Published online Jan 21, 2015. doi: 10.3748/wjg.v21.i3.1036
Peer-review started: April 27, 2014
First decision: May 29, 2014
Revised: June 23, 2014
Accepted: July 24, 2014
Article in press: July 25, 2014
Published online: January 21, 2015
Processing time: 269 Days and 3.5 Hours
Paraganglioma is a rare tumor of paraganglia, derived from neural crest cells in sympathetic or parasympathetic ganglions. Primary paraganglioma originating from the pancreas is rare. We report two patients with paraganglioma in the head of the pancreas, in whom computed tomography showed a sharply marginated, hypervascular tumor with cystic areas. Significant intratumoral vessels and early contrast filling of the draining veins from the mass were not found. Although the pancreatic paraganglioma was located at the pancreatic head, the bile ducts often revealed no dilation, and sometimes the main pancreatic duct was mildly dilated. These findings are helpful in differentiating pancreatic paraganglioma from other pancreatic neoplasms. It is often difficult to distinguish between nonfunctional pancreatic paragangliomas and pancreatic endocrine tumors. In many reports,pancreatic paragangliomas show the retroperitoneal extension of a paraganglioma into the pancreas rather than a true pancreatic neoplasm. In surgical treatment, we could select simple excision of the tumor rather than radical surgery.
Core tip: Primary paraganglioma that arises in the pancreas is rare. We herein present two pathologically proven cases of pancreatic paraganglioma, retrospectively analyze their clinical and imaging features, and review the literature.
- Citation: Meng L, Wang J, Fang SH. Primary pancreatic paraganglioma: A report of two cases and literature review. World J Gastroenterol 2015; 21(3): 1036-1039
- URL: https://www.wjgnet.com/1007-9327/full/v21/i3/1036.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i3.1036
Paraganglioma is a rare tumor of paraganglia, derived from neural crest cells in sympathetic or parasympathetic ganglions[1,2]. Intra-adrenal paraganglioma is found mainly in the adrenal medulla, and extra-adrenal paraganglioma is located in the head, neck, mediastinum and retroperitoneum. Primary paraganglioma that arises in the pancreas is rare[3].
A 54-year-old woman felt left upper abdominal pain for 20 d. She denied obvious symptoms of gastric bleeding and vomiting. Blood tests and blood pressure were normal. On medical examination, no mass of upper abdomen was palpated. Her abdomen was soft without tenderness and jaundice.
