayyum R. Effectiveness of continuing medical education. Evid Rep Technol Assess (Full Rep). 2007;1-69. [PubMed] |
| 38. | Mahnke CB, Jordan CP, Bergvall E, Person DA, Pinsker JE. The Pacific Asynchronous TeleHealth (PATH) system: review of 1,000 pediatric teleconsultations. Telemed J E Health. 2011;17:35-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 39. | Jones C, Roderick P, Harris S, Rogerson M. An evaluation of a shared primary and secondary care nephrology service for managing patients with moderate to advanced CKD. Am J Kidney Dis. 2006;47:103-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 40. | Burkey Y, Black M, Reeve H. Patients’ views on their discharge from follow up in outpatient clinics: qualitative study. BMJ. 1997;315:1138-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 41. | Brez S, Rowan M, Malcolm J, Izzi S, Maranger J, Liddy C, Keely E, Ooi TC. Transition from specialist to primary diabetes care: a qualitative study of perspectives of primary care physicians. BMC Fam Pract. 2009;10:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 42. | Gandhi TK, Sittig DF, Franklin M, Sussman AJ, Fairchild DG, Bates DW. Communication breakdown in the outpatient referral process. J Gen Intern Med. 2000;15:626-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 225] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 43. | O’Malley AS, Reschovsky JD. Referral and consultation communication between primary care and specialist physicians: finding common ground. Arch Intern Med. 2011;171:56-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 158] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 44. | Chen AH, Kushel MB, Grumbach K, Yee HF. Practice profile. A safety-net system gains efficiencies through ‘eReferrals’ to specialists. Health Aff (Millwood). 2010;29:969-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 45. | Kim-Hwang JE, Chen AH, Bell DS, Guzman D, Yee HF, Kushel MB. Evaluating electronic referrals for specialty care at a public hospital. J Gen Intern Med. 2010;25:1123-1128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 88] [Article Influence: 5.9] [Reference Citation Analysis (0)] |