Published online Dec 21, 2015. doi: 10.3748/wjg.v21.i47.13352
Peer-review started: February 24, 2015
First decision: March 26, 2015
Revised: April 13, 2015
Accepted: September 30, 2015
Article in press: September 30, 2015
Published online: December 21, 2015
Processing time: 295 Days and 5.4 Hours
AIM: To clarify the pathogenesis of gastroesophageal reflux disease symptoms in non-erosive reflux disease (NERD) patients.
METHODS: Thirty-five NERD patients with persistent symptoms, despite taking rabeprazole 10 mg twice daily for at least 8 wk, were included in this study. All patients underwent 24 h combined impedance - pH on rabeprazole. The symptom index (SI) was considered to be positive if ≥ 50%, and proximal reflux episodes were determined when reflux reached 15 cm above the proximal margin of the lower esophageal sphincter.
RESULTS: In 14 (40%) SI-positive patients, with liquid weakly acid reflux, the occurrence rate of reflux symptoms was significantly more frequent in proximal reflux episodes (46.7%) than in distal ones (5.7%) (P < 0.001). With liquid acid reflux, there were no significant differences in the occurrence rate of reflux symptoms between proximal reflux episodes (38.5%) and distal ones (20.5%) (NS). With mixed liquid-gas weakly acid reflux, the occurrence rate of reflux symptoms in proximal reflux episodes was significantly more frequent (31.0%) than in distal reflux ones (3.3%) (P < 0.001). With mixed liquid-gas acid reflux, there were no significant differences in the occurrence rate of reflux symptoms between proximal reflux episodes (29.4%) and distal ones (14.3%) (NS).
CONCLUSION: The proximal extent of weakly acidic liquid and mixed liquid-gas reflux is a major factor associated with reflux perception in SI-positive patients on proton pump inhibitor therapy.
Core tip: Thirty-five non-erosive reflux disease patients with persistent symptoms, despite taking rabeprazole 10 mg twice daily, were included. In 14 (40%) symptom index (SI)-positive patients, with liquid weakly acid reflux, the occurrence rate of reflux symptoms in proximal reflux episodes was significantly more frequent (46.7%) than in distal ones (5.7%) (P < 0.001). With mixed liquid-gas weakly acid reflux, the occurrence rate of reflux symptoms in proximal reflux episodes was significantly more frequent (31.0%) than in distal reflux ones (3.3%) (P < 0.001). The proximal extent of weakly acidic liquid and mixed liquid-gas reflux is a major factor of reflux perception in SI-positive patients on proton pump inhibitor (PPI).
- Citation: Nakagawa K, Koike T, Iijima K, Saito M, Kikuchi H, Hatta W, Ara N, Uno K, Asano N, Shimosegawa T. Characteristics of symptomatic reflux episodes in Japanese proton pump inhibitor-refractory non-erosive reflux disease patients. World J Gastroenterol 2015; 21(47): 13352-13359
- URL: https://www.wjgnet.com/1007-9327/full/v21/i47/13352.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i47.13352
The reflux of gastric juice containing acid, bile, and pepsin into the esophagus is a causal factor of gastroesophageal reflux disease (GERD). It was reported that the incidence of GERD has increased significantly in each of the last two decades in Western countries[1]. The incidence of GERD is also increasing in Japan as well[2] because of the decreasing prevalence of Helicobacter pylori (H. pylori) infection and the Westernization of the diet in recent decades.
Proton pump inhibitors (PPIs) are commonly used as the first-line treatment because of their high effectiveness and prolonged duration in suppressing of gastric acid secretion. Several studies have demonstrated that non-erosive reflux disease (NERD) patients are less sensitive to PPI treatment than patients with erosive reflux disease (ERD)[3-5]. Patients with NERD are hypersensitive to visceral stimulation, which is characterized by a reduced pain threshold to experimental stimulation[6,7].
With a combined pH and multiple intraluminal impedance (MII-pH) technique that can detect GERD irrespective of acidity, reflux with a nadir pH between 4 and 7 (weakly acidic reflux) and with a nadir pH above 7 (alkaline reflux) can be detected[8]. In Western countries, several studies have reported using MII-pH monitoring in GERD patients[9-11], but the pathogenesis of heartburn and acid regurgitation has not yet been fully elucidated in PPI-refractory NERD patients on PPI.
Few studies have evaluated the association between reflux symptoms and reflux episodes, and reflux episodes that are liquid reflux and mixed liquid-gas reflux in PPI-refractory NERD patients on PPI. Therefore, the aim of this study was to clarify reflux episodes, the occurrence of reflux symptoms, and the pH values at each impedance site by classifying them into acid reflux and weakly acid reflux.
