Published online Mar 28, 2015. doi: 10.3748/wjg.v21.i12.3619
Peer-review started: May 2, 2014
First decision: May 29, 2014
Revised: July 28, 2014
Accepted: October 15, 2014
Article in press: October 15, 2014
Published online: March 28, 2015
Processing time: 332 Days and 3.3 Hours
AIM: To investigate the utility of scintigraphic studies in predicting response to laparoscopic fundoplication (LF) for chronic laryngopharyngeal reflux symptoms.
METHODS: Patients with upper aero-digestive symptoms that remained undiagnosed after a period of 2 mo were studied with conventional pH and manometric studies. Patients mainly complained of cough, sore throat, dysphonia and globus. These patients were imaged after ingestion of 99m-technetium diethylene triamine pentaacetic acid. Studies were quantified with time activity curves over the pharynx, upper and lower oesophagus and background. Late studies of the lungs were obtained for aspiration. Patients underwent LF with post-operative review at 3 mo after surgery.
RESULTS: Thirty four patients (20 F, 14 M) with an average age of 57 years and average duration of symptoms of 4.8 years were studied. Twenty four hour pH and manometry studies were abnormal in all patients. On scintigraphy, 27/34 patients demonstrated pharyngeal contamination and a rising or flat pharyngeal curve. Lung aspiration was evident in 50% of patients. There was evidence of pulmonary aspiration in 17 of 34 patients in the delayed study (50%). Pharyngeal contamination was found in 27 patients. All patients with aspiration showed pharyngeal contamination. In the 17 patients with aspiration, graphical time activity curve showed rising activity in the pharynx in 9 patients and a flat curve in 8 patients. In those 17 patients without pulmonary aspiration, 29% (5 patients) had either a rising or flat pharyngeal graph. A rising or flat curve predicted aspiration with a positive predictive value of 77% and a negative predictive value of 100%. Over 90% of patients reported a satisfactory symptomatic response to LF with an acceptable side-effect profile.
CONCLUSION: Scintigraphic reflux studies offer a good screening tool for pharyngeal contamination and aspiration in patients with gastroesophageal reflux disease.
Core tip: Scintigraphic studies offer a good screening tool for patients with gastroesophageal reflux disease (GERD) who are suspected of laryngopharyngeal reflux (LPR) and lung aspiration. Such studies can predict the response to fundoplication. Although the application for this study was in a highly selected group who underwent fundoplication for LPR, the results have been equally valid in over 700 unselected patients with suspected GERD. The technique however requires careful attention to detail for acquisition parameters, particularly with the volume of liquid into which the tracer is introduced.
- Citation: Falk GL, Beattie J, Ing A, Falk S, Magee M, Burton L, Wall HVD. Scintigraphy in laryngopharyngeal and gastroesophageal reflux disease: A definitive diagnostic test? World J Gastroenterol 2015; 21(12): 3619-3627
- URL: https://www.wjgnet.com/1007-9327/full/v21/i12/3619.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i12.3619
Gastro-oesophageal reflux disease (GERD) has a number of protean manifestations that make it difficult to diagnose and treat. In 2006, the Montreal Consensus Group defined GERD as “a condition which develops when the reflux of stomach contents causes troublesome symptoms or complications”. The range of symptoms includes cough, sore throat and atypical chest pain and other apparent non-oesophageal symptoms. A proportion of patients may be asymptomatic even with significant acid reflux[1,2]. Furthermore, asymptomatic physiological episodes of GERD are a daily manifestation, further complicating the diagnosis[3].
While traditionally understood GERD (heartburn and regurgitation) is common, it has a different symptom profile to laryngopharyngeal reflux (LPR). The connection between GERD and LPR is however a contentious issue which has been canvassed in both the editorial format[4] and refereed publication[5]. These publications, especially the editorial by Spechler[4] rightly point out that not all chronic cough is due to GERD, as approximately half the patients treated for LPR do not have evidence of acid-reflux on pH monitoring[5]. We examined the connection between GERD and LPR in a small, selected population of patients referred for laparoscopic fundoplication as treatment for chronic cough and suspected pulmonary aspiration of refluxate. These patients had been carefully investigated and had established GERD by the standard criteria of pH and manometric studies. Detecting LPR and pulmonary aspiration are the two major blind spots of the accepted approach using pH and manometry, with some evidence that impedance studies may help with detecting LPR[6,7]. We examined the utility of scintigraphic reflux studies in the diagnosis of standard GERD, LPR and in the direct visualization of pulmonary aspiration of tracer during these studies.
Patients were extracted from a research database for either proven or suspected GERD which had been approved by the Institutional Ethics Committee (LNR/12 CRGH/248). Consecutive patients undergoing laparoscopic fundoplication for suspected LPR disease on the basis of abnormal pH/manometry studies was extracted from this database. All patients were considered if they had predominantly upper respiratory tract symptoms that remained undiagnosed after 8 wk of investigation by appropriate specialists. Major upper respiratory tract symptoms documented were cough, sore throat, recurrent throat clearing, voice change, laryngospasm, aspiration, globus and regurgitation. Any history of heartburn regurgitation and dysphagia was also elicited. Because of the severity of continuing extra-oesophageal symptoms despite full medical management and results of standard investigations for GERD as the likely cause of LPR, patients were surgically treated by fundoplication. This is therefore a highly selected group of patients with a high pre-test probability of GERD causing LPR and with a long history of undiagnosed upper respiratory tract symptoms. Patients were reassessed clinically at three months following surgery for the severity of symptoms and/ or the degree of improvement in symptoms. Clinical data was prospectively collected using a standardized proforma before and after surgery and entered into a database.
