Published online Jul 7, 2015. doi: 10.3748/wjg.v21.i25.7929
Peer-review started: January 12, 2015
First decision: March 10, 2015
Revised: April 9, 2015
Accepted: May 21, 2015
Article in press: May 21, 2015
Published online: July 7, 2015
Processing time: 181 Days and 3.2 Hours
Neuroblastoma (NB) is the most common extracranial solid tumor in children. Diarrheal NB is quite rare and is not easy to diagnose in the early stage. Six cases of diarrheal NB in our hospital treated from 1996 to 2006 were retrospectively analyzed, including characteristics such as electrolyte imbalance, pathologic features, vasoactive intestinal peptide (VIP) immunohistochemical staining results, treatment, and prognosis. All patients were boys with 3-8 loose or watery stools each day and routine fecal tests were normal. Abdominal tumors were identified by B-ultrasound. Drugs were ineffective. Three patients underwent surgery, and the remaining three patients received surgery and chemotherapy. Diarrhea stopped after treatment in five patients. Two patients died due to intractable hypokalemia. The tumor was located in the adrenal gland in four patients, in the upper retroperitoneum in one patient, and in the presacral area in one patient. Pathologic findings were NB and ganglioneuroblastoma. Five patients were at clinical stage I-II, and one was at stage III. Four patients survived (followed-up for 6 mo to 4 years). Immunohistochemical staining for VIP was positive. Refractory diarrhea is a paraneoplastic syndrome of NB and is rare. Patients aged 1-3 years who present with chronic intractable diarrhea should be followed closely. Intractable diarrhea, hypokalemia, and dysplasia are the initial clinical manifestations. Increased VIP is characteristic of this disease. Potassium supplementation plays a vital role in the treatment procedure, especially preoperatively. The prognosis of diarrheal NB is good following appropriate treatment.
Core tip: Neuroblastoma (NB) is the most common extracranial solid tumor in children. Diarrheal NB is quite rare and is not easy to diagnose in the early stage. Six cases of diarrheal NB were retrospectively analyzed, including characteristics such as electrolyte imbalance, pathologic features, vasoactive intestinal peptide immunohistochemical staining results, treatment, and prognosis.
- Citation: Han W, Wang HM. Refractory diarrhea: A paraneoplastic syndrome of neuroblastoma. World J Gastroenterol 2015; 21(25): 7929-7932
- URL: https://www.wjgnet.com/1007-9327/full/v21/i25/7929.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i25.7929
Neuroblastoma (NB) is the most common extracranial solid tumor in children, and the primary tumor can be located in any part of the sympathetic chain or the adrenal medulla[1]. The tumor is most commonly found in the abdomen (75%), followed by the mediastinum (20%) and the neck (5%)[2]. Retroperitoneal NB is initially enigmatic, leading to progression and a poor prognosis. Patients with diarrhea as the main symptom, namely diarrheal NB, are quite rare[3]. Consequently, diarrheal NB is not easy to diagnose in the early stage of the disease. In this article, data from six patients with diarrheal NB treated in our hospital from 1996 to 2006 were retrospectively analyzed, including characteristics such as electrolyte imbalance, pathologic features, vasoactive intestinal peptide (VIP) immunohistochemical staining results, treatment, and prognosis.
According to the diagnostic criteria for NB, we developed the following criteria for inclusion of patients in the study: an increase in urinary catecholamine metabolites, consistent with a primary or metastatic tumor determined by NB or pathologic features from a tissue biopsy, and NB cells were detected in bone marrow. Patient information was collected, including sex, age, clinical manifestations, laboratory tests, imaging studies, treatment, pathologic findings, and follow-up results. VIP was measured by immunohistochemical staining. From the year 1996 to 2006, a total of six cases of diarrheal NB were admitted to our hospital. All patients were boys. The minimum age at diagnosis was 1 year and the maximum age was 2 years 6 mo. Diarrhea occurred from the age of 9 mo to 2 years. The time from when diarrhea occurred to diagnosis ranged from 4 mo to 1 year. Loose or watery stools occurred 3-8 times each day, and routine fecal tests were normal. Drugs were ineffective. Diarrhea was the first symptom and was consistent in five cases, and abdominal tumors were identified by B-ultrasound.
Two patients underwent preoperative chemotherapy, in one case diarrhea stopped after 1 mo of chemotherapy, in the other patient, diarrhea was reduced and stopped after surgery. Three cases underwent surgery without preoperative chemotherapy, diarrhea stopped in two patients after surgery, and one patient died during surgery. One patient visited a doctor due to abdominal pain and a tumor was identified; diarrhea began after preoperative chemotherapy and the symptoms were obvious even after tumor resection. Water and electrolyte imbalance and malnutrition were difficult to correct and the patient died. The main characteristics were chronic dehydration, intractable hypokalemia, chronic malnutrition, and growth retardation. Potassium was as low as 1.3 mmol/L, and potassium supplementation by routine daily peripheral venous infusion was generally ineffective, and a high concentration of potassium infused intravenously was necessary. ECG monitoring was necessary in these patients to prevent cardiac arrest. Blood vessel leakage and skin necrosis occurred in one patient following the infusion of high concentrations of potassium via a peripheral vein. Although patients may adapt to chronic hypokalemia, correction of hypokalemia before surgery is necessary. One of the six cases, whose preoperative serum potassium was 2.8 mmol/L, was not cured, and cardiac arrest occurred during the operation; serum potassium at that time was 1.8 mmol/L. It is noteworthy that even if the preoperative serum potassium had been corrected (4.84 mmol/L), hypokalemia (1.8 mmol/L) would still have occurred during surgery, and serum potassium should be monitored frequently during surgery.
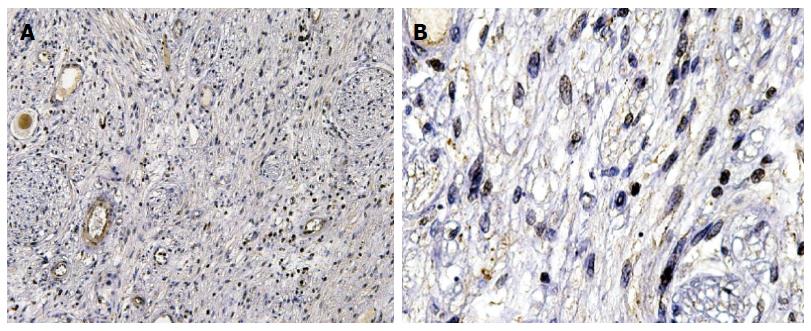
Of the six patients included in this study, the tumors were located in the adrenal gland in four cases, in the upper retroperitoneum in one case, and in the presacral area in one case. Pathologic findings were NB and ganglioneuroblastoma. Five patients were clinical stage I-II, and one case was stage III. Four patients survived (followed-up for 6 mo to 4 years). It is generally believed that diarrhea is related to VIP secretion by the tumor[4]. The immunohistochemical staining results are shown in Figure 1.
NB is the most common extracranial solid tumor in children, and the primary tumor can be located in any part of the sympathetic chain or the adrenal medulla[5]. The tumor most commonly occurs in the abdomen (75%), followed by the mediastinum (20%) and the neck (5%). Retroperitoneal NB is initially occult, leading to progression and a poor prognosis[6]. Due to a lack of B-ultrasound newborn screening, early identification of NB is mainly dependent on initial symptoms[7]. Fever[8], limb pain[9], abdominal mass, abdominal pain[10], and lower limb weakness are the most common clinical manifestations in the majority of patients. Patients with diarrhea as the main symptom, suggestive of diarrheal NB, are quite rare. Consequently, it is not easy to diagnose in the early stage of the disease.
Intractable diarrhea is due to the tumor secreting large amounts of VIP, and these children usually present with secretory diarrhea, hypokalemia, and achlorhydria[11]. VIP acts on the intestinal epithelial cells via the blood circulation, causing excessive secretion of intestinal fluid and promoting pancreatic juice and bile secretion, and further exacerbating the loss of water and electrolytes. Secretory diarrhea is the most obvious symptom of the disease, and our patients suffered from serious watery diarrhea that lasted a long time, and was not relieved even after 72 h of fasting, which led to the diagnosis. In 1952, Hawfield and Daisly reported a case of adrenal neuroblastoma with chronic diarrhea where the diarrhea stopped after removal of the tumor[12]. Other investigators also reported ganglioneuroma and ganglion NB with watery diarrhea, hypokalemia, and achlorhydria syndrome in 1973[13]. They detected high levels of VIP in the patients’ serum or tumor. Using peroxidase-anti-peroxidase staining assays, immunohistochemical methods, VIP serum level, and tumor tissue staining, they also found that the ganglion-like tumor cells were positive, but undifferentiated NB cells were negative.
VIP was first isolated in 1970 from pig small intestines[14]. It has been confirmed that the central nervous system and the sympathetic ganglion neurons are also rich in VIP. This peptide is composed of 28 amino acids and its main function is to dilate blood vessels, to inhibit histamine, which can stimulate gastric acid secretion resulting in achlorhydria, and stimulate the secretion of intestinal fluid resulting in excessive watery diarrhea. Normal amounts of VIP can be inactivated by the liver, and its physiologic function is insignificant. When ganglion cells proliferate, such as in tumors, and secrete excessive VIP, watery diarrhea syndrome occurs.
Some researchers have proposed the concept of “VIP secreting tumors”, and these tumors include pheochromocytoma, mast cell tumors, non-B cell hyperplasia, and medullary thyroid carcinoma. Refractory watery diarrhea in children is mainly due to high VIP levels in plasma. Such cases were first reported by Ghishan et al[15] in 1979. VIP secreting tumor-induced diarrhea is characterized by watery diarrhea, hypokalemia, and alkalosis (WDHA syndrome). This syndrome is most common in children aged one year to three years, and should be included in the differential diagnosis of pediatric chronic diarrhea.
In summary, diarrheal NB is a rare disease that is difficult to identify in the early stage. Patients aged 1-3 years who present with chronic intractable diarrhea should be followed closely. Intractable diarrhea, hypokalemia, and dysplasia are the initial clinical manifestations. An increased level of VIP is characteristic. Attention should be paid to potassium supplementation, which plays a vital role in the treatment procedure, especially preoperatively. In order to prevent sudden cardiac death, monitoring of electrolytes and ECG changes during surgery is important. The prognosis of diarrheal NB is good following appropriate treatment.
We thank Hong Qin, Wei Yang, Hai-Yan Cheng, and Xiao-Feng Chang for their technical assistance.
Intractable diarrhea, hypokalemia, and dysplasia are the initial clinical manifestations of diarrheal neuroblastoma.
All patients were boys who had 3-8 loose or watery stools each day, abdominal tumors, and normal routine fecal tests.
The differential diagnosis of patients aged 1-3 years who present with chronic intractable diarrhea should include diarrheal neuroblastoma.
Routine fecal tests were normal.
Abdominal tumors were identified by B-ultrasound in all cases.
Pathologic findings were neuroblastoma or ganglioneuroblastoma with positive immunohistochemical staining for vasoactive intestinal peptide.
Tumor resection and potassium supplementation play a vital role in the treatment procedure.
Such cases were first reported by Ghishan et al in 1979.
Patients aged 1-3 years who present with chronic intractable diarrhea should be followed closely and potassium supplementation plays a vital role in the treatment procedure, especially preoperatively.
This manuscript is very interesting. Diarrheal neuroblastoma is quite rare.
P- Reviewer: Kawai HF, Miyoshi E, Mullan MJ S- Editor: Yu J L- Editor: AmEditor E- Editor: Wang CH
| 1. | Ganeshan VR, Schor NF. Pharmacologic management of high-risk neuroblastoma in children. Paediatr Drugs. 2011;13:245-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Maris JM. Recent advances in neuroblastoma. N Engl J Med. 2010;362:2202-2211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1588] [Cited by in RCA: 1496] [Article Influence: 99.7] [Reference Citation Analysis (0)] |
| 3. | Mendelsohn G, Eggleston JC, Olson JL, Said SI, Baylin SB. Vasoactive intestinal peptide and its relationship to ganglion cell differentiation in neuroblastic tumors. Lab Invest. 1979;41:144-149. [PubMed] |
| 4. | Bourgois B, Boman F, Nelken B, Bonnevalle M, Turck D. [Intractable diarrhoea revealing a neuroblastoma hypersecreting the vasoactive intestinal peptide]. Arch Pediatr. 2004;11:340-343. [PubMed] |
| 5. | Gilshtein H, Peled Z, Grunner S, Fischer D, Kakiashvili E, Kluger Y. Ganglioneuroma of the adrenal gland: a rare tumor in a rare location. Case Rep Oncol. 2012;5:487-489. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Nzegwu MA, Aghaji A. Neuroblastoma occurring in a 38-year old Nigerian man: a rare finding. Rare Tumors. 2009;1:e15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Xia SY, Li R, Song SB, Liang FQ. [Diagnosis and surgical therapy of primary retroperitoneal neurogenic tumors]. Zhonghua Yi Xue Za Zhi. 2009;89:1567-1569. [PubMed] |
| 8. | Forgie SE, Robinson JL. Pediatric malignancies presenting as a possible infectious disease. BMC Infect Dis. 2007;7:44. [PubMed] |
| 9. | Wilson PE, Oleszek JL, Clayton GH. Pediatric spinal cord tumors and masses. J Spinal Cord Med. 2007;30 Suppl 1:S15-S20. [PubMed] |
| 10. | Chu CM, Rasalkar DD, Hu YJ, Cheng FW, Li CK, Chu WC. Clinical presentations and imaging findings of neuroblastoma beyond abdominal mass and a review of imaging algorithm. Br J Radiol. 2011;84:81-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Wildhaber B, Niggli F, Bergsträsser E, Stallmach T, Sacher P. Paraneoplastic syndromes in ganglioneuroblastoma: contrasting symptoms of constipation and diarrhoea. Eur J Pediatr. 2003;162:511-513. [PubMed] |
| 12. | Gera PK, Kikiros CS, Charles A. Chronic diarrhoea: a presentation of immature neuroblastoma. ANZ J Surg. 2008;78:218-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Bourdeaut F, de Carli E, Timsit S, Coze C, Chastagner P, Sarnacki S, Delattre O, Peuchmaur M, Rubie H, Michon J. VIP hypersecretion as primary or secondary syndrome in neuroblastoma: A retrospective study by the Société Française des Cancers de l’Enfant (SFCE). Pediatr Blood Cancer. 2009;52:585-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Balemba OB, Grøndahl ML, Mbassa GK, Semuguruka WD, Hay-Smith A, Skadhauge E, Dantzer V. The organisation of the enteric nervous system in the submucous and mucous layers of the small intestine of the pig studied by VIP and neurofilament protein immunohistochemistry. J Anat. 1998;192:257-267. [PubMed] |
| 15. | Ghishan FK, Soper RT, Nassif ED, Younoszai MK. Chronic diarrhea of infancy: nonbeta islet cell hyperplasia. Pediatrics. 1979;64:46-49. [PubMed] |