From August 2011 to April 2014, 35 consecutive NERD patients [14 men; median age, 65 (21-76) years] with persistent symptoms suggestive of gastro-esophageal reflux despite taking rabeprazole 10 mg twice daily for at least 8 wk were included in this study. Patients with troublesome GERD symptoms in the absence of visible esophageal mucosal injury at endoscopy without taking off PPI were defined as NERD. In fact, patients’ symptoms were assessed using a questionnaire for the diagnosis of reflux disease, the frequency scale for symptoms of gastro-esophageal reflux disease (FSSG)[12]. PPI-refractory NERD patients were so defined if their FSSG scores were higher than 8, and they had persistently troublesome GERD symptoms, such as heartburn or regurgitation, even while taking a double dose of PPI (rabeprazole, 10 mg bid) for at least 8 wk. All PPI-refractory NERD patients were administered 24 h combined MII-pH on PPI. “Heavy alcohol use” was defined as consuming more than 75 mL ethanol per day.
Subjects with peptic ulcer disease, malignant disease, a history of previous esophagogastric surgery, or who had taken antibiotics and prokinetic drugs prior to the endoscopic examination were excluded from the analysis. This study was approved by the Tohoku University Hospital Ethics Committee. Informed consent was obtained from all subjects, and the study was conducted according to the provisions of the Declaration of the Helsinki. No complications occurred in any patients during this study.
All patients underwent esophagogastroduodenoscopy. Hiatus hernia was diagnosed when the distance between the esophagogastric junction and the diaphragmatic hiatus was ≥ 2 cm. Gastric atrophy was endoscopically assessed by the pattern system described by Kimura and Takemoto[13]. The extent of atrophy was classified as either closed or open according to their classification. The closed type is defined as having an atrophic border restricted to the lesser curvature of the stomach, whereas the open type is when the atrophic border is absent on the lesser curvature but extends along the anterior and posterior walls of the stomach. In this study, “Gastric atrophy” was defined as the open type.
Serum IgG antibodies against H. pylori were measured by enzyme linked immunosorbent assay using an EIA kit (E Plate “Eiken”H. pylori-antibody, Eiken Chemical Co. Ltd., Tokyo, Japan). Patients were considered to be infected with H. pylori if their serum test values were greater than 9.90 U/mL.
The data of intraluminal electrical impedance were recorded with a 2.1 mm in diameter polyvinyl assembly containing a series of cylindrical electrodes spaced at 2 cm intervals (ConforTec MII/pH, Sandhill Scientific, Highland Ranch, CO, United States). Each pair of electrodes formed a measuring segment corresponding to one recording channel (Sandhill Scientific, Highland Ranch, CO, United States). The signals from six impedance channels and two pH channels were recorded at 50 samples per second.
The data were stored in a portable recorder and saved on a 256 Mb Compact Flash card (San Disk, Milpitas, CA, United States). The esophageal pH level and gastric pH level were measured using an antimony pH electrode. pH electrodes were calibrated using pH 4.0 and pH 7.0 buffer solutions before beginning the recording.
Patients were studied after an overnight fast of at least 10 h. After stationary esophageal manometry to locate the lower esophageal sphincter (LES), the pH- MII was passed through the nose under topical anesthesia and positioned with the pH electrodes at 5 cm above the proximal border of the LES and 10 cm below the LES. In this position, impedance was measured at 3, 5, 7, 9, 15, and 17 cm proximal to the LES. Once the desired location was achieved, the catheter was taped to the patient’ s nose and connected to a recording device on the patient’ s belt, and the impedance and pH data were recorded and stored. Patients were encouraged to maintain normal activity, sleep schedules, and usual meals at regular times. Subjects were in the upright position as much as possible during the daytime and were allowed free movement and one recumbent period. All subjects had three usual meals at regular times without between-meal eating during the measurement period. All events during testing, including meals, symptoms, and body position (upright/recumbent), were entered by the patient directly into the monitor. Portable MII-pH monitoring was performed over 24 h, after which patients returned to the testing laboratory for catheter removal.