Scintigraphy, pH studies and manometry were repeated in 5 patients with recurrent symptoms post-operatively.
Ambulatory 24 h pH monitoring was performed using antimony crystal dual channel catheters (Medtronics, Synectics Medical, Minneapolis, Minnesota, United States) as described elsewhere. Data was recorded with a Digi trapper Mark III recorder (Medtronics, Synectics Medical) and analysed with the Synectics PW esophagram reflux analysis module (Medtronics, Synectics Medical). Abnormal proximal reflux was based on results of previous studies[8].
Stationary manometry was performed using a water perfused dent sleeve 8 channel catheter (Dent Sleeve International, Mississauga, Ontario, Canada) using standard techniques as described elsewhere. Data was recorded using a multichannel recording system (PC polygraph HR Medtronics, Synectics Medical, Minneapolis, Minnesota, United States) and analysed using PolyGram software program (Medtronics, Synectics Medical, Minneapolis, Minnesota, United States). Oesophageal motility was graded as normal, mildly, moderately or severely ineffective oesophageal motility modified from Kahrilas et al[9,10].
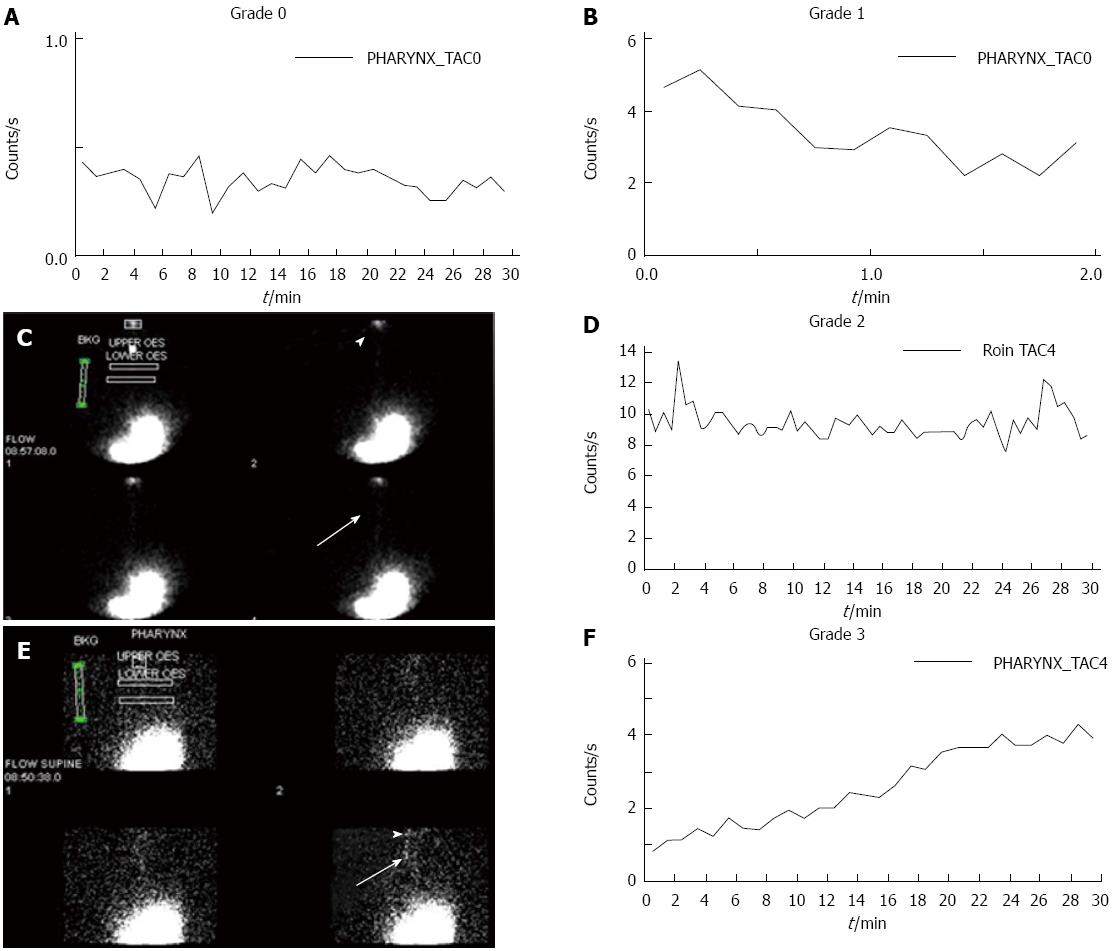
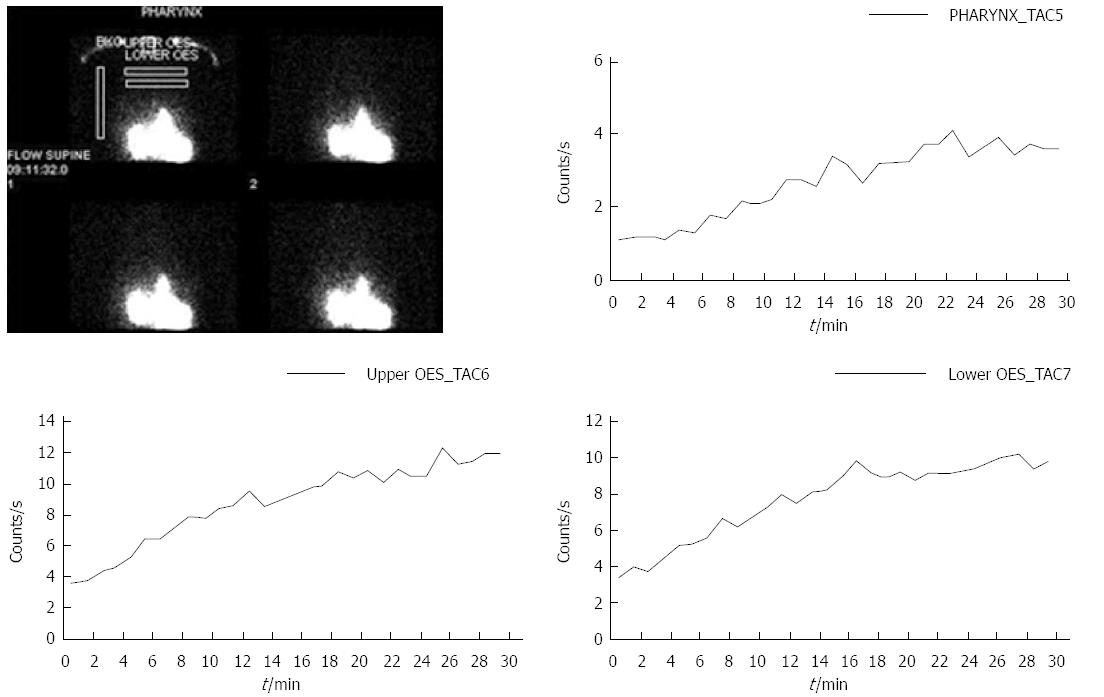
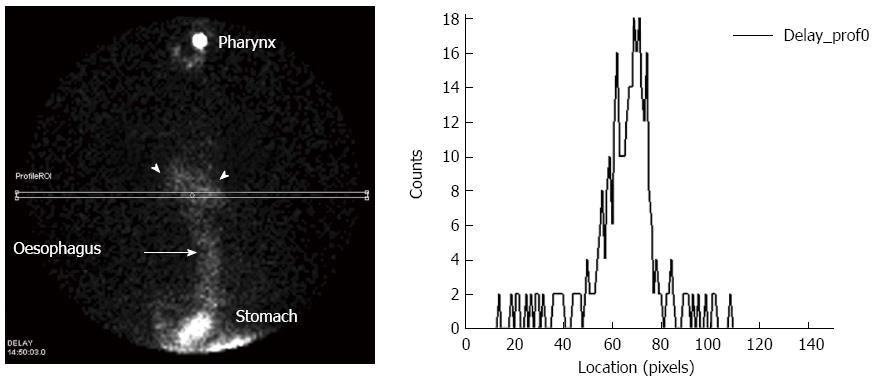
