Published online Jan 14, 2015. doi: 10.3748/wjg.v21.i2.609
Peer-review started: May 16, 2014
First decision: June 18, 2014
Revised: June 22, 2014
Accepted: August 28, 2014
Article in press: August 28, 2014
Published online: January 14, 2015
Processing time: 246 Days and 24 Hours
AIM: To evaluate the efficacy of intraoperative endoscopic retrograde cholangio-pancreatography (ERCP) combined with laparoscopic cholecystectomy (LC) for patients with gall bladder stones (GS) and common bile duct stones (CBDS).
METHODS: Patients treated for GS with CBDS were included. LC and intraoperative transcystic cholangiogram (TCC) were performed in most of the cases. Intraoperative ERCP was done for cases with proven CBDS.
RESULTS: Eighty patients who had GS with CBDS were included. LC was successful in all cases. Intraoperative TCC revealed passed CBD stones in 4 cases so intraoperative ERCP was performed only in 76 patients. Intraoperative ERCP showed dilated CBD with stones in 64 cases (84.2%) where removal of stones were successful; passed stones in 6 cases (7.9%); short lower end stricture with small stones present in two cases (2.6%) which were treated by removal of stones with stent insertion; long stricture lower 1/3 CBD in one case (1.3%) which was treated by open hepaticojejunostomy; and one case (1.3%) was proved to be ampullary carcinoma and whipple’s operation was scheduled.
CONCLUSION: The hepatobiliary surgeon should be trained on ERCP as the third hand to expand his field of therapeutic options.
Core tip: The incidence of common bile duct stones (CBDS) in patents with gall bladder stones (GS) varies between 7% and 20%. Management of CBDS is changing with advances in endoscopic techniques in many regards. Laparoscopic cholecystectomy is the gold standard in treating GS. This has created controversies in the management of CBDS. The hepatobiliary surgeon should be trained in endoscopic retrograde cholangio-pancreatography as the third hand to expand his field of therapeutic options.
- Citation: El Nakeeb A, Sultan AM, Hamdy E, El Hanafy E, Atef E, Salah T, El Geidie AA, Kandil T, El Shobari M, El Ebidy G. Intraoperative endoscopic retrograde cholangio-pancreatography: A useful tool in the hands of the hepatobiliary surgeon. World J Gastroenterol 2015; 21(2): 609-615
- URL: https://www.wjgnet.com/1007-9327/full/v21/i2/609.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i2.609
The incidence of common bile duct stones (CBDS) in patients with gall bladder stones (GS) is 7 to 20%[1,2]. Laparoscopic cholecystectomy (LC) is the gold standard in treating GS (3). This has produced debates in the treatment of CBDS[3,4]. Many authors have tried to find an optimal option to manage combined CBDS and GS. Different options are available. All CBDS existing at the time of cholecystectomy should be extracted, since residual stones in the common bile duct (CBD) may cause subsequent hepatobiliary and pancreatic complications[4].
There are different options that exist for removal of CBDS, including preoperative endoscopic retrograde cholangiopancreatography (ERCP) before LC, laparoscopic common bile duct exploration, open CBD exploration and postoperative ERCP[2,5,6]. The use of preoperative ERCP has been argumentative[4]. Many studies found that 40%-90% performed a useless procedure due to passed stones, failed clearance of CBD, and retained stones despite its complications[7-13]. Postoperative ERCP avoids unnecessary examination but has a failure rate of 7%-14%[2,8,10]. LC with intraoperative ERCP and endoscopic sphincterotomy (ES) is an alternative technique for management of GS and CBDS[2,11,14].
Laparoscopic common bile duct exploration (LCBDE) is successful in removing the CBD stones in 80%-95% of cases but it is time consuming with a morbidity rate about 4%-16%[15,16]. However, the limitation of this technique is when there are multiple large or impacted ductal stones. It needs more laparoscopic skill and a longer learning curve is required for LCBDE[17-21].
ERCP is done mainly by physicians and radiologists, and rarely by surgeons. The wide use of laparoscopic surgery and the advances in technology and training made ERCP and intraoperative US important aids in the hands of experienced hepatobiliary surgeons[1-3]. The optimal treatment of CBDS is dependent on the skills of the surgical team and the availability of instruments and endoscopies at the hospital. The single procedure has advantages over the two step procedure[2].
This study was planned to evaluate intraoperative ERCP combined with LC for patients with GS and CBDS as regards the success rate and safety, and to show the importance of ERCP for the hepatobiliary surgeon.
Consecutive patients with GS and CBDS at the Gastroenterology Surgical Center, Mansoura University, Mansoura, Egypt, during the period from August 2011 through April 2013, were managed by a single step treatment combining laparoscopic cholecystectomy and intraoperative ERCP. After completion of LC in the same set, exclusion criteria included age older than 80 years, pregnancy, previous history of gastrectomy, or coagulopathy.
Informed consent was obtained from all patients to be included in the study, after explanation of the nature of the disease and possible treatment. The study was approved by the local ethical committee of our hospital.
All patients were subjected to careful history taking, clinical examination, and laboratory investigation including total serum bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT). Abdominal ultrasound was done for all cases to assess GB and CBD dilation and stones. Magnetic resonance cholangiography (MRCP) was done in some cases where US could not confirm the diagnosis. A preoperative and intraoperative prophylactic antibiotic (cefotax 1 g, iv) was given to all patients. Somatostatin was given routinely to all patients one hour before surgery (1 mL, sc) to prevent development of post ERCP pancreatitis.
Laparoscopic cholecystectomy was started in all cases using the standard 4-ports technique under general anesthesia. Intraoperative cholangiogram was performed by the transcystic route in all cases. When laparoscopic cholecystectomy was finished, we temporarily put in an intraabdominal drain and closed the ports and prepared for ERCP. ERCP was performed in the supine position or the semiprone position. Endoscopic sphincterotomy was done in all cases using an endoflex type double lumen sphincterotomy and both Terumo and Hydrajag wires. Removal of stones was done by balloon, dormia basket or mechanical lithotripsy in difficult cases. A completion cholangiogram was done to confirm freedom of the CBD from stones. Electrocautery probes were used to ensure haemostasis if there was suspicion of bleeding from the papillotomy.
The following items were recorded: difficulty of cannulation of the biliary tract using Freeman score [1 = one to five attempts (easy), 2 = six to 15 attempts (moderate difficult), 3 = more than 15 attempts (difficult), 4 = failed][22]; the need for precut for cannulation; total operative time; hospital stay; and cost. Any complications of the procedure were assessed using Cotton’s criteria: mild (2-3 d spent in hospital); moderate (4-10 d in hospital; or serious (more than 10 d in hospital or need surgical or radiological interference)[23].
The patients were followed up on postoperative day 7, and then at 1 mo and 3 mo after the operation. Patients were also seen at our clinic if they developed symptoms between follow-up visits. Follow up was done by clinical examination, serum bilirubin and abdominal ultrasound.
Statistical analysis of the data in this study was performed using SPSS software, version 17. For continuous variables, descriptive statistics were calculated and were reported as median. Categorical variables were described using frequency distributions
Eighty patients seen during the recruiting period, (20 men and 60 women) were eligible and entered the study. The median age was 32 years. All patients presented with abdominal pain and jaundice. The median preoperative bilirubin was 3.8 (range 0.4-10) mg (Table 1).
| Variables | Data |
| Age (yr) | 32 (18-59) |
| Sex | |
| Male | 20 (25) |
| Female | 60 (75) |
| Bilirubin (mg) | 3.8 (0.4-10) |
| AST (IU) | 99 (21-468) |
| ALT (IU) | 93 (24-1000) |
| CBD diameter (mm) | 11 (6-15) |
| Size of stones in CBD | |
| Mean size (mm) | 8 (5-17) |
Abdominal ultrasound revealed the presence of multiple GS in all patients. The median diameter of the CBD was 11 (6-15) mm (Table 1).
Laparoscopic cholecystectomy was successful in 79/80 cases (98.8%). Intraoperative transcystic cholangiogram (IOTC) was performed in 78 cases. IOTC was not performed in two cases due to failure of cannulation of the narrow cystic duct. It showed passed stones in four cases so ERCP was unnecessary for these cases.
ERCP was performed in 76 cases and was successful in 74 cases (97.3%). Failure of cannulation occurred in two cases (one case due to atrophic papilla, and another one due to juxta-diverticulum papilla). The cannulation was easy in 50/76 cases (65.8%) while precut was needed in 8 cases (10.5%) (Table 2).
| Variables | Data |
| Duration of operation (min) | 95 (75-200) |
| Hospital stay (h) | 19 (18-24) |
| Time to reach papilla (s) | 25 (20-45) |
| ERCP done | 76 (95) |
| ERCP not done (passed stone by TCC) | 4 (5) |
| Difficulty in cannulation | |
| Grade 1 | 50/76 (65.8) |
| Grade 2 | 24/76 (31.58) |
| Failure of cannulation | 2 (2.6) |
| Precut papillotomy | 8/76 (10.52) |
| Results | |
| ERCP with stone extraction | 64 (84.2) |
| Passed stone | 6 (7.9) |
| Short stricture lower end CBD with stone ES with stent | 2 (2.6) |
| Long stricture lower 1/3 CBD...treated by open hepaticojejunostomy | 1 (1.3) |
| Filling defect at the lower end biopsied... adenocarcinoma | 1 (1.3) |
| Failure of cannulation | 2 (2.6) |
| Method of stone extraction | |
| Balloon | 52/66 (78.8) |
| Basket | 4/66 (6.1) |
| Combined basket and balloon | 8/66 (12.1) |
| lithotripsy | 2/66 (3.1) |
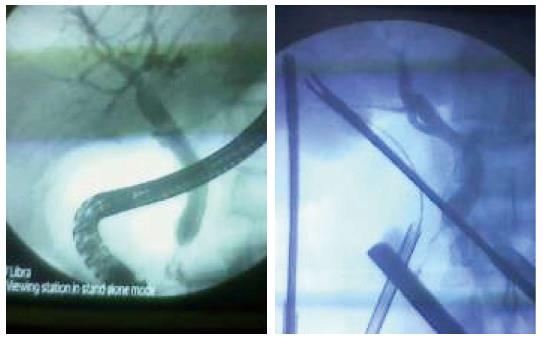
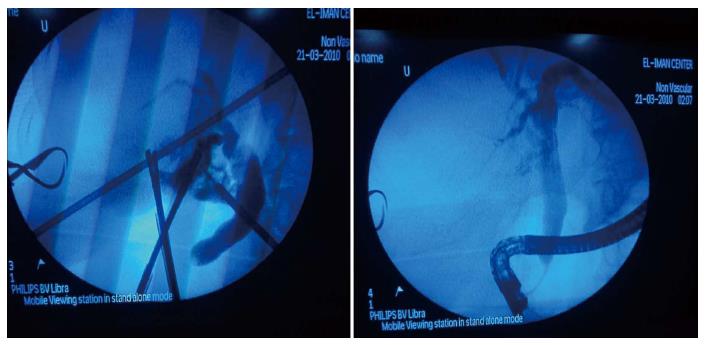
Intraoperative ERCP showed a dilated CBD with stones in 64 cases (84.2%) where removal of stones were successful. Six cases (7.9%) showed passed stones. A short lower end stricture with small stones presented in 2 cases (2.6%) who were treated by removal of stones with stent insertion and follow up CT (Figure 1). Postoperative CT was free and removal of the stent was done 1 mo later. Long stricture lower 1/3 CBD was found in 1 case (1.3%) and treated by open hepaticojejunostomy (Figure 2), and 1 case (1.3%) was proved to be ampullary carcinoma and whipple’s operation was scheduled (Figure 3, Table 2). Failure of cannulation occurred in 2 cases, (1 case due to atrophic papilla, and another case due to juxta-diverticulum papilla) and the decision was made to complete the two cases by laparoscopic CBD exploration.
Stone extraction was done by balloon in 56/66 cases (78.8%), by basket in 4/66 cases (6.1%), by combined balloon and basket in 8/66 cases (12.1%), and mechanical lithotripsy was needed in 2 cases (3.1%) that had large hard stones.
The median operative time was calculated for both maneuvers and found to be 95 (75-200) min. The postoperative course was smooth in all cases with no mortality. Melena occurred in 1 case due to peptic ulcer.
The complication rate after ERCP was 5/76 (6.6%) and took the form of bleeding papillotomy in 2 cases managed by side view endoscopy using electrocautery probe, hyperamylasemia in 2 cases and passed conservatively, and pancreatitis in 1 patient which was managed conservatively
The median hospital stay was 19 (18-24) h. The average net cost was $850 ($700-1350) for both maneuvers (Table 2).
All patients were followed up on postoperative day 7, 1 mo, and 3 mo postoperatively. No recurrent or residual stones were detected at these times.
The most popular methods of detecting CBDS include intraoperative cholangiography (IOC), intraoperative ultrasonography, ERCP, endoscopic ultrasonography, and MRC[4]. ERCP had its beginning in the late 1960s, with its introduction in the United States by McCune[24]. Endoscopic papillotomy and stone removal is successful in more than 90% of cases, with 5% morbidity and less than 1% mortality rate in expert hands[25]. Preoperative ERCP and ES is an effective option for removing CBDS in most cases, but only 10%-60% of patients will have stones on ERCP[1,6,8,9,26]. Even with strict selection criteria more than 10% of the preoperative ERCP are normal, and the possibility of occurrence of post-ERCP pancreatitis varies between 1%-13.5%[10,27-30]. Postoperative ERCP avoids undue trial but has a failure rate of 7%-14%[2,8,10].
Up till now ERCP has been mastered by either physicians or radiologists. The hepatobiliary surgical teams in our center have mastered ERCP, with more than 7000 procedures performed since 1991. So, we continuously have the availability to perform intraoperative ERCP (IO-ERCP) maneuvers.
ElGeidie et al[11] reported that LC and IO-ERCP is an available treatment for managing CBDS but it needs a well equipped hospital as regards endoscopies and a skillful surgical team. The success rate for IO-ERCP was 97.8%, the mean surgical time was 112 min, postoperative stay was 1.3 d and the morbidity rate was 4.5%.
LC and IO-ERCP is a single procedure for management of CBDS that decreases the hospital stay and costs. It also reduces unnecessary ERCP and decreases the need to return to the operating room following technical failure of ERCP. Ghazal et al[2] performed a study of 45 cases with GS and with a suspected or confirmed CBDS. Cholecystectomy was completed laparoscopically in 44 patients. The conversion rate was 1/45 due to marked adhesions at the Calot’s triangle. IOC was done in all cases and revealed CBDS in 36 cases. IO-ERCP with ES was performed successfully in 73.2% of patients. The mean surgical time was 119 min (ranging from 100 to 150 min). There was no postoperative morbidity related to the procedure and no evidence of retained CBDS on follow up[2].
DePalma et al[31] reported a 100% success rate in stone clearance with IO-ERCP in 15 cases, with a mean surgical time of 97.7 ± 30.4 min[31,32]. However, it needs organization to overcome the technical problems and to encourage the spread of this single procedure LC/ERCP[33]. It is difficult to assure the immediate availability of an endoscopist if stones are detected unexpectedly on IOC. This situation is time consuming and prolongs the operative times. The technical difficulties of the combined approach are related to both the supine position as more experience is required for successful cannulation of the papilla, and insufflation of gases[33].
In the present study the authors are surgeons who are experienced in both laparoscopy and ERCP; thus it is easy to secure an endoscopist if stones are detected unexpectedly on IOC immediately so the operative time in our study was shorter than other studies. Patients in our study were discharged after a mean hospital stay of 19 h (range 18-120 h). Williams and Vellacot[8] reported a hospital stay of 2.5 d, ranging from 1 to 5 d. Ghazal et al[2] reported that the mean hospital stay was 2.55 ± 0.89 d.
In our study some settings had been performed to solve the difficulties of IO-ERCP. It is technically more difficult to do ERCP in the supine position but it improves fluoroscopic visualization of hilar anatomy. We found that the position of the endoscope required for facing the papilla in the duodenum was somewhat different and was overcome by using specific techniques, such as clockwise rotation of the head of the endoscope or clockwise body rotation. To overcome the issue of intestinal distension, we perform LC and IOC first then after completion of LC we perform ERCP.
Single-stage LC/ERCP provides effective manage-ment for CBDS and may be helpful in selected patients who may not afford a second anesthetic maneuver[7]. Also, to increase the success rate of IO-ERCP, various rendezvous techniques were developed through the cystic duct[34]. Rabago et al[35] presented a prospective randomized study of LC with two different approaches: preoperative ERCP vs IO-ERCP for CBDS. Intraoperative ERCP was performed using a rendezvous technique.
A Swedish registry shows successful bile duct cannu-lation was achieved in 92% of the ERCPs performed. The presence of CBDS was seen in 36.8% of examinations. Perioperative and postoperative morbidities were 2.5% and 9.8%, respectively. The rate of ERCP-induced pancreatitis was 2.7%, and the hospital mortality rate was 5.9%[36].
In conclusion, hepatobiliary surgery is an expanding field of surgery. The hepatobiliary surgeon should be acquainted with operative ultrasound, endoscopy and ERCP as the third hand to expand his field of therapeutic options. This will limit the time loss in difficult biliary situations.
Surgeons have tried to find an optimal option to manage combined common bile duct (CBD) stones and gall bladder stones (GS). Different options are available. All CBD stones (CBDS) present at the time of cholecystectomy should be removed, since residual stones in the CBD may cause subsequent hepatobiliary and pancreatic complications. There are different options exist for removal of CBDS, including preoperative endoscopic retrograde cholangio-pancreatography (ERCP) before laparoscopic cholecystectomy (LC), laparoscopic common bile duct exploration, open CBD exploration and postoperative ERCP.
ERCP is performed mainly by physicians and radiologists, and rarely by surgeons. The wide use of laparoscopic surgery and the advances in technology and training make ERCP and intraoperative US important aids in the hands of the experienced hepatobiliary surgeon.
The optimal treatment of CBDS is dependent on the skills of the surgical team and availability of instruments and endoscopies at the hospital. There is no doubt that the single procedure has advantages over the two step procedure. This study was planned to evaluate intraoperative ERCP combined with LC for patients with GS and CBDS as regards the success rate and safety, and to show the importance of ERCP for the hepatobiliary surgeon.
The hepatobiliary surgeon should be trained in ERCP as the third hand to expand his field of therapeutic options.
This manuscript of “Intraoperative endoscopic retrograde cholangio-pancreatography, a useful tool in hands of hepatobiliary surgeon” is well written.
P- Reviewer: Yahav J S- Editor: Qi Y L- Editor: O’Neill M E- Editor: Ma S
| 1. | Mitchell SA, Jacyna MR, Chadwick S. Common bile duct stones: a controversy revisited. Br J Surg. 1993;80:759-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Ghazal AH, Sorour MA, El-Riwini M, El-Bahrawy H. Single-step treatment of gall bladder and bile duct stones: a combined endoscopic-laparoscopic technique. Int J Surg. 2009;7:338-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 56] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Uchiyama K, Onishi H, Tani M, Kinoshita H, Ueno M, Yamaue H. Timing of laparoscopic cholecystectomy for acute cholecystitis with cholecystolithiasis. Hepatogastroenterology. 2004;51:346-348. [PubMed] |
| 4. | Urbach DR, Khajanchee YS, Jobe BA, Standage BA, Hansen PD, Swanstrom LL. Cost-effective management of common bile duct stones: a decision analysis of the use of endoscopic retrograde cholangiopancreatography (ERCP), intraoperative cholangiography, and laparoscopic bile duct exploration. Surg Endosc. 2001;15:4-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 92] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Fletcher DR. Changes in the practice of biliary surgery and ERCP during the introduction of laparoscopic cholecystectomy to Australia: their possible significance. Aust N Z J Surg. 1994;64:75-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Coppola R, Riccioni ME, Ciletti S, Cosentino L, Ripetti V, Magistrelli P, Picciocchi A. Selective use of endoscopic retrograde cholangiopancreatography to facilitate laparoscopic cholecystectomy without cholangiography. A review of 1139 consecutive cases. Surg Endosc. 2001;15:1213-1216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Sarli L, Costi R, Gobbi S, Iusco D, Sgobba G, Roncoroni L. Scoring system to predict asymptomatic choledocholithiasis before laparoscopic cholecystectomy. A matched case-control study. Surg Endosc. 2003;17:1396-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Williams GL, Vellacott KD. Selective operative cholangio-graphy and Perioperative endoscopic retrograde cholangiopancreatography (ERCP) during laparoscopic cholecy-stectomy: a viable option for choledocholithiasis. Surg Endosc. 2002;16:465-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Barr LL, Frame BC, Coulanjon A. Proposed criteria for preoperative endoscopic retrograde cholangiography in candidates for laparoscopic cholecystectomy. Surg Endosc. 1999;13:778-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Bergamaschi R, Tuech JJ, Braconier L, Walsøe HK, Mårvik R, Boyet J, Arnaud JP. Selective endoscopic retrograde cholangiography prior to laparoscopic cholecystectomy for gallstones. Am J Surg. 1999;178:46-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | ElGeidie AA, ElEbidy GK, Naeem YM. Preoperative versus intraoperative endoscopic sphincterotomy for management of common bile duct stones. Surg Endosc. 2011;25:1230-1237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Neoptolemos JP, Davidson BR, Shaw DE, Lloyd D, Carr-Locke DL, Fossard DP. Study of common bile duct exploration and endoscopic sphincterotomy in a consecutive series of 438 patients. Br J Surg. 1987;74:916-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 62] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Stain SC, Cohen H, Tsuishoysha M, Donovan AJ. Choledo-cholithiasis. Endoscopic sphincterotomy or common bile duct exploration. Ann Surg. 1991;213:627-633; discussion 633-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 74] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Wright BE, Freeman ML, Cumming JK, Quickel RR, Mandal AK, Minn M. Current management of common bileduct stones: Is there a role for laparoscopic cholecystectomy and intraoperative endoscopic retrograde cholangiopancreatography as a single-stage procedure? Surgery. 2002;132:729-37. [RCA] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Clayton ES, Connor S, Alexakis N, Leandros E. Meta-analysis of endoscopy and surgery versus surgery alone for common bile duct stones with the gallbladder in situ. Br J Surg. 2006;93:1185-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 99] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 16. | Poulose BK, Arbogast PG, Holzman MD. National analysis of in-hospital resource utilization in choledocholithiasis management using propensity scores. Surg Endosc. 2006;20:186-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 17. | Rojas-Ortega S, Arizpe-Bravo D, Marín López ER, Cesin-Sánchez R, Roman GR, Gómez C. Transcystic common bile duct exploration in the management of patients with choledocholithiasis. J Gastrointest Surg. 2003;7:492-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 60] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Thompson MH, Tranter SE. All-comers policy for laparoscopic exploration of the common bile duct. Br J Surg. 2002;89:1608-1612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 77] [Article Influence: 3.3] [Reference Citation Analysis (1)] |
| 19. | Gholipour C, Shalchi RA, Abassi M. Efficacy and safety of early laparoscopic common bile duct exploration as primary procedure in acute cholangitis caused by common bile duct stones. J Laparoendosc Adv Surg Tech A. 2007;17:634-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Kharbutli B, Velanovich V. Management of preoperatively suspected choledocholithiasis: a decision analysis. J Gastrointest Surg. 2008;12:1973-1980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Wilcox CM. Should patients undergoing ERCP be placed in the prone or supine position? Nat Clin Pract Gastroenterol Hepatol. 2008;5:488-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [PubMed] |
| 23. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2035] [Article Influence: 59.9] [Reference Citation Analysis (1)] |
| 24. | McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of vater: a preliminary report. Ann Surg. 1968;167:752-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 410] [Cited by in RCA: 373] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 25. | Sivak MV Jr. Trained in ERCP (editorial)Training in advanced pancreaticobiliary endoscopy: Why, how, and will we even need ERCP in the future? Gastrointest Endosc. 2013;58:412-414. [RCA] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Lacaine F, Corlette MB, Bismuth H. Preoperative evaluation of the risk of common bile duct stones. Arch Surg. 1980;115:1114-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 82] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 27. | Erickson RA, Carlson B. The role of endoscopic retrograde cholangiopancreatography in patients with laparoscopic cholecystectomies. Gastroenterology. 1995;109:252-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 56] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Enochsson L, Lindberg B, Swahn F, Arnelo U. Intraoperative endoscopic retrograde cholangiopancreatography (ERCP) to remove common bile duct stones during routine laparoscopic cholecystectomy does not prolong hospitalization: a 2-year experience. Surg Endosc. 2004;18:367-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 72] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 29. | Andriulli A, Leandro G, Niro G, Mangia A, Festa V, Gambassi G, Villani MR, Facciorusso D, Conoscitore P, Spirito F. Pharmacologic treatment can prevent pancreatic injury after ERCP: a meta-analysis. Gastrointest Endosc. 2000;51:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 138] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 30. | Carr-Locke DL. Therapeutic role of ERCP in the management of suspected common bile duct stones. Gastrointest Endosc. 2002;56:S170-S174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 31. | De Palma GD, Angrisani L, Lorenzo M, Di Matteo E, Catanzano C, Persico G, Tesauro B. Laparoscopic cholecystectomy (LC), intraoperative endoscopic sphincterotomy (ES), and common bile duct stones (CBDS) extraction for management of patients with cholecystocholedocholithiasis. Surg Endosc. 1996;10:649-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Deslandres E, Gagner M, Pomp A, Rheault M, Leduc R, Clermont R, Gratton J, Bernard EJ. Intra-op endoscopic sphincterotomy for common bile duct stones during laparoscopic cholecystectomy. Gastrointest Endosc. 1993;9:54-58. [RCA] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 33. | Meyer C, Le JV, Rohr S, Thiry LC, Duclos B, Reimund JM, Baumann R. Management of common bile duct stones in a single operation combining laparoscopic cholecystectomy and perioperative endoscopic sphincterotomy. Surg Endosc. 1999;13:874-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 34. | Tekin A, Ogetman Z, Altunel E. Laparoendoscopic “rendezvous” versus laparoscopic antegrade sphincterotomy for choledocholithiasis. Surgery. 2008;144:442-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 35. | Rabago LR, Delgado M, de Vicente C, Moral I, Ventosa N, CASTro JL, Echarri JV, Llorente R, Romeo J, Gea F. Intraoperative ERCP for the Management of Choledocholithiasis: A Comparative Study. Gastrointestinal Endosc. 2004;59:199. [DOI] [Full Text] |
| 36. | Enochsson L, Swahn F, Arnelo U, Nilsson M, Löhr M, Persson G. Nationwide, population-based data from 11,074 ERCP procedures from the Swedish Registry for Gallstone Surgery and ERCP. Gastrointest Endosc. 2010;72:1175-1184, 1184.e1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 145] [Article Influence: 9.7] [Reference Citation Analysis (0)] |