Published online Dec 7, 2015. doi: 10.3748/wjg.v21.i45.12970
Peer-review started: April 15, 2015
First decision: May 18, 2015
Revised: May 25, 2015
Accepted: August 31, 2015
Article in press: August 31, 2015
Published online: December 7, 2015
Processing time: 237 Days and 3 Hours
Superior mesenteric artery (SMA) syndrome is defined as a compression of the third portion of the duodenum by the abdominal aorta and the overlying SMA. SMA syndrome associated with anorexia nervosa has been recognized, mainly among young female patients. The excessive weight loss owing to the eating disorder sometimes results in a reduced aorto-mesenteric angle and causes duodenal obstruction. Conservative treatment, including psychiatric and nutritional management, is recommended as initial therapy. If conservative treatment fails, surgery is often required. Currently, traditional open bypass surgery has been replaced by laparoscopic duodenojejunostomy as a curative surgical approach. However, single incision laparoscopic approach is rarely performed. A 20-year-old female patient with a diagnosis of anorexia nervosa and SMA syndrome was prepared for surgery after failed conservative management. As the patient had body image concerns, a single incision laparoscopic duodenojejunostomy was performed to achieve minimal scarring. As a result, good perioperative outcomes and cosmetic results were achieved. We show the first case of a young patient with SMA syndrome who was successfully treated by single incision laparoscopic duodenojejunostomy. This minimal invasive surgery would be beneficial for other patients with SMA syndrome associated with anorexia nervosa, in terms of both surgical and cosmetic outcomes.
Core tip: Traditional open bypass surgery has been replaced by laparoscopic duodenojejunostomy as a curative surgical approach for superior mesenteric artery (SMA) syndrome. However, the single incision laparoscopic approach is rarely performed. Here, we show our experience of single incision laparoscopic duodenojejunostomy in a 20-year-old woman with anorexia nervosa and SMA syndrome. As both diseases are commonly seen in young women with body image concerns, the cosmetic outcome of surgery should be taken into consideration. We believe that this minimally invasive surgery is beneficial for patients with SMA syndrome associated with body image concerns, in terms of both surgical and cosmetic outcomes.
- Citation: Yao SY, Mikami R, Mikami S. Minimally invasive surgery for superior mesenteric artery syndrome: A case report. World J Gastroenterol 2015; 21(45): 12970-12975
- URL: https://www.wjgnet.com/1007-9327/full/v21/i45/12970.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i45.12970
Superior mesenteric artery (SMA) syndrome is defined as a compression of the third portion of the duodenum by the abdominal aorta and the overlying superior mesenteric artery. The narrow aortomesenteric angle results in chronic, intermittent, or acute complete or partial duodenal obstruction. Patients often present with nausea, vomiting, abdominal distention, decreased appetite, and weight loss[1]. Non-surgical treatment is recommended as initial therapy, but when conservative treatment fails, surgery is often required. After the first successful laparoscopic duodenojejunostomy by Gersin et al[2] in 1998, the procedure became the most common surgical treatment[3].
Among these patients, eating disorder such as anorexia nervosa (AN) may coexist as an underlying pathology[4]. We describe here a young female patient with SMA syndrome successfully treated by single incision laparoscopic duodenojejunostomy. Because this patient had body image concerns associated with AN, single incision laparoscopic surgery (SILS) was selected as a “scarless” method.
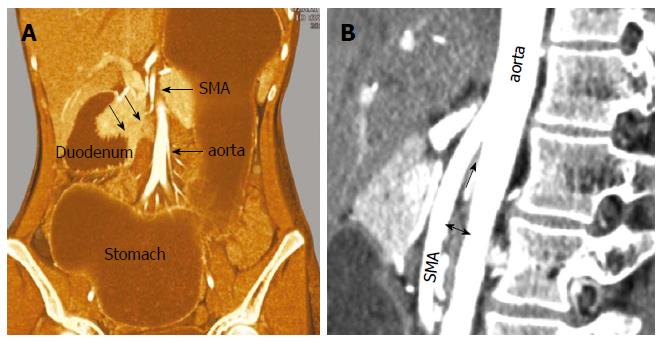
Three years prior to the surgery, a 17-year-old girl with a known history of AN presented to our emergency department with complaints of repeated vomiting and abdominal distension. She had been under the sporadic care of a psychiatrist and was not on any medications. A contrast-enhanced computed tomography scan also revealed a dilated stomach and proximal duodenum, and severe narrowing of the third portion of the duodenum (Figure 1A). A sagittal view showed the aorto-mesenteric angle was narrow at 10° (normal range, 25°-60°) and the aorto-mesenteric distance was short at 5.5 mm (normal range, 10-28 mm, Figure 1B). With these findings, the diagnosis of SMA syndrome was made. The patient was hospitalized five times over 3 years and experienced a 10-kg weight loss with persistent amenorrhea. As symptoms recurred frequently with conservative treatment, surgical treatment was suggested. Although the patient agreed to undergo surgery, she was very nervous about the residual scarring. Considering the impact on her body image, SILS was proposed. After discussion with the patient and her family, informed consent was obtained for laparoscopic duodenojejunostomy with single incision.