Patients were fasted overnight and medications were ceased for the 24 h prior to the test. While upright, patients were positioned in front of a Hawkeye 4 gamma camera (General Electric, Milwaukee, United States) with markers placed on the mandible and over the stomach to ensure the regions of interest were within the field of view of the camera. Patients swallowed 100-150 mL of water with 40-60 MBq of 99mTc DTPA followed by another 50 mL of water to clear the mouth and oesophagus of radioactivity. Dynamic images of the pharynx, oesophagus and stomach were obtained for 5 min at 15 s per frame into a 64 × 64 matrix. A second 30 min dynamic image was obtained in the supine position immediately following the upright study utilising 30 s frames. Following acquisition of the supine study, the patients were given a further 50 mL of water with 60 MBq of 99mTc phytate(colloid) followed by 50 mL of water as a flush. Delayed images were obtained at 2 h to assess the presence of aspiration of tracer activity into the lungs. Images were analysed by time activity curves over the pharynx, upper and lower half of the oesophagus and a background region over the right side of the chest, away from the stomach and oesophagus. Delayed images were analysed by a line profile over the lungs. Time activity curves were graded as showing no GERD, a falling curve, flat or rising curves. We defined the area under the curves (AUC) for the upper oesophagus and oropharynx after subtraction of the background level of activity as the Falk index.