The data stored on the Compact Flash card were downloaded onto a personal computer and visually analyzed with the assistance of dedicated software, Bioview analysis version 5.4.3 (Sandhill Scientific). Each recording was manually reviewed, edited, and analyzed independently by two authors (K.N. and T.K.). Discordant readings were reviewed until consensus was reached. Reflux episodes were classified according to previously described criteria[14]. Liquid reflux was defined as a retrograde 50% drop in impedance starting distally (above the LES) and propagating at least to the next two more proximal impedance measuring segments. Gas reflux was defined as a rapid (3000 Ω/s) increase in impedance, occurring simultaneously in at least two esophageal measuring segments, in the absence of swallowing. Mixed liquid-gas reflux was defined as gas reflux occurring immediately before or during a liquid reflux. Reflux episodes consisting of only gaseous reflux, which appears as a simultaneous increase in impedance > 3000 Ω, in any two consecutive sites were excluded from the study. Reflux events were divided into three subcategories based on the pH level at the point of reflux: acid reflux (reflux episodes that reduced the pH of the esophagus to below 4 or that occurred when the esophageal pH was already below 4), weakly acid reflux (an impedance-detected reflux event occurring when the esophageal pH was between 4 < pH < 7), and weakly alkaline reflux (a reflux episode during which the pH did not drop below 7)[8]. The numbers and duration of total reflux events, acid reflux, and weakly acid reflux were analyzed, whereas meal periods (three periods of about 20 min each) were excluded from the analysis. A reflux episode was considered to be proximal reflux if the impedance indicated liquid and mixed liquid-gas reflux at 15 cm above the LES, and distal reflux if reflux was below that level.
Symptoms were considered to be associated with reflux if reflux episodes were detected 5 min prior to the symptom occurring. The symptom index (SI) was calculated for each patient in relation to liquid reflux and mixed liquid-gas reflux. SI was defined as the ratio of the number of symptoms related to the reflux to the total number of symptoms[15]. The relationship between reflux symptoms and reflux episodes was analyzed only in SI positive patients.
Pathological acid reflux is present when the intra-esophageal pH is below 4 for greater than 4.2% of the time[16].
Parametric data were expressed as mean ± standard deviation (SD) and non-parametric data as median (interquartile range). The frequencies of different impedance/pH patterns of reflux in each group were analyzed and compared using Mann - Whitney U -test. Correlations among intragastric pH levels and the numbers of total reflux events, acid reflux, and non-acid reflux, were analyzed by Spearman’s rank correlation. Fisher’s exact test was used to compare the categorical variables in the clinicopathological features between SI positive and negative. A P value of < 0.05 was considered to be significant. Analyses were carried out using SPSS software (version 11.0; Chicago, IL, United States).
Comparisons of related parameters between the SI-positive group and the SI-negative group are shown in Table 1. Of the 35 NERD patients, 14 (40.0%) were SI-positive, and 21 (60.0%) were SI-negative. There were no significant differences in gender, heavy alcohol use, current smokers, body mass index, presence of esophageal hiatus hernia, gastric atrophy, or prevalence of H. pylori infection. The mean FSSG score of the SI-negative group (23.1 ± 9.0) was significantly higher than that of the SI-positive group (16.7 ± 8.7) (P = 0.0437). Five patients (three patients with SI positive and two patients with SI negative) had abnormal esophageal acid exposure times.
| SI positive | SI negative | P value | |
| No. patients | 14 (40.0) | 21 (60.0) | NS1 |
| Age (SD) | 61.9 (12.3) | 59.3 (15.6) | NS1 |
| Gender (male/female) | 6/8 | 7/14 | NS2 |
| Heavy drinker | 3 (21.4) | 4 (19.0) | NS2 |
| Current smoker | 2 (14.3) | 1 (4.8) | NS2 |
| BMI | 21.1 (2.1) | 21.0 (2.3) | NS2 |
| Hiatus hernia | 3 (21.4) | 8 (38.1) | NS2 |
| Helicobacter pylori | 4 (28.5) | 6 (28.6) | NS2 |
| Gastric atrophy | 6 (42.9) | 7 (33.3) | NS2 |
| FSSG score (SD) | 16.7 (8.7) | 23.1 (9.0) | 0.04373 |
In the 14 patients with a positive SI, 589 liquid and mixed liquid-gas reflux episodes were recorded. Amongst these, 94 (16.0%) were acid reflux, 477 (80.9%) were weakly acidic reflux, and 18 (3.1%) were weakly alkaline reflux.
