Published online Jan 28, 2015. doi: 10.3748/wjg.v21.i4.1362
Peer-review started: June 17, 2014
First decision: June 27, 2014
Revised: August 6, 2014
Accepted: September 18, 2014
Article in press: September 19, 2014
Published online: January 28, 2015
Processing time: 224 Days and 19.6 Hours
A case of intractable upper gastrointestinal-hemorrhage was reported in a patient with portal hypertension caused by an arterioportal fistula (APF), namely, celiac axis-portal vein arteriovenous fistula. Portal hypertension caused by extrahepatic-APFs is extremely rare. Trauma, malignancy, and hereditary causes are the common etiology of APFs; but were absent in our patient. Our patient represents an unusual case of unexplained APF who presented with portal hypertension and was successfully managed through endovascular aortic repair.
Core tip: We present a rare case of intractable upper gastrointestinal hemorrhage due to celiac axis-portal vein arteriovenous fistula. Through this case report, we hope to highlight diagnosis of this unusual condition, and discuss our subsequent management. This case represents an unusual cases of unexplained presenting with portal hypertension that was successfully managed through endovascular aortic repair.
- Citation: Liu YR, Huang B, Yuan D, Wu ZP, Zhao JC. Unusual case of digestive hemorrhage: Celiac axis-portal vein arteriovenous fistula. World J Gastroenterol 2015; 21(4): 1362-1364
- URL: https://www.wjgnet.com/1007-9327/full/v21/i4/1362.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i4.1362
Portal hypertension is defined as the increase in porto-systemic resistance and/or flow[1]. The etiology of portal hypertension can be divided into pre-, intra-, and post-hepatic causes. The primary cause of portal hypertension is liver cirrhosis, which accounts for 90% of the cases in the United States[2]. The second - most common - etiology of portal hypertension is extrahepatic portal vein thrombosis, which accounts for 7% of cases. The remaining 3% of cases, including our case, are the result of a variety of rare etiologies.
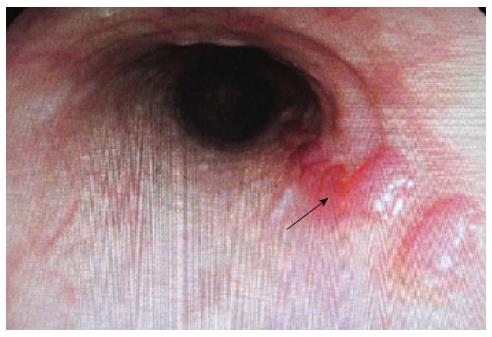
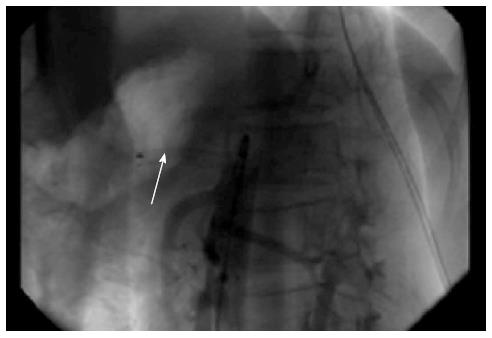
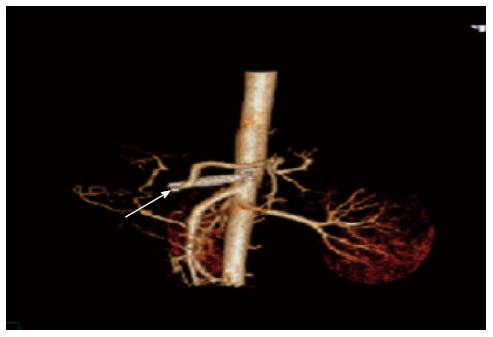
A-17-years old child with no history of liver disease or gastric ulcers was admitted to West China Hospital, Sichuan University for a five-day history of hematemesis and tarry stools. The physical examination revealed a blood pressure of 122/63 mmHg, a heart rate of 73 beats per minute, and a platelet count reduced to 45 × 109/L. Pertinent laboratory values of liver function, renal function, and electrolytes were normal; moreover all marks for hepatitis, and autoimmune disease were negative. Gastroscope revealed esophageal varices (Figure 1). Based upon this finding, it was speculated that the overflowing of the portal vein due to the shunt between the artery and the portal vein was causing perisinusoidal portal hypertension. To further confirm this hypothesis, digital subtraction angiography was performed and revealed a mass of 52 mm × 48 mm. The portal vein was highlighted at the arterial phase, strongly suggesting that the mass was an arterioportal fistula involving an arteriole from celiac axis feeding directly into the portal vein (Figure 2). Taken together, the arterioportal fistula was concluded to be the cause of this patient’s non-cirrhotic portal hypertension. Surgery was performed under local anesthesia with full hemodynamic monitoring. The right femoral artery was isolated, and 5-F catheter sheaths were placed into the right femoral artery via guidewire. A covered stent (10 mm × 40 mm. Fluency Plus-) was deployed slowly and accurately in the celiac axis. An aortogram revealed no endoleak and no blood flow entering into the portal vein, but the proper hepatic artery and left gastric artery were not observed (Figure 3). The post-operation recovery of the patient has been uneventful, and no additional episodes of upper gastrointestinal bleeding have been reported by the patient on three subsequent clinic visits during the last six months (Figure 4).