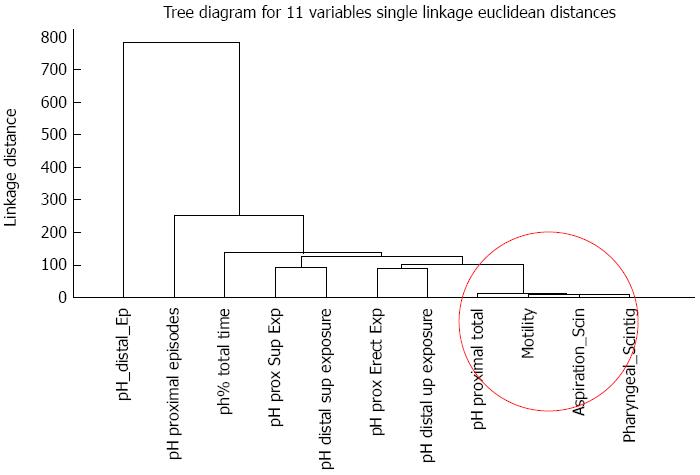
Data was analysed by nonparametric statistical methods as much of the analysis was of ordinal data with multiple studies for each patient. Standard ANOVA statistics, Wilcoxon matched pairs test and Pearson correlation coefficient (2 tails) with significance levels of 0.05 were utilised. Cluster analysis of the principal variables was also undertaken to evaluate linkages between 11 key variables. The Statistica V8 software (Statsoft, Oklahoma, United States) package was used for data analysis.
There were 34 patients (20 F, 14 M) with an average age of 57 years (range: 38-72 years). Proximal LPR symptoms were reported in 33 of 34 patients with one patient having no proximal symptoms, but severe heartburn and sinusitis. GERD was reported in 22 patients. Details of symptoms are provided in Table 1. Average duration of symptoms was 4.8 years (range: 0.5-22 years). All patients underwent laparoscopic fundoplication on the basis of symptoms, supporting tests and failure of best medical management (including double-dose proton pump inhibitor therapy).
| Symptoms | Total (n = 34) |
| GERD | 33 |
| Heartburn | 24 |
| Regurgitation | 23 |
| LPR | 33 |
| Chronic cough | 25 |
| Voice change | 15 |
| Throat clearing/aspiration | 11 |
| Sore throat | 10 |
| Globus | 5 |
| Laryngospasm | 2 |
Patients remained on anti-reflux medical therapy for six weeks post-operatively with cessation prior to the 3 mo review. At three months, total control of symptoms was reported in 27 (79%), partial in 4, giving overall improvement in 31 (91%). The rate of dysphagia was unchanged in 12 (44%). Occasional chest pain and bloating was present in 4, reduction in cough frequency in 1 and continued heartburn but eliminated cough in 1. Scintigraphy demonstrated low-grade reflux to the mid-oesophagus but not the pharynx in this patient. Reappearance of cough on stopping PPI occurred in 2 and no symptom resolution in 1 despite normalisation of scintigraphy and 24-h pH monitoring. Two patients were lost to review. Scintigraphy showed recurrent reflux to the pharynx in the 2 former patients and no evidence of reflux in the latter. The pH study was also normal in the latter patient.
Cough was the only significant symptom predicting pharyngeal contamination by scintigraphy (P = 0.047) and voice change predicted aspiration by scintigraphy (P = 0.038). All symptoms were strongly correlated with pharyngeal contamination by scintigraphy. Cough, laryngospasm and globus were strongly correlated with aspiration (scintigraphy). Change in voice was present in 15 patients, 11 demonstrated aspiration and 13 pharyngeal contamination by scintigraphy.
The 24 h pH studies were abnormal in all patients (Table 2). Episodes of reflux/24 h in the distal oesophagus were a mean of 128 and in the upper oesophagus, a mean of 31. The acid reflux exposure time distal was a mean of 16%, and 20% when supine. Reflux exposure time proximal was a mean 1.6%/24 h and 10.5% when supine. There were strong correlations between all symptoms and each of the proximal 24-h pH parameters. Strong correlations were found for heartburn, regurgitation and distal pH results. Strong correlations were found between severity of pH results and pulmonary aspiration by scintigraphy.
| pH studies | mean ± SD | Range | |
| Minimum | Maximum | ||
| pH distal episodes | 128.06 ± 91.41 | 8 | 356 |
| pH distal %total time | 16.04 ± 19.22 | 5.2 | 105 |
| pH distal erect exposure | 15.68 ± 18.72 | 4.2 | 102 |
| pH distal sup exposure | 20.10 ± 29.35 | 13 | 102 |
| pH proximal episodes | 31.30 ± 38.48 | 11 | 145 |
| pH proximal %total time | 1.59 ± 2.11 | 1 | 9.7 |
| pH prox erect exposure | 4.68 ± 17.65 | 0 | 102 |
| pH prox sup exposure | 10.52 ± 29.49 | 2 | 102 |
Lower oesophageal sphincter pressure had a mean ± SD of 2.94 ± 5.03 (normal > 18, range: 0-18 mmHg). Oesophageal motility was frequently abnormal and graded as severe IEM in 16, moderate IEM in 4, mild IEM in 5 and normal in 9. Highly significant correlations were found between impaired motility and pulmonary aspiration (P = 0.000063), episodes of reflux by scintigraphy (P = 0.000011), amplitude of reflux by scintigraphy (P = 0.0026) and the Falk index (AUC) (P = 0.000001).
There was evidence of pulmonary aspiration in 17 of 34 patients in the delayed study (50%). Pharyngeal contamination was found in 27 patients. All patients with aspiration showed pharyngeal contamination. In the 17 patients with aspiration, graphical time activity curve showed rising activity in the pharynx in 9 patients and a flat curve in 8 patients. In those 17 patients without pulmonary aspiration, 29% (5 patients) had either a rising or flat pharyngeal graph. A rising or flat curve predicted aspiration with a positive predictive value of 77% and a negative predictive value of 100%. There was a significant correlation between pharyngeal contamination and aspiration (P = 0.000). All patients in the cohort had evidence of gastro-oesophageal reflux by scintigraphy. Significant correlations were found for almost all pH studies and the isotope episodes, and amplitude of reflux in the oesophagus by scintigraphy (P < 0.01) but not for proximal supine acid exposure.
The hierarchical tree relationship between variables was expressed as a vertical icicle plot of the 11 variables (Figure 1) with single linkages using non-standardised Euclidean distances[11]. Tight linkages were shown between positive pharyngeal scintigraphy, aspiration by scintigraphy, manometric motility studies and impaired oesophageal motility, proximal total and exposure time.
When assessing patients for persistent upper respiratory tract symptoms (predominantly cough) and no cause is immediately apparent, there is accumulated clinical evidence to consider the possibility of LPR. However, approximately 30% of the population in one series of 2000 random cases had a score of over 10 in the reflux symptom index[12] with 75% also complaining of symptomatic GERD[13] (Figure 2). The task of assessing GERD in such a vast number of patients is problematic as there would be the need for a relatively invasive algorithm of endoscopy, pH/manometry/ impedance monitoring, ENT examination, respiratory function studies, amongst others. This would incur substantial costs and patient inconvenience. Endoscopy shows abnormalities in less than 50% of patients with reflux disease[14]. The presence of pepsin in saliva has shown promise as a surrogate marker of GERD that reaches the pharynx[15,16] but does not indicate lung aspiration of refluxate. A simple non-invasive test is required to assess the presence of significant full-column or proximal oesophageal reflux with potential for pharyngeal contamination and pulmonary aspiration of gastric contents. This particular standardised protocol for scintigraphy has the potential to be such an option.
Two channel 24 h pH monitoring provides a good measure of the frequency, severity and percentage of various aspects of acidic reflux. It may demonstrate full-column reflux rising to the level of the cricopharyngeus, and so a likelihood of pharyngeal contamination (Figure 3). However recent work using impedance studies has demonstrated that many patients suffer reflux which is not identified on pH monitoring but remains symptomatic and potentially damaging[17,18]. The pH study does not measure the presence of acid or non-acid material in the pharynx[19]. One clear advantage of reflux scintigraphy is that it measures any reflux to the level of the pharynx and the direct occurrence of pulmonary aspiration. It is not dependent upon measuring acid. A rising time-activity curve over the pharynx was demonstrably a good predictor of pulmonary aspiration in this group of patients. It very likely indicates continuing episodes of GERD combined with a failure of normal clearance mechanisms due to impaired motility. A flat pharyngeal time-activity curve may indicate a failure of pharyngeal clearance in the absence of repeated episodes of GERD into the pharynx. This relationship is reflected in the correlation between the manometric motility studies which measure ineffective oesophageal clearance of acid[10] and the presence of pulmonary aspiration on scintigraphy.
Upper aero-digestive symptoms and positive pharyngeal scintigraphy were strongly associated when analysed as paired variables on an individual patient basis. Cough, laryngospasm and globus were strongly correlated with positive aspiration scintigraphy. This suggests an aetiological role for the persistence of reflux (acid or weakly acidic/alkaline) fluid in the pharynx and subsequent aspiration into the respiratory tract (Figure 4). There is evidence that this may directly trigger the cough reflex[20] or lower the threshold for the cough reflex as indicated by C2 and C5 testing[21]. The concept of direct damage is supported by the findings in the 25 cases of chronic cough, where 14 cases had aspiration and 23 pharyngeal contamination by scintigraphy. The alternate theory of chronic cough mediated by afferent nerves in the distal oesophagus is also well supported in other studies[22]. There is no reason to suppose that both mechanisms are not separately operative in individual patients or indeed concurrent as there was no way to identify reflex-mediated patients. However, scintigraphic findings in the current study are not congruent with the concept of a reflex-mediated aetiology as the majority of the patients with cough, laryngospasm and globus had evidence of direct contamination of the pharynx and lungs. Perhaps reflex mediation may be more frequent in a less pathological group. The scintigraphic studies have shown a surprising degree of pulmonary aspiration (50%) in patients with cough. This may reflect the very highly and conservatively selected group of patients with long disease duration, likely to have more severe disease than in other reported series.