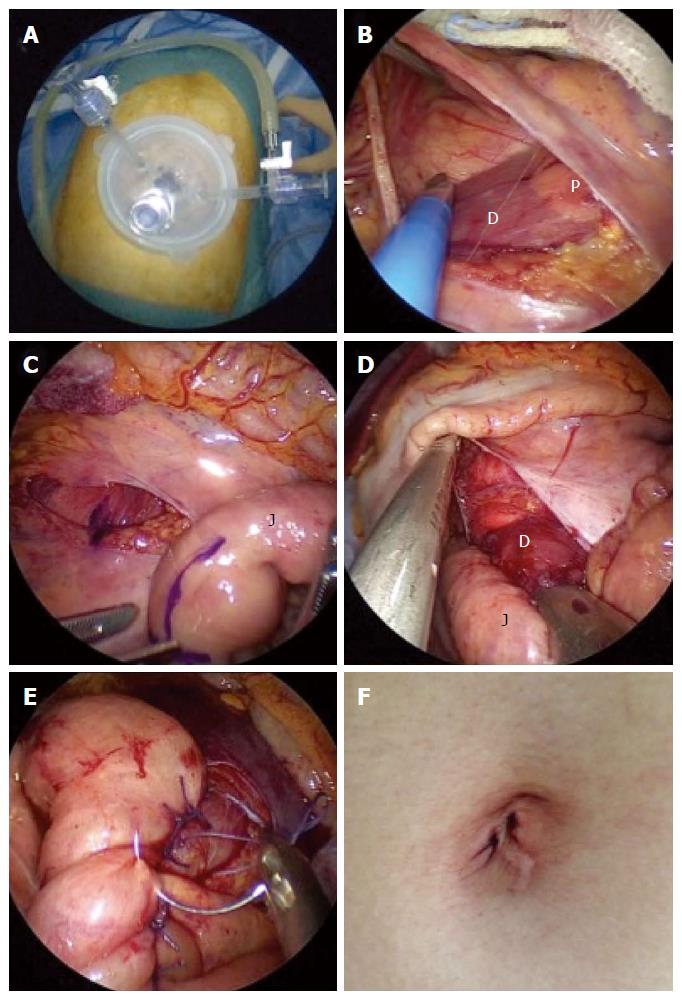
General anesthesia was induced and the patient was placed in the dorsal lithotomy position. The surgeon stood between the patient’s legs. The first assistant handled the scope on the patient’s left side. First, a trans-umbilical zigzag incision was made with the Hasson technique. After making the incision, a single-port three-channel device was inserted. Two 5-mm trocars and a 30° rigid 5-mm endoscope were used. With upward traction on the transverse colon, the dilated duodenum was easily identified. After isolation of the transverse mesocolon and duodenum, the anterior wall of second to third portion of the duodenum and the head of the pancreas were exposed. The duodenum and proximal jejunum (25 cm from the Treitz ligament) were marked with crystal violet at the planned anastomosis site, followed by a side-to-side duodenojejunostomy using a 45-mm stapler device. To insert the stapler device, one 5-mm trocar was replaced with a 12-mm trocar. The common entry hole was closed by hand in two layers, using 3-0 absorbable polyfilament. The patient’s body mass index was 14.0 kg/m2. The operative time was 148 min with little bleeding. No drain was placed. Intraoperative findings are summarized in Figure 2A-E.
The postoperative course was unremarkable. Oral fluid and solid food intake was allowed on postoperative day (POD) 2. An upper gastrointestinal study on POD 3 showed good patency of the anastomosis (Figure 3). The patient was discharged uneventfully on POD 6. Over the first 2 mo, she gained 3 kg. Although she continues to receive psychiatric care, she is doing well.