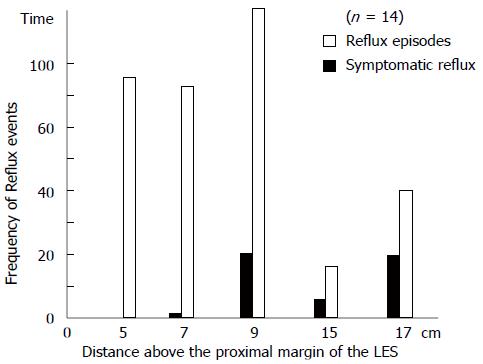
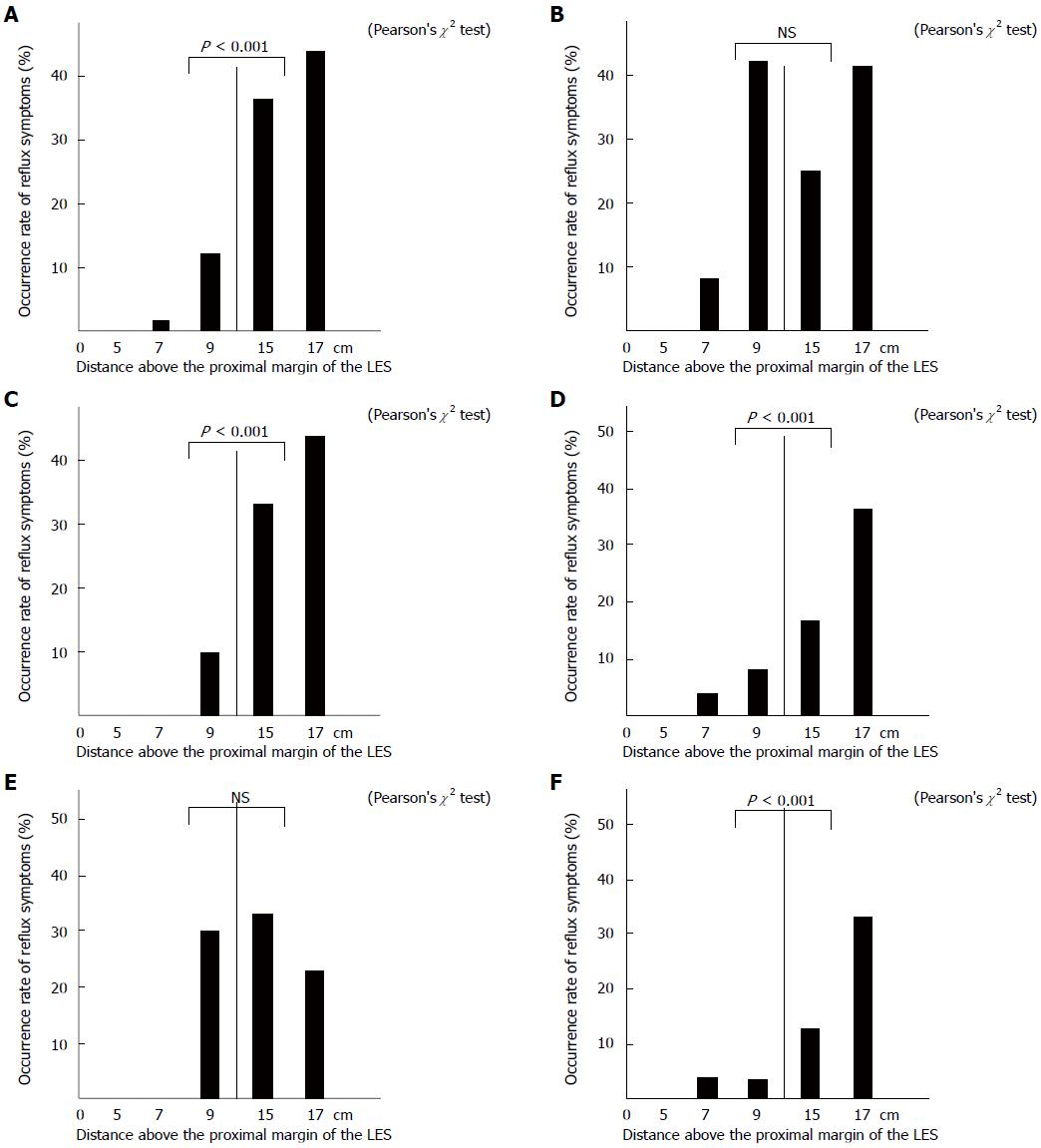
In the SI-positive patients, a total of 383 liquid reflux episodes with acid reflux and weakly acid reflux were detected. Overall, 51 (13.3%) reflux episodes were symptomatic, including 14 (27.5%) acid and 37 (72.5%) weakly acidic. The total reflux episodes and symptoms above the proximal margin of the LES at each impedance site are shown in Figure 1. The 325 distal reflux episodes were significantly more frequent (84.9%) than the 58 proximal ones (15.1%) (P < 0.001). The occurrence rate of reflux symptoms above the proximal margin of the LES at each impedance site is shown in Figure 2A. The occurrence rate of reflux symptoms in proximal reflux episodes was significantly more frequent (44.8%) than in distal ones (7.7%) (P < 0.001). With liquid acid reflux, there were no significant differences in the occurrence rate of reflux symptoms between proximal reflux episodes (38.5%) and distal ones (20.5%) (NS) (Figure 2B). On the other hand, with liquid weakly acid reflux, the occurrence rate of reflux symptoms in proximal reflux episodes was significantly more frequent (46.7%) than in distal ones (5.7%) (P < 0.001) (Figure 2C).
