MAIN TEXT
Hepatocellular carcinoma (HCC) is the sixth most common cancer and the third most common cause of cancer-related deaths worldwide[1,2]. As HCC is usually associated with cirrhosis, the treatment is complex because of the need to be oncologically radical but liver parenchymal-destruction conservative[3]. Potentially curative treatments for HCC include liver resection, transplantation, or local ablative therapy[4].
The Barcelona Clinic Liver Cancer (BCLC) classification[5] has been endorsed as the optimal staging system and treatment algorithm for HCC by the European Association for the Study of Liver Disease (EASL) and the American Association for the Study of Liver Disease (AASLD)[6,7]. The main prognostic factors of this staging system are related to tumor status (defined by the number and size of nodules, the presence or absence of vascular invasion and the presence or absence of extrahepatic spread), liver function (defined by the Child-Pugh classification and portal hypertension), and general performance status defined by the Eastern Cooperative Oncology Group (ECOG). The BCLC classification links stage stratification with corresponding therapeutic recommendations, with liver resection recommended only to those patients harboring early-stage tumors (BCLC Stage A)[1,5,7]. However, a recent study published in Ann Surg[8] disclosed that in ten well-known hepatobiliary tertiary referral centers in the West and the East, 50% of patients harboring intermediate or advanced HCC still underwent surgery despite the BCLC guidelines recommend palliative treatments (chemoembolization or oral sorafenib). As liver surgeons, we would like to raise the following comments, which need to be discussed with and further clarified by the BCLC constitutors.
First, judgment subjectivity exists in the BCLC classification to some extent, which takes root in the assessment of the ECOG PS itself (an important prognostic factor in this classification). According to the definition of the BCLC classification, patients with advanced HCC (i.e., BCLC stage C) include patients with cancer-related symptoms (PS 1-2), vascular invasion, extrahepatic spread, or a combination[1]. In other words, once the HCC patients have cancer-related symptoms (PS 1 means still near fully ambulatory and PS 2 means less than 50%[9]), they should be classified as advanced HCC (i.e., BCLC stage C). However, it is often difficult to judge whether atypical symptoms such as abdominal pain or malaise, are tumor-related or liver-related, as more than half of patients with HCC have cirrhosis at diagnosis. Actually, biases by physicians on subjective evaluation commonly exist in clinical practice, especially for those patients with a single HCC but with compensated cirrhosis (Child-Pugh A).
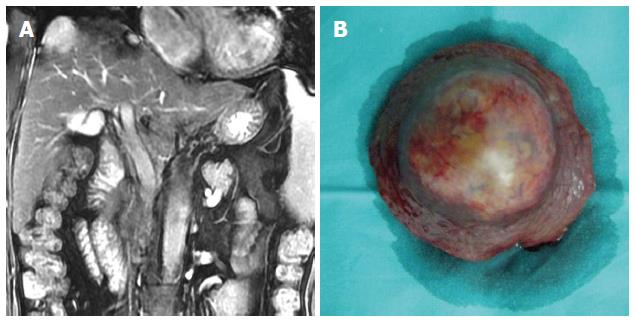
In our opinion, even if the patient’s symptoms are definitely tumor-related (i.e., PS 1-2), the diagnosis of advanced HCC in the BCLC classification is debatable. A female patient who complained of persistent right epigastric pain was diagnosed to harbor a single 3-cm HCC with compensated cirrhosis (Child-Pugh A). Her persistent abdominal pain (PS 2) was caused by an exophytic tumor growth compressing on the diaphragm (Figure 1). According to the BCLC classification, she had a BCLC stage C HCC. According to the BCLC guidelines, only oral sorafenib should be given. In actual fact curative HCC resection was successfully performed for this patient in August 2007, and she is still alive and disease-free.
Figure 1 Patient 1.
A 55-year-old woman with a 30-year-history of hepatitis B virus infection presented with persistent right upper-quadrant pain. Her performance status was 2, her AFP was > 1000 μg/L and her liver function was Child-Pugh A. She was diagnosed with a Barcelona Clinic Liver Cancer stage C hepatocellular carcinoma (HCC) with compensated cirrhosis. A: MRI showed a single 3.0-cm tumor in segment 8 with exophytic growth towards the diaphragmatic dome; B: She underwent curative liver resection for HCC in August 2007, and is still alive and disease-free.
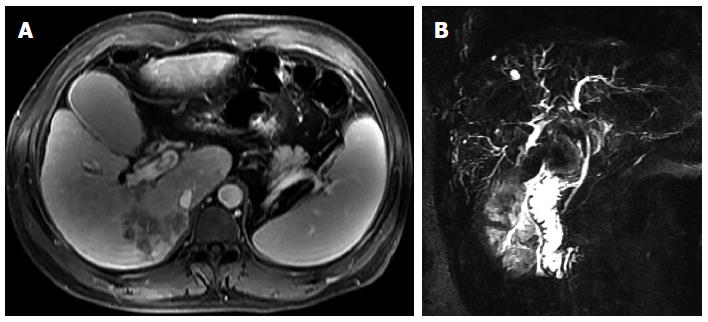
Additionally, although the BCLC constitutors tried very hard to take every possible situation into consideration, the truth is that in many HCC patients the situation is more complicated. For example, the BCLC classification gave full consideration of the presence of vascular invasion as an independent poor prognostic factor of HCC, but it never mentioned the presence of biliary invasion (Figure 2), which is a specific but not an uncommon type of HCC[10]. Previous studies has shown that the prognosis of HCC with biliary invasion with or without obstructive jaundice is as poor as HCC with vascular invasion despite treatment[11-13]. Should biliary invasion be included into the BCLC staging just like vascular invasion? It may be still a blind spot by the BCLC classification[14].
Figure 2 Patient 2.
A 42-year-old man presented with yellowish discoloration of skin. Liver function tests revealed obstructive jaundice. His performance status was 2, his AFP was 512 μg/L and his liver function was Child-Pugh B. He was diagnosed with a Barcelona Clinic Liver Cancer stage C hepatocellular carcinoma with biliary invasion. A: CT scan showed a 5.0-cm tumor with ill-defined margins in segment 6; B: MRCP showed a filling defect in the upper common bile duct.
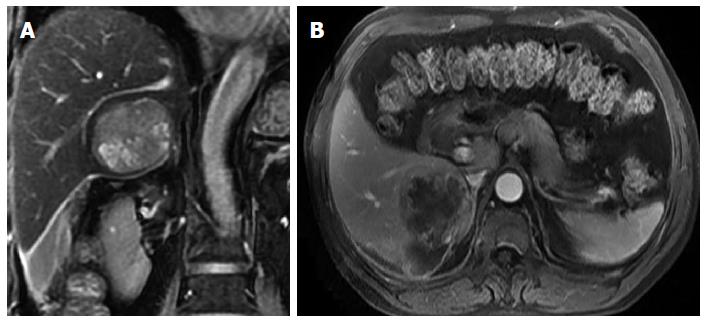
Another specific group of HCC patients who have never been mentioned in the BCLC classification is ruptured HCC (Figure 3), which happens in about 3%-15% of patients with HCC[15-18]. Once a patient develops acute spontaneous rupture of HCC (mostly PS 3-4 as a life-threatening complication), the patient should be classified according to the BCLC classification as having a terminal stage HCC (i.e., BCLC stage D). Should only supportive care be given to these patients in accordance with the BCLC guidelines? In numerous previously published studies, emergency transarterial embolization or liver resection (either emergency or staged) have been performed on these patients, and satisfactory results have been obtained, including saving lives in acute emergencies and even having occasional patients with long-term survival[15,16,18-22]. Thus, in our opinions, it is necessary for the BCLC classification to clarify this special but not uncommon situation of HCC so as to avoid some clinicians blindly adhering to the treatment guidelines.
Figure 3 Patient 3.
A 60-year-old man with documented hepatitis B virus infection complained of sudden right abdominal pain and temporary loss of consciousness. His performance status was 3 and his liver function was Child-Pugh A. He was diagnosed with hemorrhagic shock and a Barcelona Clinic Liver Cancer stage D hepatocellular carcinoma (HCC) presenting with spontaneous rupture. A and B: Magnetic resonance imaging showed a single 5.5-cm tumor in segment 6 and homogeneous liquid area around and below the right liver. He underwent emergency liver resection in January 2011 and subsequent abdominal wall metastasis resection in December 2011. He is still alive but he has developed intrahepatic recurrence of HCC.
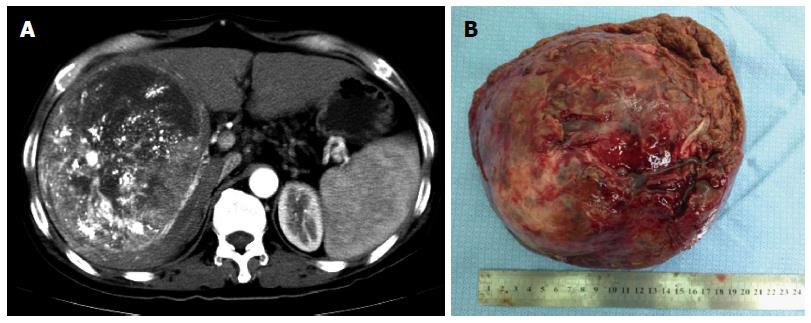
For most liver surgeons, it is not surprising that the authors of the recent study[8] stated that the BCLC treatment recommendation concerning surgery for HCC was too restrictive, and the authors suggested updating the EASL/AALSD therapeutic guidelines. However, in two subsequent correspondences[23,24], Dr. Bruix (one of the BCLC constitutors) and other renowned scholars pointed out the misclassification between the BCLC stage A and B for some patients in the study. In the subsequent replies[25,26] by the authors, a large number of articles released by the BCLC constitutors[1,5-7,27-32] were listed which clearly indicated 5 cm was used as a cutoff point between the BCLC stages A and B (intermediate), and the variable of size was included as a criterion for the differentiation between these two stages (Figure 4A). Beyond any doubt, this is a high-level debate in academic circles because most of these participating scholars have published hundreds of academic papers in the field of HCC. What is worth reflecting on is why such a controversy on the BCLC classification should still exist among these top experts in HCC. Would it be even more confusing for the majority of ordinary clinicians? It seems incredible to us that this recent debate on which BCLC stage should a patient with HCC belong to is still on-going, as the BCLC classification has been proposed for 15 years[5] and it has passed through several sequential revisions[1,32,33].