SMA syndrome is an uncommon but well-recognized clinical entity. It is seen more commonly in female individuals and usually occurs in older children and adolescents. SMA syndrome associated with AN has been also recognized[4,5]. Anorexia nervosa is a complex eating disorder characterized by an abnormally low body weight, intense fear of gaining weight, and a distorted body image. It is seen most commonly in teenage girls and young adult women. The excessive weight loss can result in the loss of the fatty tissue that surrounds the superior mesenteric artery and its neurovascular pedicle. In the absence of an appropriate fatty scaffolding, the angle at which the SMA branches from the aorta is reduced, resulting in compression of the third portion of the duodenum between the SMA and the aorta[6]. This combination of pathologies is uniquely challenging: SMA syndrome can precipitate and exacerbate AN because of the nausea associated with the small bowel obstruction and conversely, AN prevents the patient from being willing or able to ingest adequate calories to allow the SMA syndrome to resolve[7].
In addition to our patient, a literature search of the PubMed database between 1950 and 2015 retrieved 13 cases of SMA syndrome associated with AN (Table 1)[4,5,7-16]. The median age of these patients was 20 years (range, 16-47 years), indicating a greater frequency among young female patients. Most patients had low body weight with low body mass index. According to our literature search, about half of these patients were successfully managed with conservative treatment. The conservative treatment included both psychiatric and nutritional management. According to our literature search, 7 patients underwent laparotomy. While duodenojejunostomy was the most commonly performed procedure, gastrojejunostomy and Treitz ligament mobilization were also performed. One of them underwent exploratory laparotomy for a misdiagnosis of appendicitis and one had an unknown procedure. The weight gain was seen in only 4 patients, and some patients continued to lose weight despite surgical correction, indicating that AN was a refractory eating disorder. Generally, the patients who need surgical intervention would have severe symptoms because of their resistance to conservative treatment. However, the correlation between the impact of surgery and severity of anorexia nervosa is still unknown. To the best of our knowledge, this is the first reported case of successful single incision laparoscopic duodenojejunostomy performed on a patient with SMA syndrome in the setting of AN.
| No. | Year | Author | Age (yr) | Sex | Boby weight (kg) | Body mass index (kg/m2) | Treatment | Performed operation | Open or laparoscopic | Weight gain |
| 1 | 1976 | Vannatta et al | 17 | Female | 28 | NA | Surgery | Duodenojejunostomy | Open | Yes |
| 2 | 1978 | Froese et al | 16 | Male | NA | NA | Conservative | - | - | NA |
| 3 | 1981 | Sours et al | 17 | Female | 37.7 | NA | Conservative | - | - | NA |
| 4 | 1981 | Pentlow et al | 21 | Female | 32 | NA | Conservative | - | - | Yes |
| 5 | 1992 | Elbadaway et al | 18 | Female | 35.8 | 12.7 | Surgery | Gastrojejunostomy | Open | Yes |
| 6 | 1997 | Adson et al | 35 | Female | NA | NA | Surgery | Exploratory laparotomy | Open | NA |
| 7 | 1998 | da Silva et al | 28 | Female | NA | NA | Surgery | NA | NA | No |
| 8 | 2004 | Lo et al | 26 | Female | 37 | 16 | Surgery | Duodenojejunostomy | Open | No |
| 9 | 2009 | Verhoef et al | 16 | Female | 39 | 15 | Conservative | - | - | Yes |
| 10 | 2010 | Gwee et al | 17 | Female | 37.3 | 14.6 | Conservative | - | - | Yes |
| 11 | 2014 | Mearelli et al | 47 | Male | NA | NA | Surgery | Treitz ligament mobilization | Open | Yes |
| 12 | 2015 | Mascolo et al | 47 | Female | 29.1 | 10.6 | Conservative | - | - | Yes |
| 13 | 2015 | Our case | 20 | Female | 32 | 14 | Surgery | Duodenojejunostomy | Laparoscopic | Yes |
In recent years, SILS has been adopted for more and more cases with the innovation of surgical instruments and improvement in surgical experience and techniques. The benefits of this approach are associated with less incisional pain, less risk of incisional hernia, fewer wound complications, and improved cosmetic outcomes[17]. For example, gastrointestinal bypass with SILS has been introduced in the field of bariatric surgery. There are some reports of successful gastrojejunostomy[18,19], but only one case of single incision laparoscopic duodenojejunostomy was reported in 2014. This was performed in a 75-year-old man with SMA syndrome and resulted in a good postoperative outcome. As that report did not contain detailed images of the operation, we include intraoperative photographs here in the figures. Compared with that report, our procedure was a less invasive surgery because no drain was placed.