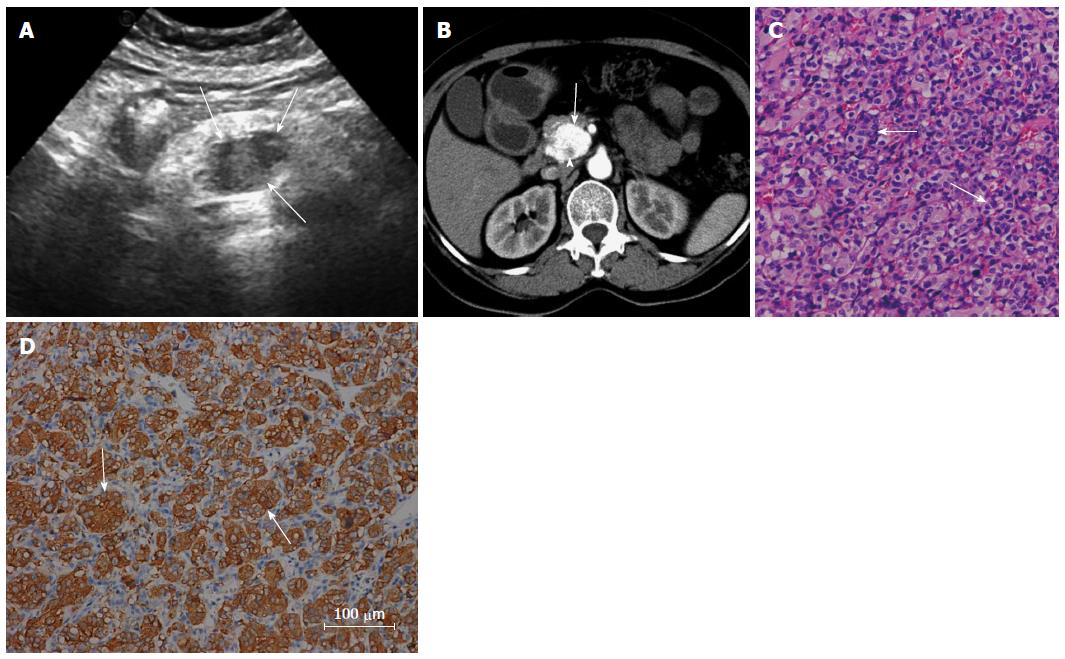
She underwent upper abdominal ultrasound, which showed an ill-defined hypoechoic mass in the pancreatic head (Figure 1A). The mass measured 2.6 cm × 2.3 cm, and the blood flow signal was plentiful. Unenhanced computed tomography (CT) revealed a poor-defined isodense mass in the head of the pancreas. On contrast-enhanced CT, the mass in the pancreatic head was found with heterogeneous striking enhancement during the arterial phase (Figure 1B), while non-enhancing patchy areas were seen in the tumor (Figure 1B). During the venous phase, the same mass was well-defined with homogeneous marked enhancement. No invasion of the adjacent organs was seen around the pancreas. Intraoperatively, a well-defined mass, 3 cm × 2.5 cm, was found with a rich supply of blood and soft texture in the pancreatic head.
Gross pathological examination revealed an encapsulated mass from the pancreas, 3 cm × 2.5 cm, with gray-red soft tissue and moderate texture. Microscopically, the tumor showed round or polygonal cells with rich cytoplasm on the hematoxylin-eosin-stained tissue sections. The tumor cells had round or ovoid nuclei (Figure 1C), arranged in nest-like structure with dilated capillary intervals. Immunohistochemical study revealed positive staining for S-100, cytokeratin (CK), non-specific enolase (NSE), CgA and Syn (Figure 1D), but negative reactions to CD34, CD117, DOG, SMA, Des and HMB47. The tumors were finally diagnosed as primary pancreatic paraganglioma.
A 41-year-old woman was found to have an upper abdominal mass incidentally on ultrasound examination 6 d earlier. She denied obvious symptoms of gastric bleeding and abdominal discomfort. Blood tests and liver and renal functions were normal. On medical examination, no mass of upper abdomen was palpated. Her abdomen was soft without tenderness and jaundice. She had no acute pain, and her signs of life were normal.
On ultrasound examination, she was found to have a well-demarcated hypoechoic mass in the pancreatic head with homogeneous echo of other pancreatic tissues. The mass measured 6.2 cm × 4.4 cm × 4.5 cm, and some blood flow signal was seen. The diameter of the main pancreatic duct was 0.73 cm and the diameter of the common bile duct was 0.46 cm.