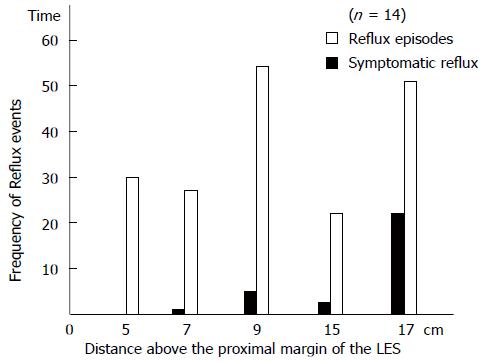
A total of 188 mixed liquid-gas reflux episodes with acid reflux and weakly acidic were detected, and 29 (15.4%) were symptomatic. The total reflux episodes and symptoms above the proximal margin of the LES at each impedance site are shown in Figure 3. Distal reflux episodes were significantly more frequent (60.1%) than proximal reflux ones (39.9%) (P = 0.0047). The occurrence rate of reflux symptoms above the proximal margin of the LES at each impedance site is shown in Figure 2D. The occurrence rate of reflux symptoms in proximal reflux episodes was significantly more frequent (30.7%) than in distal ones (5.3%) (P < 0.001). In addition, when classifying acid reflux and weakly acid reflux, as simply acid reflux, there were no significant differences in the occurrence rate of reflux symptoms between proximal reflux episodes (29.4%) and distal ones (14.3%) (NS) (Figure 2E). On the other hand, with weakly acid reflux, the occurrence rate of reflux symptoms in proximal reflux episodes was significantly more frequent (31.0%) than in distal ones (3.3%) (P < 0.001) (Figure 2F).
In Western countries, 20 mg of rabeprazole is the standard dose for GERD patients, whereas in Japan, 20 mg rabeprazole is used as a double dose PPI therapy for such patients. Therefore, patients with persistent symptoms despite using 20 mg rabeprazole were considered to be PPI-refractory NERD patients in Japan.
In this study, the relationship between reflux symptoms and reflux episodes were analyzed only in SI positive patients. SI negative patients did not show a relationship between reflux symptoms and reflux episodes because they were not analyzed.
Of the 35 NERD patients, 14 (40.0%) were SI-positive and 21 (60.0%) were SI-negative. SI-negative is characterized by functional heartburn (FH), which is generally defined according to the Rome III criteria as the presence of reflux symptoms with no evidence of symptomatic reflux by MII-pH monitoring[17].
The FSSG score, which is widely used for the diagnosis of GERD in Japan, assesses the 12 symptoms that Japanese patients with GERD complain of most often, not only heartburn but also dyspeptic symptoms, such as “heavy stomach” and “feeling full quickly”[12,18,19]. In the present study, the FSSG score in the SI-negative group was significantly higher than that in the SI-positive group because patients with FH had a tendency to be more sensitive both to heartburn and dyspeptic symptoms than those who were SI positive.
In our study, 94 of total reflux episodes (16.0%) were acid reflux, 477 (80.9%) were weakly acidic reflux, and 18 (3.1%) were weakly alkaline reflux. Therefore, weakly acid reflux is a major factor in the reflux symptoms of SI positive patients with NERD, despite taking a double-dose of PPI. These results are similar to previous results reported from Western countries[20,21] and Japan[22,23].
A previous study suggested that the level of reflux might play an important role in the symptoms of GERD, including NERD patients[10,20-23]. In Western countries, it has been reported that a high proximal extent of the refluxate is an important factor associated with reflux perception in patients with GERD off-PPI therapy[10,13] and on-PPI therapy[24,25]. In Japan, it was reported that proximal liquid migration was associated with symptomatic reflux in PPI-refractory NERD patients[22,23]. However, few studies have evaluated in Japan the relationship between reflux symptoms and reflux episodes by comparing liquid reflux and mixed liquid-gas reflux in PPI-refractory NERD. In addition, few studies have classified reflux episodes and the occurrence of reflux symptoms at each impedance site into acid reflux and weakly acid reflux.