The benefit of selecting SILS in this case was its cosmetic outcome, which was important to the patient. To acquire a good operative field with minimal skin incision, we used a zigzag incision technique. Hachisuka et al[20] reported that this type of skin incision could become virtually scarless within months after an operation. In our case, the umbilical incision became virtually scarless 3 mo after surgery (Figure 2F).
Limitations that make SILS difficult to apply include internal and external conflicts between instruments and difficulty achieving traction for triangulation formation[21]. Through experience, we have learned best practices of using SILS in selected patients, including those needing cholecystectomy, appendectomy, and right hemicolectomy. Duodenojejunostomy is a simple procedure, requiring no organ resection. This resulted in fewer potential difficulties than other applications of SILS, such as cancer surgery. The loss of visceral fat, often seen in a patient with SMA syndrome or AN, resulted in a good operative field and made it easy to identify the target organs. Though the distance between the duodenum and the port site was relatively close, the interference between the scope and forceps was minimal. As SILS is often limited by the co-axial arrangement of the instruments, the close distance made the angle between the instruments wider. Using the cut mode for electrocautery instead of the coagulation mode can prevent organ injury for tensionless tissues. Dissection between the duodenum and the transverse mesocolon should be performed carefully with this method. The closure of the common entry hole after side-to-side duodenojejunostomy is an important procedure because it needs a skilled laparoscopic suturing technique. The interrupted or running suture should be performed precisely, despite the restricted operative field. To perform this operation safely, experience with SILS in other applications is recommended. Cholecystectomy or appendectomy might be a good initial experience with SILS. Right hemicolectomy is a good procedure for surgeons to learn the skills needed for duodenojejunostomy, as they have a similar operation field in the right upper quadrant. With all of these procedures, this “scarless” operation could lead to early recovery and cosmetic satisfaction.
Single incision laparoscopic duodenojejunostomy may be a feasible option as a curative operation for SMA syndrome. We believe that this minimally invasive surgery is especially beneficial for patients with SMA syndrome associated with AN and its associated body image issues, in terms of both surgical and cosmetic outcomes.
A 17-year-old girl with a known history of anorexia nervosa presented with complaints of repeated vomiting and abdominal distension.
The patient was diagnosed with superior mesenteric artery syndrome.
Anorexia nervosa, bulimia, megaduodenum or duodenal ileus.
Laboratory tests showed no abnormal value.
A contrast-enhanced computed tomography scan revealed a dilated stomach and proximal duodenum, and severe narrowing of the third portion of the duodenum.
Three years later, after the failure of conservative treatment, laparoscopic duodenojejunostomy was performed with single umbilical incision and operative course was uneventful.
While laparoscopic duodenojejunostomy is widely performed as a curative surgical approach, single incision laparoscopic approach is rarely performed. The authors show the first case of a young patient with superior mesenteric artery (SMA) syndrome who was successfully treated by single incision laparoscopic duodenojejunostomy.
Duodenojejunostomy is a surgical procedure for superior mesenteric artery syndrome, which includes the anastomosis between the proximal duodenum and a proximal loop.
Single incision laparoscopic duodenojejunostomy may be a feasible option as a curative operation for SMA syndrome, in terms of both surgical and cosmetic outcomes.
The authors firstly reported a case of single incision laparoscopic duodenojejunostomy, which could both cure SMA symdrome and improve cosmetic effect. We believe this minimally invasive surgery will be suitable for the patients with SMA syndrome who do not respond to the conservative treatment.