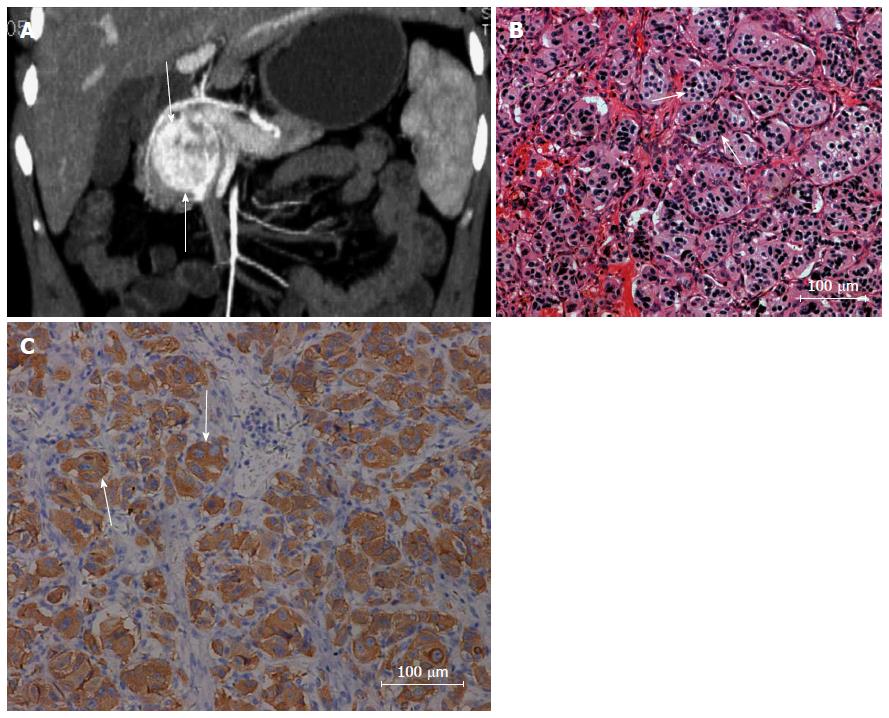
Unenhanced CT revealed a poor-defined mass in the pancreatic head with low and heterogeneous density. On contrast-enhanced CT, a well-demarcated mass in the head of the pancreas, 4.2 cm × 4 cm, was found with marked enhancement (Figure 2A), while some patchy areas were not enhanced. The main pancreatic duct was mildly dilated.
Intraoperatively, a mass measuring 6 cm × 5 cm with well-demarcated margins was found in the pancreatic head without infiltration of the adjacent organs and blood vessels. The main pancreatic duct was dilated with a diameter of 0.4 cm. No significant lymph nodes were seen around the pancreas.
Gross pathological examination revealed a well-defined mass from the pancreas, 4 cm × 4 cm, with gray-yellow soft tissue and hard texture. Under microscopic examination, the tumor cell nuclei were round or ovoid. Nuclear staining was deeper in some areas. A few cells had large nuclei with hyperchromatism and pink cytoplasm, arranged in organ-like or nest-like structures (Figure 2B). The stroma was rich in capillaries.
Immunohistochemistry showed S-100, CK, NSE, CgA and Syn positivity (Figure 2C). Insulin,somatostatin and glucagon were negative. At last, the tumors were diagnosed as primary paraganglioma arising from the pancreas.
The paraganglion system is composed of numerous neuroepithelial cells (chief cells). There are many neuronal secretion granules with catecholamines in the cytoplasm. Microscopically, the chief cells are surrounded by the sustentacular cells, arranged in nest-like structures (cell balls). Intra-adrenal paraganglioma is mainly present in the adrenal medulla as pheochromocytoma. Extra-adrenal paraganglioma is divided into two major categories. One type is chemodectoma, which is located in the parasympathetic nervous system in the head, neck or mediastinum, and is non-chromaffin. The other type is ectopic pheochromocytoma, which is located in the sympathetic nervous system in the retroperitoneum or along the aorta, and contains chromaffin.
Primary paraganglioma that arises in the pancreas is rare. It is characterized on imaging features as sharply marginated, hypervascular tumor with cystic areas;the latter reveals necrotic or cystic change. Our two pathologically proven cases were in accordance with the above imaging features. Kim et al[3] reported a well-defined, extremely hypervascular pancreatic paraganglioma with significant intratumoral vessels and early contrast filling of the draining veins from the mass. In our two cases, these imaging characteristics were not found.
Although the pancreatic paraganglioma is located at the pancreatic head, the bile ducts often reveal no dilation, and sometimes the main pancreatic duct is mildly dilated. The CT findings are different from those of pancreatic carcinoma, which is usually characterized as a mild to moderate enhanced tumor with prominent dilation of the biliary and pancreatic ducts, as well as retroperitoneal invasion[4]. Clinically, functional pancreatic endocrine tumor is usually < 3 cm, with striking and homogenous enhancement in the arterial phase. The diameter of nonfunctional pancreatic endocrine tumor is usually > 5 cm. The tumor always has necrosis, cystic change or calcification, so it shows heterogeneous or ring-liked enhancement[5]. It is often difficult to distinguish between nonfunctional pancreatic paragangliomas and pancreatic endocrine tumors. In many reports, pancreatic paragangliomas show the retroperitoneal extension of a paraganglioma into the pancreas rather than a true pancreatic neoplasm[6]. In relation to surgical treatment, the prognosis is equally good for simple excision of the tumor and radical surgery such as pancreaticoduodenectomy. In our patients, combinatorial image analysis helped us to diagnose pancreatic paraganglioma and we could select the non-excessive surgical treatment without post-surgical functional disorder of the pancreas[7].