In our study, with liquid reflux, the occurrence rate of reflux symptoms in the proximal reflux episodes was significantly more frequent (44.8%) than in distal ones (7.7%). With liquid weakly acid reflux, the occurrence rate of reflux symptoms in proximal reflux episodes was significantly more frequent (46.7%) than in distal ones (5.7%). With mixed liquid-gas weakly acid reflux, the occurrence rate of reflux symptoms in proximal reflux episodes was significantly more frequent (31.0%) than in distal ones (3.3%). As supported by previous studies, the proximal extent of reflux with liquid weakly acid reflux is a major factor in the perception of reflux[22,23]. The etiology of the association between the symptoms and the proximal extent of gastroesophageal reflux still remains to be fully elucidated. In a previous study, a secondary mechanical hyperalgesia of the proximal esophagus (not exposed to acid) was demonstrated following acid perfusion of the distal esophagus[26]. Additionally, dilation of the intercellular spaces of the esophageal epithelium, first demonstrated in the distal esophagus and proposed as a mechanism of reflux perception in NERD, has since been demonstrated in the proximal esophagus by Caviglia et al[27]. Additionally, the proximal esophagus might have a larger number of mechanoreceptors than the distal esophagus as a result of dilatation of the intercellular spaces of the epithelium[28]. In NERD patients, the presence of gas in the refluxate significantly enhances the probability of reflux perception[13]. Concerning mixed liquid-gas reflux, clarification of these mechanisms could be useful. However, with liquid acid reflux, there were no significant differences in the occurrence rate of reflux symptoms between proximal reflux episodes (38.5%) and distal ones (20.5%). With mixed liquid-gas acid reflux, there were no significant differences in the occurrence rate of reflux symptoms between proximal reflux episodes (29.4%) and distal ones (14.3%). The occurrence rate of reflux symptoms was more frequent in the proximal esophagus with weakly acid reflux, although it was more frequent in distal esophagus as well as proximal esophagus with acid reflux. Therefore, acid reflux is an important factor even in distal esophageal reflux in PPI-refractory NERD patients. Acid reflux causes macroscopic damage to the esophageal wall, which is a stimulating factor that contributes to the reflux symptoms[29]. Even if the proportion of acid reflux is less than that of weakly acid reflux, acid reflux is one of the important factors in the perception of reflux with insufficient acid suppressive therapy in NERD patients.
In this study, the subjects did not have standardized meals during the measurement period because we wanted to evaluate reflux conditions in their usual daily activity.
Reflux episodes consisting of gas reflux events without liquid (belches) and weakly alkaline were not considered for the purpose of this study. We did not include the relationship between gas-only reflux episodes and symptoms because of differences in the mechanisms and therapeutic approaches for liquid-containing and gas-only reflux episodes. Furthermore, the frequency of symptomatic pure gas reflux and weakly alkaline was very low and, therefore, not further analyzed.
In conclusion, the proximal extent of weakly acidic liquid and mixed liquid-gas reflux are major factors associated with reflux perception in SI-positive patients on PPI therapy. In acid reflux that includes gas, reflux to the distal esophagus is associated with reflux perception in SI-positive patients with PPI-refractory NERD.
The pathogenesis of heartburn and acid regurgitation in non-erosive reflux disease (NERD) patients still remains to be fully elucidated.
Several studies have demonstrated that NERD patients are less sensitive to proton pump inhibitor (PPI) treatment than patients with erosive reflux disease. With a combined pH and multiple intraluminal impedance (MII-pH) technique that can detect gastroesophageal reflux disease (GERD) irrespective of acidity, reflux with a nadir pH between 4 and 7 (weakly acidic reflux) and with a nadir pH above 7 (alkaline reflux) can also be detected.
In Western countries, several studies have reported using MII-pH monitoring in GERD patients, but the pathogenesis of heartburn and acid regurgitation has not yet been fully elucidated in PPI-refractory NERD patients on PPI. Few studies have evaluated the association between reflux symptoms and reflux episodes, and reflux episodes that are liquid reflux and mixed liquid-gas reflux in these patients. The proximal extent of weakly acidic liquid and mixed liquid-gas reflux is a major factor associated with reflux perception in symptom index (SI)-positive patients on PPI therapy.
The proximal extent of weakly acidic liquid and mixed liquid-gas reflux is a major factor associated with reflux perception in SI-positive patients on PPI therapy. Additionally, with acid reflux that includes gas, reflux to the distal esophagus is associated with reflux perception in SI-positive patients with PPI-refractory NERD.