P- Reviewer: Xu L S- Editor: Yu J L- Editor: A E- Editor: Liu XM
| 1. | Gerasimidis T, George F. Superior mesenteric artery syndrome. Wilkie syndrome. Dig Surg. 2009;26:213-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Gersin KS, Heniford BT. Laparoscopic duodenojejunostomy for treatment of superior mesenteric artery syndrome. JSLS. 1998;2:281-284. [PubMed] |
| 3. | Lee TH, Lee JS, Jo Y, Park KS, Cheon JH, Kim YS, Jang JY, Kang YW. Superior mesenteric artery syndrome: where do we stand today? J Gastrointest Surg. 2012;16:2203-2211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 81] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 4. | Vannatta JB, Cagas CR, Cramer RI. Superior mesenteric artery (Wilkie’s) syndrome: report of three cases and review of the literature. South Med J. 1976;69:1461-1465. [PubMed] |
| 5. | Sours JA, Vorhaus LJ. Superior mesenteric artery syndrome in anorexia nervosa: a case report. Am J Psychiatry. 1981;138:519-520. [PubMed] |
| 6. | Valdes A, Cárdenas O, Espinosa A, Villazón O, Valdes V. Superior mesenteric artery syndrome. J Am Coll Surg. 2005;201:808. [PubMed] |
| 7. | Verhoef PA, Rampal A. Unique challenges for appropriate management of a 16-year-old girl with superior mesenteric artery syndrome as a result of anorexia nervosa: a case report. J Med Case Rep. 2009;3:127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Froese AP, Szmuilowicz J, Bailey JD. The superior-mesenteric-artery syndrome: cause or complication of anorexia nervosa? Can Psychiatr Assoc J. 1978;23:325-327. [PubMed] |
| 9. | Pentlow BD, Dent RG. Acute vascular compression of the duodenum in anorexia nervosa. Br J Surg. 1981;68:665-666. [PubMed] |
| 10. | Elbadaway MH. Chronic superior mesenteric artery syndrome in anorexia nervosa. Br J Psychiatry. 1992;160:552-554. [PubMed] |
| 11. | Adson DE, Mitchell JE, Trenkner SW. The superior mesenteric artery syndrome and acute gastric dilatation in eating disorders: a report of two cases and a review of the literature. Int J Eat Disord. 1997;21:103-114. [PubMed] |
| 12. | de Silva AP, Molagoda A, Fernando PL, de Silva HJ. The young woman who could not stop vomiting. Postgrad Med J. 1998;74:691-692. [PubMed] |
| 13. | Lo DY, Yen JL, Jones MP. Massive gastric dilation and necrosis in anorexia nervosa: cause or effect? Nutr Clin Pract. 2004;19:409-412. [PubMed] |
| 14. | Gwee K, Teh A, Huang C. Acute superior mesenteric artery syndrome and pancreatitis in anorexia nervosa. Australas Psychiatry. 2010;18:523-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Mearelli F, Degrassi F, Occhipinti AA, Casarsa C, De Manzini N, Biolo G. Pinched: superior mesenteric artery syndrome. Am J Med. 2014;127:393-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Mascolo M, Dee E, Townsend R, Brinton JT, Mehler PS. Severe gastric dilatation due to superior mesenteric artery syndrome in anorexia nervosa. Int J Eat Disord. 2015;48:532-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Bae SU, Baek SJ, Min BS, Baik SH, Kim NK, Hur H. Reduced-port laparoscopic surgery for a tumor-specific mesorectal excision in patients with colorectal cancer: initial experience with 20 consecutive cases. Ann Coloproctol. 2015;31:16-22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Morales-Conde S, Rubio-Manzanares Dorado M, Barranco A, Alarcón I, Pereira JL, García-Luna PP, Socas M. Single-port Roux-en-Y gastric bypass: toward a less invasive procedure with the same surgical results and a better cosmesis. Surg Endosc. 2013;27:4347-4353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Pitot D, Takieddine M, Abbassi Z, Agrafiotis A, Bruyns L, Ceuterick M, Daoudi N, Dolimont A, Soulimani A, Vaneukem P. Pure transumbilical SILS gastric bypass with mechanical circular gastrojejunal anastomosis feasibility. Surg Endosc. 2014;28:3007-3011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Hachisuka T, Kinoshita T, Yamakawa T, Kurata N, Tsutsuyama M, Umeda S, Tokunaga S, Yarita A, Shibata M, Shimizu D. Transumbilical laparoscopic surgery using GelPort through an umbilical zigzag skin incision. Asian J Endosc Surg. 2012;5:50-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Choi SI, Lee KY, Park SJ, Lee SH. Single port laparoscopic right hemicolectomy with D3 dissection for advanced colon cancer. World J Gastroenterol. 2010;16:275-278. [PubMed] |