The ultimate test of the predictive value of reflux scintigraphic findings has been the symptomatic response to definitive surgical management by laparoscopic fundoplication. Resolution of laryngopharyngeal symptoms were found in 90% of cases. This supports the choice of patients for intervention based on the scintigraphic findings. It is no surprise that there has been a continuation of dysphagia in this patient group with a large percentage of oesophageal dysmotility. It is of course possible that there may have been a strong placebo effect within this patient group, which has been reported to be as high as 85% in chronic cough treated with pharmacological intervention such as opiates. However, opiates also have centralised effects upon cerebral neurotransmitters[23]. Surgical intervention in this situation is however more likely to have a response rate closer to 35%, which is generally accepted for the placebo effect[24]. The one patient that had no response to surgery had no definable reflux by pH monitoring or scintigraphy on follow-up. It does demonstrate the complexity of the disease where there may be a mixed pathology of both GERD and primary respiratory disease or a behavioral component. In a large multicentre study of laparoscopic fundoplication for GERD with 5 year follow-up in 1340 patients, symptoms were satisfactorily treated in 93% of patients[25]. More applicable to this study is a group of 47 patients reported over a six year period having laparoscopic fundoplication for the treatment of chronic cough[26]. Symptom relief was reported in 30 (64%) with a similar side-effect profile. The use of reflux scintigraphy may have yielded substantially better primary symptom management by improved selection as in our series.
Scintigraphic studies have been utilized to evaluate pulmonary aspiration in infants and children for many years, generally as tracer being instilled in milk which is administered at night with scanning the following morning[27,28]. These studies have been performed with low radiation exposure, often as low as single chest x-ray examinations and are considered safe and acceptable. Modifications of the technique have been shown to provide good results in the detection of GERD[29-32] and lung aspiration of refluxate[33,34]. Results in these series tend to vary with technical differences[29,31,35,36]. It appears that the volume of liquid in which the tracer is introduced into the stomach is important, as is the framing rate for study acquisition. The optimal volume is reported between 150 and 300 mL[29,31,32] and framing rates between 15 and 30 s, not 60 s which leads to significant reflux being missed[37]. Computer modeling and clinical data indicates that as little as 0.1 MBq of activity aspirated into the lung can be detected by the gamma camera[34]. There is some conflict in the reported reproducibility measures of visual interpretation vs analysis of time-activity curves. In one series, the computerised analysis was significantly better[38] while in another, visual interpretation was better[39]. These differences very likely reflect variations in the acquisition parameters. Importantly, reproducibility was good in both studies with kappa values greater than 0.70. Acquisition protocols in the current study were aligned with the technique of Caglar et al[38]. Two groups have reported good sensitivity and utility of the scintigraphic technique for the detection of laryngeal reflux and aspiration of tracer into the lungs[35,36]. The study of Bestetti et al[35] reported 201 patients with symptomatic posterior laryngitis documented by laryngoscopy and who were evaluated after administration of 300 mL of orange juice labeled with 99mTc. GERD was demonstrated by scintigraphy in 134 (67%), of which 78% was proximal and 31 patients were positive on scintigraphy for pulmonary aspiration. These findings are similar to the current report. Symptoms profiles were also similar between the study of Bestetti et al[35] and our group. Proximal symptoms in our group were tightly correlated with positive pharyngeal contamination. Cough was the only significant variable predicting positive pharyngeal contamination by multivariate analysis. Voice change was the only variable that predicted positive pulmonary aspiration by multivariate analysis. This finding has clinical importance. Our study showed good concordance for oesophageal scintigraphy with the 24 h pH and motility findings on an individual patient basis as paired studies. Other have reported less favourable results for scintigraphy (82% for pH studies vs 33% for scintigraphy)[31]. This may reflect a different and less severe patient sample. Technical difference may also have contributed to these disparate findings.
This study is relatively small and collected over a four year period. Such studies are time-consuming and invasive and patient compliance becomes a significant issue. The use of patient questionnaires raises the problem of the degree of placebo effect[40]. There were a large number of uncontrolled variables in the study and a high degree of patient variability, especially in the pH studies. A valid approach is therefore to consider these variable as dependant paired studies on an individual basis, as none of the variables were held constant. Cluster analysis was a valuable tool to assess a large number of variables and identify fundamental linkages between variables to get a sense of connectedness[11]. The finding of strong linkages between the motility studies, pH proximal total exposure time, pharyngeal and aspiration scintigraphy is reassuring.
The findings of the current study indicate that reflux scintigraphy utilising the current protocol is a potential screening tool for pharyngeal contamination and lung aspiration if GERD is suspected in patients with cough or other LPR symptoms. This requires further study in a more mixed and less selected group of patients. Subsequent assessment in over 700 patients has shown further utility in predicting response to surgical intervention and more importantly, factors that may predict surgical failure. The technique is simple, reproducible and has a low radiation exposure that is considered acceptable even in a pediatric population. The patient group with long-term LPR symptoms, especially cough and extensive investigation over a long time course can be selected for a high likelihood of symptomatic improvement by laparoscopic fundoplication. The combination of reflux scintigraphy, motility studies and two channel 24 h pH monitoring can increase the likelihood of success to over 90%. Patients with cough should therefore be assessed for pulmonary aspiration.