Most reports on the etiology of arterioportal fistula (APF) in the literature is focuses on trauma, hepatocellular carcinoma (HCC), and congenital causes[3]. The clinical manifestations of APFs include congestive heart failure (40%-60%), portal hypertension (20%-40%), and diarrhea with abdominal pain (20%)[4]. Hepatic trauma is a common cause of APFs. HCC can cause APFs, and studies have demonstrated that APFs may occur in up to 60% of patients with HCC[5,6]. Congenital APFs are associated with portal hypertension and gastrointestinal hemorrhage[3,7]. The portal hypertension in our patient manifested as splenomegaly on computed tomography, as esophageal varices on gastroscope and, as blood platelet counts reduced to 45 × 109/L. Our patient did not have the any history of congenital APF, abdominal trauma, or malignancy. Thus, we believe that the present report is a case of unexplained AFP. Based on literature search, this is one of the few cases of unexplained APF presenting with portal hypertension.
The treatment of APF is either surgical or minimally invasive though interventional radiology (IR) techniques. Surgical ligation of the supplying artery can performed, but the surgical wound of patient is not inconsequential. IR offers many advantages over surgical treatment. These advantages include decreased morbidity and mortality, reduced risk of subsequent complications, and a significant reduction in the time required for recovery. With the advancement of interventional radiology techniques, the trend has shifted to IR techniques[8]. The AFP adhesion in our patient was serious; therefore, we selected IR technique.
IR is accomplished through artery embolization. The therapy in our case was accomplished through celiac axis endovascular aortic repair; Because we were concerned about the risk of celiac axis embolism of the coils of the IR intervention. Endovascular aortic repair complications include non-target repair, hepatic infarction, and ischemic cholangitis. The proper hepatic artery in our case was covered with a stent because of stent migration, however, the proper hepatic artery in our case exhibited a decreased diameter, and no complications were observed.
In summary, we described a case of portal hypertension due to unexplained APF. The patient was successfully treated through endovascular aortic repair and is being monitored regularly in our outpatient clinic without any further episodes of bleeding.
The child with no history of liver disease or gastric ulcers was admitted to hospital for a five-day history of hematemesis and tarry stools.
Digestive hemorrhage: celiac axis-portal vein arteriovenous fistula.
Portal hypertension was caused by liver diseases and gastric ulcers, but the patient with no history of liver diseases and gastric ulcers.
Platelet count reduced to 45 × 109/L. Pertinent laboratory values of liver function, renal function, and electrolytes were normal; moreover all marks for hepatitis, and autoimmune disease were negative.
Computed tomography (CT) revealed a mass of 52 mm × 48 mm behind the head of the pancreas. The portal vein was highlighted at the arterial phase, strongly suggesting the existence of a hepatic arterioportal communication.
Patient was successfully managed through endovascular aortic repair.
Intractable upper gastrointestinal hemorrhage for portal hypertension caused by an arterioportal fistula (APF) is rare, however, though CT or digital subtraction angiography we can find the cause.
Patients with intractable upper gastrointestinal hemorrhage, with no history of liver disease or gastric ulcers, should be diagnosed as portal hypertension caused by an APF.
This manuscript illustrates an unusual cause of gastrointestinal hemorrhage. This article encourages the clinician to consider a unique source of portal hypertension caused by APF.
P- Reviewer: Saito T S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Bari K, Garcia-Tsao G. Treatment of portal hypertension. World J Gastroenterol. 2012;18:1166-1175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 95] [Cited by in RCA: 104] [Article Influence: 8.0] [Reference Citation Analysis (1)] |
| 2. | García-Pagán JC, Gracia-Sancho J, Bosch J. Functional aspects on the pathophysiology of portal hypertension in cirrhosis. J Hepatol. 2012;57:458-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 207] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 3. | Garcia-Tsao G, Korzenik JR, Young L, Henderson KJ, Jain D, Byrd B, Pollak JS, White RI. Liver disease in patients with hereditary hemorrhagic telangiectasia. N Engl J Med. 2000;343:931-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 233] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 4. | Strodel WE, Eckhauser FE, Lemmer JH, Whitehouse WM, Williams DM. Presentation and perioperative management of arterioportal fistulas. Arch Surg. 1987;122:563-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Redmond PL, Kumpe DA. Embolization of an intrahepatic arterioportal fistula: case report and review of the literature. Cardiovasc Intervent Radiol. 1988;11:274-277. [PubMed] |
| 6. | Allison DJ, Jordan H, Hennessy O. Therapeutic embolisation of the hepatic artery: a review of 75 procedures. Lancet. 1985;1:595-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 82] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Garcia-Tsao G. Liver involvement in hereditary hemorrhagic telangiectasia (HHT). J Hepatol. 2007;46:499-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 125] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 8. | Ridout DL, Bralow SP, Chait A, Nusbaum M. Hepatoportal arteriovenous fistula treated with detachable balloon embolotherapy. Am J Gastroenterol. 1989;84:63-66. [PubMed] |