In conclusion, we report two patients with paraganglioma in the head of the pancreas, in whom CT showed a well-defined tumor with cystic areas and rich blood supply. These findings are helpful in differentiating pancreatic paraganglioma from other pancreatic neoplasms. For surgical treatment, we could select simple excision of the tumor rather than radical surgery.
Case 1 felt left upper abdominal pain for 20 d. Case 2 denied obvious symptoms of gastric bleeding and abdominal discomfort.
The mass was found in the pancreatic head.
Computed tomography (CT) findings are helpful to differentiate between pancreatic paraganglioma and other pancreatic neoplasms, such as pancreatic carcinoma and pancreatic endocrine tumor.
Blood tests and liver and renal functions were normal.
CT findings are a well-defined, hypervascular tumor with cystic areas.
The tumors were finally diagnosed as primary pancreatic paraganglioma by microscopic examination and immunohistochemical study.
Simple excision of the tumor was performed.
Primary paraganglioma that arises in the pancreas is rare. Lightfoot et al found pancreatic paragangliomas in many reports show the retroperitoneal extension of a paraganglioma into the pancreas rather than a true pancreatic neoplasm.
Paraganglioma is a rare tumor of the paraganglia, derived from neural crest cells in sympathetic or parasympathetic ganglions. These tumors can be widely distributed from the adrenal medulla to the head, neck, mediastinum and retroperitoneum.
It is often difficult to distinguish between pancreatic paragangliomas and pancreatic endocrine tumors.
The authors reported two patients with paraganglioma in the head of the pancreas, a rare pancreatic tumor. The imaging features of pancreatic paraganglioma are well described. These findings are helpful to differentiate between pancreatic paraganglioma and other pancreatic neoplasms.
P- Reviewer: Hackert T, Yang LB S- Editor: Gou SX L- Editor: A E- Editor: Liu XM
| 1. | Borgohain M, Gogoi G, Das D, Biswas M. Pancreatic paraganglioma: An extremely rare entity and crucial role of immunohistochemistry for diagnosis. Indian J Endocrinol Metab. 2013;17:917-919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Jamilloux Y, Favier J, Pertuit M, Delage-Corre M, Lopez S, Teissier MP, Mathonnet M, Galinat S, Barlier A, Archambeaud F. A MEN1 syndrome with a paraganglioma. Eur J Hum Genet. 2014;22:283-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Kim SY, Byun JH, Choi G, Yu E, Choi EK, Park SH, Lee MG. A case of primary paraganglioma that arose in the pancreas: the Color Doppler ultrasonography and dynamic CT features. Korean J Radiol. 2008;9 Suppl:S18-S21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | He J, Zhao F, Li H, Zhou K, Zhu B. Pancreatic paraganglioma: A case report of CT manifestations and literature review. Quant Imaging Med Surg. 2011;1:41-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 5. | Procacci C, Carbognin G, Accordini S, Biasiutti C, Bicego E, Romano L, Guarise A, Minniti S, Pagnotta N, Falconi M. Nonfunctioning endocrine tumors of the pancreas: possibilities of spiral CT characterization. Eur Radiol. 2001;11:1175-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 47] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Lightfoot N, Santos P, Nikfarjam M. Paraganglioma mimicking a pancreatic neoplasm. JOP. 2011;12:259-261. [PubMed] |
| 7. | Ohkawara T, Naruse H, Takeda H, Asaka M. Primary paraganglioma of the head of pancreas: contribution of combinatorial image analyses to the diagnosis of disease. Intern Med. 2005;44:1195-1196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |