Published online May 14, 2015. doi: 10.3748/wjg.v21.i18.5744
Peer-review started: November 19, 2014
First decision: December 26, 2014
Revised: January 19, 2015
Accepted: February 11, 2015
Article in press: February 11, 2015
Published online: May 14, 2015
Processing time: 180 Days and 22.1 Hours
Situs inversus viscerum (SIV) is a rare congenital condition characterized by complete transposition of all viscera. This anatomical pathology makes endoscopic retrograde cholangiopancreatography (ERCP) technically difficult. We report a new case of a 70-year-old Chinese male with total SIV who had obstructive jaundice. Magnetic resonance cholangiopancreatography demonstrated a number of stones in the gallbladder and common bile duct (CBD). Therapeutic ERCP was performed to relieve biliary obstruction and remove the CBD stones. This procedure started with the patient in a supine position and the endoscopist at the left side of the table. When the papilla was maintained, the patient was repositioned to a prone position and standard endoscopic sphincterotomy and endoscopic papillary balloon dilatation procedures were conducted. ERCP was performed successfully and relevant complications did not occur in this patient. We also present a review of the literature published between 1985 and 2014 in the PubMed and EMBASE databases. There were eight published cases during this period, with one each from America, Finland, India, Italy, South Korea and Pakistan, and two from Spain. Our case is the first reported in China.
Core tip: Endoscopic retrograde cholangiopancreatography (ERCP) is widely applied for the diagnosis and treatment of pancreaticobiliary disease. However, this approach can be challenging in cases of anatomical variations. Total situs inversus viscerum (SIV) is a rare condition that involves a 180° reversal of all the visceral positions, which increases the difficulty of ERCP. Endoscopic access to the papilla and subsequent cannulation are difficult in these patients. However, we successfully overcame these difficulties by changing the patient’s positions during the procedure. Standard endoscopic sphincterotomy and endoscopic papillary balloon dilatation procedures were performed with no complications. Herein, we also review several related cases with summary information, key steps and technique information for ERCP in patients with SIV.
- Citation: Hu Y, Zeng H, Pan XL, Lv NH, Liu ZJ, Hu Y. Therapeutic endoscopic retrograde cholangiopancreatography in a patient with situs inversus viscerum. World J Gastroenterol 2015; 21(18): 5744-5748
- URL: https://www.wjgnet.com/1007-9327/full/v21/i18/5744.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i18.5744
Situs inversus viscerum (SIV) is a rare congenital condition that occurs at a frequency of 1:5000 to 1:10000 live births. This condition is defined by a left-right transposition of all viscera as a mirror image[1]. In total SIV, there is complete transposition of all viscera and dextroposition of the heart and the liver is palpable in the left upper quadrant. This uncommon anatomy causes difficulties in the diagnosis and treatment of disease.
Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that can reveal the pancreaticobiliary tract clearly. Currently, this approach is widely applied for the extraction of common bile duct (CBD) stones due to its shorter operation time, reduced trauma and fewer complications. Therapeutic ERCP for bile duct stones has a success rate of 96% to 100%. However, this method can be technically challenging due to anatomic variations (such as Billroth I, Billroth II gastric resection, Roux-en-Y enteroanastomosis, SIV and duodenal papillary diverticula).
Herein, we report a case of successfully treated choledocholithiasis using endoscopic sphincterotomy (EST) and endoscopic papillary balloon dilatation (EPBD) in a 70-year-old male with total SIV. We also provide a review of related reports in the literature.
A 70-year-old patient with a history of coronary heart disease presented to our hospital in 2014 with left upper abdomen colicky pain that lasted six days and was associated with nausea, vomiting, fever (37.9 °C) and jaundice.
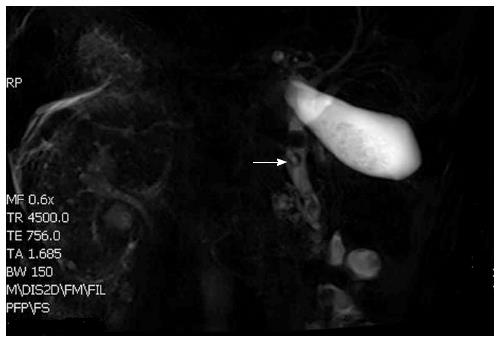
Physical examination revealed pronounced tenderness in the left upper abdomen. Laboratory studies showed that the percentage of neutrophils was 72.2%, alanine transaminase was 58 U/L, aspartate transaminase was 51 U/L, total bilirubin was 5.64 mg/dL, direct bilirubin was 3.97 mg/dL and gamma-glutamyl transpeptidase was 1150 U/dL. All other laboratory parameters (e.g., alkaline phosphatase) were in the normal range. A chest X-ray (Figure 1) and electrocardiogram confirmed dextrocardia. Magnetic resonance cholangiopancreatography demonstrated total SIV in the abdomen and multiple stones in the gallbladder and CBD, of which the largest was 1.3 cm in size (Figure 2).
A low-fat diet, energy supplements, liver-protecting treatment (glutathione 1.2 g per day) and magnesium sulfate injection (20 mL, once) were given to the patient before performing ERCP. After the operation, energy supplements, an octreotide acetate injection (0.3 mg in 0.9% sodium chloride 50 mL, Q12H) and a pantoprazole sodium injection (40 mg in 0.9% sodium chloride 100 mL, BID) were given to the patient. Five days after treatment, the patient’s temperature returned to normal and his pain was relieved. Therapeutic ERCP was performed on this patient after admission.
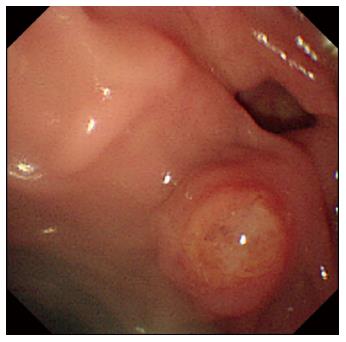
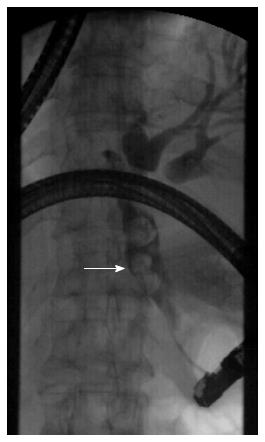
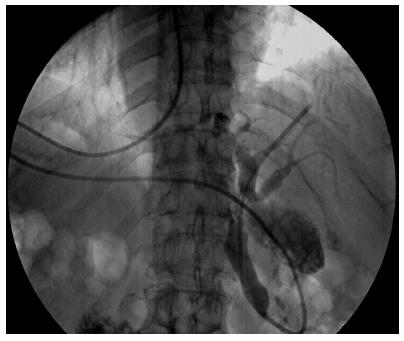
After premedication with scopolamine butylbromide (40 mg) and conscious sedation with propofol (100 mg), ERCP was performed with a side-viewing endoscope (Olympus JF-260). Initially, the patient was in a supine position, which is an unusual position for ERCP with the endoscopist standing at the left side of the patient who faced to the left. The duodenoscope was passed through the esophagus entrance and cardia depending on a breakthrough of feeling and landmarks, such as the Z-line and the transition to gastric mucosa. Then, the surgeon followed the direction of the gastric folds, allowing the duodenoscope to pass along the surface of the greater curvature of the stomach towards the antrum, according to the classic “setting sun” sign. The endoscope ultimately approached and traversed the pylorus and found the papilla at the descending part of the duodenum. At this time, three difficulties were encountered (discussed in the discussion section). Then, the patient was repositioned to a regular prone position. A similar method was used to arrive at the stomach. However, routine maneuvers became difficult in the second part of the duodenum; therefore, the endoscope was rotated clockwise to 180° with some torsion and shortening. Here, we observed a duodenal diverticulum with an ampulla on its edge (Figure 3). Cannulation was performed with a standard sphincterotome and jag wire measuring 450 cm × 0.035 inches (0.89 mm). Cholangiography showed that the biliary ducts had filling defects (Figure 4). A sphincterotomy was performed, although due to the diverticulum and altered CBD anatomy, the biliary orifice was located in the right upper quadrant, corresponding to the 1 o’clock position. After a standard sphincterotomy and balloon dilation, the stone was removed with a Dormia basket (Olympus FG-301Q Figure 5).
Postoperative laboratory results showed that the pancreatic enzyme levels were 197 U/L after 3 hours and 235 U/L after 24 h. The white blood cell count and the percentage of neutrophils were within the normal ranges. Postoperative pancreatitis and relevant complications did not occur in this patient. Five days later, the patient underwent another cholangiography which revealed no CBD stones (Figure 6). The patient was discharged after 6 d.
EST and stone extraction are standard procedures for the removal of CBD stones[2]. The left lateral or prone position, which is conducive to revealing the duodenal papilla and improving the success rate of cannulation, is the typical position for patients during ERCP. In some conditions, such as deep sedation with endotracheal anesthesia, cardiopulmonary dysfunction, massive ascites and extreme obesity, patients have difficulty in adopting this position and a supine position is therefore advocated[3]. Endoscopic access to the papilla and subsequent cannulation are the key steps of ERCP, which can be significantly affected by congenital or acquired anatomic alterations.
SIV is a congenital condition with complete transposition of all viscera. The side view endoscope is built for the right position of the liver with the papilla at the medial side of the duodenum in ERCP. However, these limitations of the device and anatomical variations make ERCP more challenging and difficult in patients with SIV. Other disorders, including Kartagener’s syndrome, primary ciliary dyskinesia, and asplenia or polysplenia syndrome, occur frequently in patients with SIV[4-6]; however, there is no evidence that SIV patients are more susceptible to CBD stones.
To date, eight cases of therapeutic ERCP in patients with SIV have been reported worldwide (Table 1). In 1985, Venu et al[7] first reported ERCP and endoscopic sphincterotomy in patients with SIV. Following intubation, the patient in this previous report was moved into several positions. In this way, the papilla could be identified and cannulation could be achieved with the endoscope in a straightened position. Some authors have reported similar cases in which ERCP was performed in other positions. In 1988, Nordback et al[8] successfully completed ERCP in patients with SIV and the authors found that the best position for cannulation was achieved when the endoscopist turned his right side towards the patient. CBD stones were observed and extracted with a Dormia basket after an endoscopic papillotomy was made toward the direction of “1 o’clock”. In 1997, Chowdhury et al[9] reported that a patient with SIV was placed in the usual left lateral position and the endoscopist was at the left side of the table at the beginning of ERCP. The endoscope was shortened by a 90° twist to the left and withdrawn; subsequently, standard EST was performed successfully. Fiocca et al[10] reported that ERCP was carried out successfully despite situs inversus requiring maintenance of the patient in a prone position with the endoscopist at the right side of the table. García-Fernández et al[11] performed ERCP in a patient with complete SIV using a “mirror image” technique. Three studies[12-14] reported in 2010 and 2014 indicated that a patient with SIV was placed in the usual prone position and the duodenoscope was turned 180° clockwise in the stomach; EST and removal of CBD stones were then performed. The case reported by Kamani et al[14] was similar to ours because this previous case also showed the same therapeutic ERCP pattern as patients with SIV and an ampullary diverticulum.
| Ref. | Country | Year | Patient’s position | Endoscopist’s position | Key steps | Complications |
| Venu et al[7] | United States | 1985 | Right lateral position → recumbent/prone position | At the right side of the table | Altered the patient's position several times before cannulation | No |
| Nordback et al[8] | Finland | 1988 | On her right in a prone position | Unknown | The endoscopist turned his right side toward the patient when cannulation was achieved and an endoscopic papillotomy was made toward the direction of "1 o'clock" | No |
| Chowdhury et al[9] | India | 1997 | Left lateral position | At the left side of the table | Minor modifications of the maneuvers and endoscope tip movement | No |
| Fiocca et al[10] | Italy | 2008 | Prone position | At the right side of the table | Passed the stomach and reached the duodenum with only a 180° turn | No |
| García-Fernández et al[11] | Spain | 2010 | Right lateral position | At the right side of the table | “Mirror image” ERCP technique:all necessary endoscopic maneuvers were performed inversely as per normal procedures | No |
| de la Serna-Higuera et al[12] | Spain | 2010 | Prone position | At the right side of the table | The duodenoscope had to be turned 180° clockwise in the stomach and a rotating sphincterotome was needed | No |
| Lee et al[13] | South Korea | 2010 | Prone position | At the right side of the table | The endoscope was rotated 180 to the right (in the stomach) and large-balloon dilation was performed after a limited sphincterotomy | No |
| Kamani et al[14] | Pakistan | 2014 | Left lateral position | At the right side of the table | Passed the stomach and reached the duodenum with a 180° turn | No |
In subjects with SIV, a mirror image of the normal anatomy makes it harder for endoscopists to gain access to duodenal papilla. From the eight cases reported, we found that most of the patients were placed in a left lateral position or prone position, which is the usual position in ERCP, and the endoscopist preferred to be at the right side of the operating table. Adjustments such as a 180° turn in the stomach or special techniques such as a “mirror imaging” were shown to contribute to maintenance of the duodenal papilla. No complications were reported in any of the previously reported cases.
In our case, because the position of the upper gastrointestinal tract and pancreaticobiliary duct is a mirror image of the normal anatomy, the endoscopist began intubation with the patient in a supine position. Following intubation, however, this technique became difficult for three reasons: first, the head could not be fixed easily in a natural position; second, cannulation was difficult when the papilla sank into the intestinal wall because of the effect of gravity and the diverticulum, which increased the difficulty of intubation and likelihood of papillary edema and damage to the pancreatic duct. In addition, the stomach could not be fixed for stability of the endoscope in the supine position. For these reasons, the patient was repositioned to a prone position with the face turned to the right and we completed the procedure with no complications. As described in other reports, a supine position was adopted for duodenoscopic examination because the anatomical view remains consistent; however, the traditional prone position, in which the endoscope needs be rotated clockwise 180°, can be applied for maintenance and cannulation in patients with SIV. We also found that cannulation is more difficult in patients with a periampullary diverticulum. To our knowledge, this case is the first reported in China.
In conclusion, therapeutic ERCP is a safe procedure for patients with SIV. However, ERCP can be performed more smoothly with conversion of the patient’s position or the use of special techniques. The major emphasis in ERCP for patients with SIV is adjusting the patient and endoscopist positions during the operation. Prior to achieving cannulation, the endoscopist may alter the patient’s position several times and perform alterations in scope positions.
A 70-year-old Chinese man presented with left upper abdomen colicky pain, fever and jaundice.
Obstructive jaundice.
Pancreatitis, pancreatic carcinoma, ampullary carcinoma and duodenal papillary carcinoma.
The percentage of neutrophils was 72.2%; alanine transaminase was 58 U/L; aspartate transaminase was 51 U/L; total bilirubin was 5.64 mg/dL; direct bilirubin was 3.97 mg/dL; and gamma-glutamyl transpeptidase was 1150 U/dL.
Chest X-ray and electrocardiogram results confirmed dextrocardia and magnetic resonance cholangiopancreatography revealed total situs inversus viscerum (SIV) in the abdomen and multiple stones in the gallbladder and common bile duct.
The patient underwent endoscopic retrograde cholangiopancreatography (ERCP) under general anesthesia.
Left upper abdomen colicky pain caused by choledocholithiasis with SIV is rare.
Total SIV is a rare condition with complete transposition of all viscera, including the heart, liver, spleen and stomach.
ERCP can be performed successfully in patients with total SIV by changing the patient’s position or adopting special techniques.
Lessons: In this study, we should have recorded the procedure in a video for additional medical data. Moreover, we also provided therapy to a similar patient but regrettably lost his record.
The authors report to us how to perform ERCP in a patient with situs inversus or SIV.
P- Reviewer: Ciaccio E, Lorenzo-Zuniga V, Reddy DN, Teoh AYB, Tomizawa M S- Editor: Ma YJ L- Editor: Roemmele A E- Editor: Ma S
| 1. | Gastrointestinal: situs inversus viscerum. J Gastroenterol Hepatol. 2002;17:1329. [PubMed] |
| 2. | Binmoeller KF, Schafer TW. Endoscopic management of bile duct stones. J Clin Gastroenterol. 2001;32:106-118. [PubMed] |
| 3. | Das A. Performing an ERCP with the patient in the supine position: necessity is the mother of improvisation. Gastrointest Endosc. 2008;67:1044-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Lee SE, Kim HY, Jung SE, Lee SC, Park KW, Kim WK. Situs anomalies and gastrointestinal abnormalities. J Pediatr Surg. 2006;41:1237-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 85] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Fonkalsrud EW, Tompkins R, Clatworthy HW. Abdominal manifestations of situs inversus in infants and children. Arch Surg. 1966;92:791-795. [PubMed] |
| 6. | Peeters H, Devriendt K. Human laterality disorders. Eur J Med Genet. 2006;49:349-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 126] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 7. | Venu RP, Geenen JE, Hogan WJ, Johnson GK, Taylor AJ, Stewart ET, Jackson A. ERCP and endoscopic sphincterotomy in patients with situs inversus. Gastrointest Endosc. 1985;31:338-340. [PubMed] |
| 8. | Nordback I, Airo I. ERCP and endoscopic papillotomy in complete abdominal situs inversus. Gastrointest Endosc. 1988;34:150. [PubMed] |
| 9. | Chowdhury A, Chatterjee BK, Das U, Dutta P, Dhali GK, Banerjee PK. ERCP in situs inversus: do we need to turn the other way? Indian J Gastroenterol. 1997;16:155-156. [PubMed] |
| 10. | Fiocca F, Donatelli G, Ceci V, Cereatti F, Romagnoli F, Simonelli L, Modini C. ERCP in total situs viscerum inversus. Case Rep Gastroenterol. 2008;2:116-120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | García-Fernández FJ, Infantes JM, Torres Y, Mendoza FJ, Alcazar FJ. ERCP in complete situs inversus viscerum using a “mirror image” technique. Endoscopy. 2010;42 Suppl 2:E316-E317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | de la Serna-Higuera C, Perez-Miranda M, Flores-Cruz G, Gil-Simón P, Caro-Patón A. Endoscopic retrograde cholangiopancreatography in situs inversus partialis. Endoscopy. 2010;42 Suppl 2:E98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Lee JH, Kang DH, Park JH, Kim MD, Yoon KT, Choi CW, Kim HW, Cho M. Endoscopic removal of a bile-duct stone using sphincterotomy and a large-balloon dilator in a patient with situs inversus totalis. Gut Liver. 2010;4:110-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Kamani L, Kumar R, Mahmood S, Jafri S, Siddiqui F. Therapeutic ERCP in patient with situs inversus totalis and ampullary diverticulum. J Coll Physicians Surg Pak. 2014;24:365-366. [PubMed] |