PPIs are commonly used as the first-line treatment because of their high effectiveness and prolonged duration in suppressing gastric acid secretion. Several studies have demonstrated that NERD patients are less sensitive to PPI treatment than patients with erosive reflux disease. Patients with NERD are hypersensitive to visceral stimulation, which is characterized by a reduced pain threshold to experimental stimulation. With a combined MII-pH technique that can detect GERD irrespective of acidity, reflux with a nadir pH between 4 and 7 (weakly acidic reflux) and with a nadir pH above 7 (alkaline reflux) can also be detected. The SI was calculated for each patient in relation to liquid reflux and mixed liquid-gas reflux. SI was defined as the ratio of the number of symptoms related to the reflux to the total number of symptoms.
This is an interesting and carefully conducted study, which sheds some light into the nature of NERD. The aim of this study was to clarify reflux episodes, the occurrence of reflux symptoms, and the pH values at each impedance site by classifying them into acid reflux and weakly acid reflux. The authors concluded that the proximal extent of weakly acidic liquid and mixed liquid-gas reflux is a major factor associated with reflux perception in SI-positive patients on PPI therapy.
P- Reviewer: Slomiany BL S- Editor: Qi Y L- Editor: Filipodia E- Editor: Zhang DN
| 1. | El-Serag HB. Time trends of gastroesophageal reflux disease: a systematic review. Clin Gastroenterol Hepatol. 2007;5:17-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 305] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 2. | Fujiwara Y, Arakawa T. Epidemiology and clinical characteristics of GERD in the Japanese population. J Gastroenterol. 2009;44:518-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 247] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 3. | Tew S, Jamieson GG, Pilowsky I, Myers J. The illness behavior of patients with gastroesophageal reflux disease with and without endoscopic esophagitis. Dis Esophagus. 1997;10:9-15. [PubMed] |
| 4. | Lind T, Havelund T, Carlsson R, Anker-Hansen O, Glise H, Hernqvist H, Junghard O, Lauritsen K, Lundell L, Pedersen SA. Heartburn without oesophagitis: efficacy of omeprazole therapy and features determining therapeutic response. Scand J Gastroenterol. 1997;32:974-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 275] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 5. | Richter JE, Kovacs TO, Greski-Rose PA, Huang section sign B, Fisher R. Lansoprazole in the treatment of heartburn in patients without erosive oesophagitis. Aliment Pharmacol Ther. 1999;13:795-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 56] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Trimble KC, Pryde A, Heading RC. Lowered oesophageal sensory thresholds in patients with symptomatic but not excess gastro-oesophageal reflux: evidence for a spectrum of visceral sensitivity in GORD. Gut. 1995;37:7-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 195] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 7. | Rodriguez-Stanley S, Robinson M, Earnest DL, Greenwood-Van Meerveld B, Miner PB. Esophageal hypersensitivity may be a major cause of heartburn. Am J Gastroenterol. 1999;94:628-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 80] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Sifrim D, Castell D, Dent J, Kahrilas PJ. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut. 2004;53:1024-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 620] [Cited by in RCA: 604] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 9. | Vela MF, Camacho-Lobato L, Srinivasan R, Tutuian R, Katz PO, Castell DO. Simultaneous intraesophageal impedance and pH measurement of acid and nonacid gastroesophageal reflux: effect of omeprazole. Gastroenterology. 2001;120:1599-1606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 434] [Cited by in RCA: 424] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 10. | Bredenoord AJ, Weusten BL, Curvers WL, Timmer R, Smout AJ. Determinants of perception of heartburn and regurgitation. Gut. 2006;55:313-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 212] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 11. | Sifrim D, Holloway R, Silny J, Xin Z, Tack J, Lerut A, Janssens J. Acid, nonacid, and gas reflux in patients with gastroesophageal reflux disease during ambulatory 24-hour pH-impedance recordings. Gastroenterology. 2001;120:1588-1598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 270] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 12. | Kusano M, Shimoyama Y, Sugimoto S, Kawamura O, Maeda M, Minashi K, Kuribayashi S, Higuchi T, Zai H, Ino K. Development and evaluation of FSSG: frequency scale for the symptoms of GERD. J Gastroenterol. 2004;39:888-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 356] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 13. | Kimura K, Takemoto T. An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy. 1969;3:87-97. [RCA] [DOI] [Full Text] [Cited by in Crossref: 612] [Cited by in RCA: 314] [Article Influence: 18.5] [Reference Citation Analysis (3)] |
