Published online Dec 7, 2014. doi: 10.3748/wjg.v20.i45.17115
Revised: March 19, 2014
Accepted: May 29, 2014
Published online: December 7, 2014
Processing time: 376 Days and 13.5 Hours
AIM: To evaluate the feasibility and outcomes of laparoscopic Nissen fundoplication after failed transoral incisionless fundoplication (TIF).
METHODS: TIF is a new endoscopic approach for treating gastroesophageal reflux disease (GERD). In cases of TIF failure, subsequent laparoscopic fundoplication may be required. All patients from 2010 to 2013 who had persistence and objective evidence of recurrent GERD after TIF underwent laparoscopic Nissen fundoplication. Primary outcome measures included operative time, blood loss, length of hospital stay and complications encountered.
RESULTS: A total of 5 patients underwent revisional laparoscopic Nissen fundoplication (LNF) or gastrojejunostomy for recurrent GERD at a median interval of 24 mo (range: 16-34 mo) after TIF. Patients had recurrent reflux symptoms at an average of 1 mo following TIF (range: 1-9 mo). Average operative time for revisional surgical intervention was 127 min (range: 65-240 min) and all surgeries were performed with a minimal blood loss (< 50 mL). There were no cases of gastric or esophageal perforation. Three patients had additional finding of a significant hiatal hernia that was fixed simultaneously. Median length of hospitalization was 2 d (range: 1-3 d). All patients had resolution of symptoms at the last follow up.
CONCLUSION: LNF is a feasible and safe option in a patient who has persistent GERD after a TIF. Previous TIF did not result in additional operative morbidity.
Core tip: Even though transoral incisionless fundoplication (TIF) has been shown to be less invasive and has the hope of decreasing the symptoms of reflux. Laparoscopic Nissen still remains the gold standard. The paper highlights that some people can have persistent gastroesophageal reflux disease even after TIF and in these cases a Nissen, even though, technically challenging is feasible without any complications in experienced hands. We believe it fills the gap for a community based general surgeon to know how to take care of such patients as the number of such patients would continue to increase as more and more TIF is employed.
- Citation: Ashfaq A, Rhee HK, Harold KL. Revision of failed transoral incisionless fundoplication by subsequent laparoscopic Nissen fundoplication. World J Gastroenterol 2014; 20(45): 17115-17119
- URL: https://www.wjgnet.com/1007-9327/full/v20/i45/17115.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i45.17115
Gastroesophageal reflux disease is a pathology of significant prevalence, with an estimated 10%-20%[1-4] of the United States population experiencing symptoms weekly. The resultant morbidity of such a widespread condition has under-recognized implications on the health of populations and healthcare expenditures. Though medical management can be effective, symptomatic relief is dependent upon long-term therapy and adequate compliance[5]; approximately 10%-40% of patients have refractory symptoms[6,7].
The significant numbers of patients who are refractory to medical therapy undergo interventions that alter gastroesophageal anatomy to address the underlying mechanisms responsible for pathologic reflux: transient lower esophageal sphincter relaxations (TLESRs), a hypotensive lower esophageal sphincter, and anatomic disruption of the gastroesophageal junction. In the past decade, transoral incisionless fundoplication (TIF)[8-13] has been employed as a less-invasive alternative to Nissen fundoplication, a surgical procedure known to be effective in refractory gastroesophageal reflux disease (GERD).
TIF is performed using an endoscopic plication device that circumferentially deploys polypropylene fasteners to create a neogastro-esophageal valve after invaginating the lower esophagus into the gastric fundus. The lengthened esophageal gastric junction (EGJ) has been found to reduce the number of post-prandial TLESRs and decrease EGJ distensibility, resulting in improvement in liquid-containing reflux while maintaining the ability to vent gastric air. The largest multi-center prospective study to-date (n = 86) reported 56% of patients were cured of GERD based on symptom reduction and discontinuation of PPIs[14]. Esophageal acid exposure was decreased in 61% percent of patients, and the study reported a significant increase in mean LES pressure from 12 to 18 mmHg; 81% of patients achieved complete cessation of proton pump inhibitors after 12 mo.
Even though initial studies have shown promise, a few series have also reported substantial treatment failure rate[15-18]. Such patients develop recurrent/persistent GERD after TIF and are considered for further antireflux surgeries. In these instances, laparoscopic Nissen fundoplication (LNF) is the next recommended intervention, but becomes technically more challenging due to deranged anatomical variation secondary to endoscopic alterations, and may potentially lead to increased complications[19].
In the context of preliminary outcomes considerably different from primary LNF, further data is needed in order to provide patients accurate counseling in the risks and benefits of undergoing a technically challenging LNF after TIF. The purpose of this study was to evaluate the feasibility and outcomes of laparoscopic Nissen fundoplication after failed TIF at our institution.