Gastroesophageal reflux disease (GERD) is a common occurrence which may however be asymptomatic and extend to laryngopharyngeal reflux (LPR) and lung aspiration of refluxate. Patients may not have symptoms of GERD but present with typical upper respiratory tract symptoms such as cough, dysphonia and globus. A high clinical index of suspicion is necessary to make the connection. Scintigraphy has the potential to screen for both LPR and lung aspiration.
Assessing LPR, lung aspiration and predicting the response to surgical therapy with laparoscopic fundoplication is the key to successful therapy. The necessary extension to this is discovering factors that predict failure of surgical therapy. Scintigraphic reflux studies have the potential to perform both tasks.
Impedance studies may prove to be reliable in the assessment of LPR as would salivary pepsin assays. The additive value to pH studies and high resolution manometry may prove to be decisive in the therapy of LPR.
Scintigraphy may prove to be a good predictor of successful laparoscopic fundoplication in terms of the presence of both LPR and lung aspiration of refluxate. More importantly it may be able to predict failure of surgery, especially in patients with co-existent gastroparesis. Post-operative assessment may provide important information regarding effectiveness of the fundoplication.
Scintigraphy uses the common isotope 99m Technetium which has a half-life of 6 h and a low radiation exposure at the doses being used. It is commonly bound to diethylene triamine pentaacetic acid which is frequently used in renal studies.
The true possible diagnostic role of scintigraphy in LPR might not be so straightforward as hypothesized, and will need more evaluations. Functional components to the symptoms may not be negligible in patients classified as having LPR, thus making more difficult a correct diagnosis, even in case of a positive scintigraphy test.
P- Reviewer: Contini S, Mittal SK S- Editor: Gou SX L- Editor: A E- Editor: Ma S
| 1. | Dickman R, Kim JL, Camargo L, Green SB, Sampliner RE, Garewal HS, Fass R. Correlation of gastroesophageal reflux disease symptoms characteristics with long-segment Barrett’s esophagus. Dis Esophagus. 2006;19:360-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Fass R, Dickman R. Clinical consequences of silent gastroesophageal reflux disease. Curr Gastroenterol Rep. 2006;8:195-201. [PubMed] |
| 3. | Richter JE. Typical and atypical presentations of gastroesophageal reflux disease. The role of esophageal testing in diagnosis and management. Gastroenterol Clin North Am. 1996;25:75-102. [PubMed] |
| 4. | Spechler SJ. Laryngopharyngeal reflux: a cause of faulty phonation or a faulted, phony diagnosis? Clin Gastroenterol Hepatol. 2006;4:431-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Vaezi MF. Laryngitis and gastroesophageal reflux disease: increasing prevalence or poor diagnostic tests? Am J Gastroenterol. 2004;99:786-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Yuksel ES, Vaezi MF. Therapeutic strategies for laryngeal manifestations of gastroesophageal reflux disease. J Clin Gastroenterol. 2013;47:195-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Smith JA, Abdulqawi R, Houghton LA. GERD-related cough: pathophysiology and diagnostic approach. Curr Gastroenterol Rep. 2011;13:247-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Dobhan R, Castell DO. Normal and abnormal proximal esophageal acid exposure: results of ambulatory dual-probe pH monitoring. Am J Gastroenterol. 1993;88:25-29. [PubMed] |
| 9. | Kahrilas PJ, Dent J, Dodds WJ, Hogan WJ, Arndorfer RC. A method for continuous monitoring of upper esophageal sphincter pressure. Dig Dis Sci. 1987;32:121-128. [PubMed] |
| 10. | Kahrilas PJ, Dodds WJ, Hogan WJ, Kern M, Arndorfer RC, Reece A. Esophageal peristaltic dysfunction in peptic esophagitis. Gastroenterology. 1986;91:897-904. [PubMed] |
| 11. | Ward JH, Jr . Hierarchical Grouping to Optimize an Objective Function. J Am Statistical Assoc. 1963;58:236-244. |
| 12. | Koufman JA, Aviv JE, Casiano RR, Shaw GY. Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg. 2002;127:32-35. [PubMed] |
| 13. | Kamani T, Penney S, Mitra I, Pothula V. The prevalence of laryngopharyngeal reflux in the English population. Eur Arch Otorhinolaryngol. 2012;269:2219-2225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 88] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 14. | Cantù P, Savojardo D, Carmagnola S, Penagini R. Impact of referral for gastro-oesophageal reflux disease on the workload of an academic Gastroenterology Unit. Dig Liver Dis. 2005;37:735-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Vaezi MF, Richter JE. Twenty-four-hour ambulatory esophageal pH monitoring in the diagnosis of acid reflux-related chronic cough. South Med J. 1997;90:305-311. [PubMed] |