| 14. | Emerenziani S, Sifrim D, Habib FI, Ribolsi M, Guarino MP, Rizzi M, Caviglia R, Petitti T, Cicala M. Presence of gas in the refluxate enhances reflux perception in non-erosive patients with physiological acid exposure of the oesophagus. Gut. 2008;57:443-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 77] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 15. | Wiener GJ, Richter JE, Copper JB, Wu WC, Castell DO. The symptom index: a clinically important parameter of ambulatory 24-hour esophageal pH monitoring. Am J Gastroenterol. 1988;83:358-361. [PubMed] |
| 16. | Johnson LF, Demeester TR. Twenty-four-hour pH monitoring of the distal esophagus. A quantitative measure of gastroesophageal reflux. Am J Gastroenterol. 1974;62:325-332. [PubMed] |
| 17. | Galmiche JP, Clouse RE, Bálint A, Cook IJ, Kahrilas PJ, Paterson WG, Smout AJ. Functional esophageal disorders. Gastroenterology. 2006;130:1459-1465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 317] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 18. | Shimoyama Y, Kusano M, Sugimoto S, Kawamura O, Maeda M, Minashi K, Kuribayashi S, Higuchi T, Zai H, Ino K. Diagnosis of gastroesophageal reflux disease using a new questionnaire. J Gastroenterol Hepatol. 2005;20:643-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Kusano M, Shimoyama Y, Kawamura O, Maeda M, Kuribayashi S, Nagoshi A, Zai H, Moki F, Horikoshi T, Toki M. Proton pump inhibitors improve acid-related dyspepsia in gastroesophageal reflux disease patients. Dig Dis Sci. 2007;52:1673-1677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Savarino E, Zentilin P, Tutuian R, Pohl D, Gemignani L, Malesci A, Savarino V. Impedance-pH reflux patterns can differentiate non-erosive reflux disease from functional heartburn patients. J Gastroenterol. 2012;47:159-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 93] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 21. | Mainie I, Tutuian R, Shay S, Vela M, Zhang X, Sifrim D, Castell DO. Acid and non-acid reflux in patients with persistent symptoms despite acid suppressive therapy: a multicentre study using combined ambulatory impedance-pH monitoring. Gut. 2006;55:1398-1402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 472] [Cited by in RCA: 458] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 22. | Kohata Y, Fujiwara Y, Machida H, Okazaki H, Yamagami H, Tanigawa T, Watanabe K, Watanabe T, Tominaga K, Arakawa T. Pathogenesis of proton-pump inhibitor-refractory non-erosive reflux disease according to multichannel intraluminal impedance-pH monitoring. J Gastroenterol Hepatol. 2012;27 Suppl 3:58-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | Iwakiri K, Sano H, Tanaka Y, Kawami N, Umezawa M, Futagami S, Hoshihara Y, Nomura T, Miyashita M, Sakamoto C. Characteristics of symptomatic reflux episodes in patients with non-erosive reflux disease who have a positive symptom index on proton pump inhibitor therapy. Digestion. 2010;82:156-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Zerbib F, Duriez A, Roman S, Capdepont M, Mion F. Determinants of gastro-oesophageal reflux perception in patients with persistent symptoms despite proton pump inhibitors. Gut. 2008;57:156-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 134] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 25. | Tutuian R, Vela MF, Hill EG, Mainie I, Agrawal A, Castell DO. Characteristics of symptomatic reflux episodes on Acid suppressive therapy. Am J Gastroenterol. 2008;103:1090-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 123] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 26. | Sarkar S, Hobson AR, Furlong PL, Woolf CJ, Thompson DG, Aziz Q. Central neural mechanisms mediating human visceral hypersensitivity. Am J Physiol Gastrointest Liver Physiol. 2001;281:G1196-G1202. [PubMed] |
| 27. | Caviglia R, Ribolsi M, Gentile M, Rabitti C, Emerenziani S, Guarino MP, Petitti T, Cicala M. Dilated intercellular spaces and acid reflux at the distal and proximal oesophagus in patients with non-erosive gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2007;25:629-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 89] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 28. | Cicala M, Habib FI, Emerenziani S. Proximal oesophagus: the added value in understanding GORD symptoms. Neurogastroenterol Motil. 2009;21:790-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Tobey NA, Carson JL, Alkiek RA, Orlando RC. Dilated intercellular spaces: a morphological feature of acid reflux--damaged human esophageal epithelium. Gastroenterology. 1996;111:1200-1205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 328] [Article Influence: 11.3] [Reference Citation Analysis (0)] |