Figure 4 Patient 4.
A 54-year-old man with long-standing chronic hepatitis B virus (HBV) infection and cirrhosis was diagnosed with hepatocellular carcinoma (HCC) during an annual routine check-up. Six weeks before his hospitalization in our center, he received transcatheter arterial chemoembolization for HCC. His performance status was 0 and his liver function was Child-Pugh A. He was diagnosed with a Barcelona Clinic Liver Cancer stage A? B? HCC and HBV-related cirrhosis. A: Computed tomography scan showed a single 17.5-cm tumor in segments 5, 6, 7, and 8 with well-defined margins and sporadic lipiodol depositions within the tumor; H: He underwent curative liver resection of HCC in July 2012, and is still alive.
Undoubtedly, HCC is one of the most complicated and heterogeneous disease which requires multidisciplinary management by a team of hepatologists, surgeons, interventional radiologists, oncologists, pathologists, and nurses. The purpose of formulation of a staging system is to provide accurate information for easy classification of patients into different risk groups. A precise staging helps to make therapeutic decisions and to estimate prognosis. Unfortunately, the best tool for staging HCC remains controversial. The lack of a consensus on an HCC staging system is mostly in part related to the heterogeneity in treatment modalities at diagnosis[34]. Therefore, as we think, it is necessary to establish specific HCC staging systems to assess prognosis, directed toward different treatment modalities, for example, for those patients with resectable or non-resectable HCC[35,36]. Considering the most complexities of HCC treatment among all malignancies, it was inadvisable and impractical to try conducting a specific or sole treatment modality for all HCCs by using a seemingly simple but uniform treatment algorithm just like the current BCLC guideline, which may well do more than good in the real life. Therefore, this should be the major intrinsic limitation of the BCLC classification, since this so-called “authoritative guidance” attempts generalize all probabilities of the treatment for patients with HCC.
In addition, it should be noted that only surgery, radiofrequency ablation, TACE, oral sorafenib, and symptomatic treatment were recommended in the BCLC guideline, but many other effective or promising treatment modalities for HCC have never been mentioned by the BCLC treatment schedule, such as radiotherapy, Yttrium (90) radioembolization, cryotherapy, microwave coagulation therapy, laser therapy, traditional Chinese medicine, immunotherapy, and so on[37-41]. Therefore, it should be considered as biased and insufficient for the BCLC treatment guideline, which may also need to be further modified by the BCLC conductors in the future.
It’s worth mentioning that nowadays the majority of patients who are not considered ideal candidates based on the BCLC guideline still agree to undergo hepatic resection all around the world[8,42,43]. An international multicenter study by Roayaie et al[42] which reported a 5-year overall survival rate of > 30% in the candidates based on the current guidelines for HCC. This group of patients accounted for nearly 70% of all the patients who underwent hepatic resection during the study period. These figures tell us currently there are many hepatic surgeons who do not follow the guidelines for HCC according to the BCLC recommendation[44-46]. Are these surgeons irresponsible? Or have patients been misled by these surgeons to make a wrong decision?
The superiority of the BCLC classification, when compared with other existing staging systems, is to provide treatment recommendations based on different stages of HCC. However, the validity of some of these recommendations requires further verification, since most of them are based on observational studies. Till now, there is still a lack of good high-level evidences in the field of HCC treatment (only fewer than one hundred RCTs on HCC have been published in the medical literature)[27]. Therefore, more clinical evidences need to be created and accumulated in the future. Admittedly, the evidences coming from RCTs are more reliable and valuable than those coming from retrospective or prospective cohort studies, although it is not desirable to underestimate, or even deny, the true value of the latter types of studies. We should also recognize that it is difficult, sometimes even impossible to conduct a RCT, especially those involving surgery, as funding support for a surgical research is always the biggest obstacle compared with a new drug research. Adding to the complexity on therapeutic researches on HCC, whether multidisciplinary treatment is better than singly therapy, and whether personalized therapy would produce better results to an individual patient with HCC are questions which have not been answered.
As Dr. Bruix[1] said, further refinement is still needed for the BCLC classification. We herein bring up our doubts and confusions about the BCLC classification. We hope to further discuss with peers and colleagues with an aim to make the BCLC classification more applicable to clinical practice in the future.