| 16. | Vakil N. Salivary pepsin to diagnose GORD? Gut. 2015;64:361-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Sifrim D, Blondeau K, Mantillla L. Utility of non-endoscopic investigations in the practical management of oesophageal disorders. Best Pract Res Clin Gastroenterol. 2009;23:369-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Aanen MC, Bredenoord AJ, Samsom M, Smout AJ. Reliability of oesophageal pH recording for the detection of gastro-oesophageal reflux. Scand J Gastroenterol. 2008;43:1442-1447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Zerbib F, Roman S, Bruley Des Varannes S, Gourcerol G, Coffin B, Ropert A, Lepicard P, Mion F. Normal values of pharyngeal and esophageal 24-hour pH impedance in individuals on and off therapy and interobserver reproducibility. Clin Gastroenterol Hepatol. 2013;11:366-372. [PubMed] |
| 20. | Patterson RN, Johnston BT, Ardill JE, Heaney LG, McGarvey LP. Increased tachykinin levels in induced sputum from asthmatic and cough patients with acid reflux. Thorax. 2007;62:491-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 76] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 21. | Qiu Z, Yu L, Xu S, Liu B, Zhao T, Lü H, Qiu Z. Cough reflex sensitivity and airway inflammation in patients with chronic cough due to non-acid gastro-oesophageal reflux. Respirology. 2011;16:645-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Irwin RS. Chronic cough due to gastroesophageal reflux disease: ACCP evidence-based clinical practice guidelines. Chest. 2006;129:80S-94S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 186] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 23. | Eccles R. The powerful placebo in cough studies? Pulm Pharmacol Ther. 2002;15:303-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 105] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 24. | Beecher HK. The powerful placebo. J Am Med Assoc. 1955;159:1602-1606. [PubMed] |
| 25. | Pessaux P, Arnaud JP, Delattre JF, Meyer C, Baulieux J, Mosnier H. Laparoscopic antireflux surgery: five-year results and beyond in 1340 patients. Arch Surg. 2005;140:946-951. [PubMed] |
| 26. | Faruqi S, Sedman P, Jackson W, Molyneux I, Morice AH. Fundoplication in chronic intractable cough. Cough. 2012;8:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Collier BD. Detection of aspiration: scintigraphic techniques. Am J Med. 1997;103:135S-137S. [PubMed] |
| 28. | Maurer AH, Parkman HP. Update on gastrointestinal scintigraphy. Semin Nucl Med. 2006;36:110-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 71] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 29. | Kjellén G, Brudin L, Håkansson HO. Is scintigraphy of value in the diagnosis of gastrooesophageal reflux disease? Scand J Gastroenterol. 1991;26:425-430. [PubMed] |
| 30. | Russell C. Functional evaluation of the esophagus. The Esophagus Medical and surgical management. Philadelphia: WB Saunders 1988; 45. |
| 31. | Shay SS, Abreu SH, Tsuchida A. Scintigraphy in gastroesophageal reflux disease: a comparison to endoscopy, LESp, and 24-h pH score, as well as to simultaneous pH monitoring. Am J Gastroenterol. 1992;87:1094-1101. [PubMed] |
| 32. | Thomas EJ, Kumar R, Dasan JB, Kabra SK, Bal CS, Menon S, Malhothra A. Gastroesophageal reflux in asthmatic children not responding to asthma medication: a scintigraphic study in 126 patients with correlation between scintigraphic and clinical findings of reflux. Clin Imaging. 2003;27:333-336. [PubMed] |
| 33. | Ravelli AM, Panarotto MB, Verdoni L, Consolati V, Bolognini S. Pulmonary aspiration shown by scintigraphy in gastroesophageal reflux-related respiratory disease. Chest. 2006;130:1520-1526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 34. | Ruth M, Carlsson S, Månsson I, Bengtsson U, Sandberg N. Scintigraphic detection of gastro-pulmonary aspiration in patients with respiratory disorders. Clin Physiol. 1993;13:19-33. [PubMed] |
| 35. | Bestetti A, Carola F, Carnevali-Ricci P, Sambataro G, Tarolo GL. 99mTc-sulfur colloid gastroesophageal scintigraphy with late lung imaging to evaluate patients with posterior laryngitis. J Nucl Med. 2000;41:1597-1602. [PubMed] |
| 36. | Galli J, Volante M, Parrilla C, Rigante M, Valenza V. Oropharyngoesophageal scintigraphy in the diagnostic algorithm of laryngopharyngeal reflux disease: a useful exam? Otolaryngol Head Neck Surg. 2005;132:717-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 37. | Seymour JC, West JH, Drane WE. Sequential ten-second acquisitions for detection of gastroesophageal reflux. J Nucl Med. 1993;34:658-660. [PubMed] |
| 38. | Caglar M, Volkan B, Alpar R. Reliability of radionuclide gastroesophageal reflux studies using visual and time-activity curve analysis: inter-observer and intra-observer variation and description of minimum detectable reflux. Nucl Med Commun. 2003;24:421-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 39. | Tuncel M, Kıratlı PO, Aksoy T, Bozkurt MF. Gastroesophageal reflux scintigraphy: interpretation methods and inter-reader agreement. World J Pediatr. 2011;7:245-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 40. | Hróbjartsson A, Gøtzsche PC. Is the placebo powerless? Update of a systematic review with 52 new randomized trials comparing placebo with no treatment. J Intern Med. 2004;256:91-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 220] [Article Influence: 10.5] [Reference Citation Analysis (0)] |