All patients from 2010 to 2013 who underwent revisional antireflux surgery after a previous TIF and had persistent objective evidence of recurrent GERD were included. Recurrent or persistent disease was determined if patients had chronic GERD (> 6 mo) hypotonic or lower esophageal sphincter (< 30 mmHg), presence of a pathologic 24 h esophageal pH monitoring.
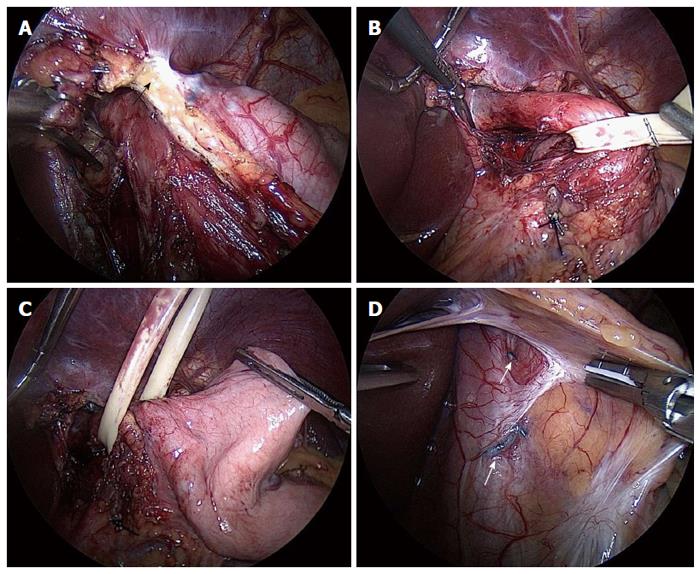
Patients subsequently underwent a LNF or a laparoscopic gastrojejunostomy by a qualified surgeon experienced in the procedure. Where appropriate, all LNFs involved entire mobilization of the prior TIF fundoplication(Figure 1A), mobilization of the esophagus with at least 3 cm within the abdominal cavity (Figure 1B), mobilization of the gastric fundus (Figure 1C), posterior closure of the crura and a 360° fundoplication resulting in at least a 3 cm wrap. Patients were followed for resolution of symptoms, and primary outcome measures included operative time, blood loss, length of hospital stay and complications encountered.
In 4 years, a total of 5 patients underwent revisional surgery due to persistent/recurrent GERD. 4 patients underwent revisional LNF and one underwent laparoscopic gastojejunostomy at a median interval of 24 mo (range; 16-30 mo). Sixty percent (n = 3) of the patients were males, with a median age of 57 (38-71) years, and a median BMI of 23.7 (23.1-27.8) kg/m2.Three of the patients developed recurrence of symptoms within one month following TIF, with the remaining two patients remaining at 5 and 9 mo.
The median operative time for revisional fundoplication was 98 min (range: 65-240 min). Three patients had an additional finding of a sliding hiatal hernia that was fixed simultaneously. One patient was found to have TIF fasteners placed superior to the gastroesophageal junction that had partially disrupted, as well as fasteners that were visible under the serosa of the stomach (Figure 1D). One patient that underwent gastrojejunostomy did so because of her history of open fundoplication followed by TIF previously. She had persistent dysphagia that resulted in her TIF being taken down in conjunction with resection of the fundus so a repeat fundoplication was not an option.
The revisional LNF was performed after taking down the adhesions from TIF and full mobilization of the prior fundoplication. A 3cm wrap was performed in all patients, and crural closure was ensured. Hiatal hernia where present was reduced simultaneously. One patient with a large hiatal hernia for which mesh was placed for reinforcement of the crural closure.The median operative blood loss was 50 mL (range: 30-50 mL). There were no cases of gastric or esophageal perforation.A median length of hospitalization was 2 d (range: 1-3 d) and were discharged after they tolerated a post Nissen/mechanical soft diet. Median follow up was 1 mo (range: 1-6 mo) at which point none of the patients had persistence of reflux symptoms.
An estimated 2/3rd of patients with non-erosive reflux disease will relapse with discontinuation of PPIs[20]; with nearly all patients relapsing with erosive disease[21]. Additionally, as an estimated 40% of patients have symptoms of GERD unresponsive to PPIs[22], definitive treatments for GERD will likely remain an area of investigation. Current evidence[23] suggests that laparoscopic Nissen fundoplication is superior to medical management for patients with normal esophageal length and motility, with 98% of patients cured of symptoms after 3-mo follow up. The procedure is however associated with 7% morbidity, primarily new-onset dysphagia. TIF is one of several techniques recently developed to provide a less-invasive definitive treatment for the millions of patients refractory to medical management.
Recent literature regarding TIF outcomes report inferior resolution of symptoms in comparison to LNF. A review of 15 published studies on TIF in 2013 reported overall patient satisfaction of 72%, PPI discontinuation in 67% of patients, a major complication rate of 3.2%, and a failure rate of 7.2%[24]. The largest prospective study of TIF outcomes (n = 84)[14] reported two instances of esophageal perforation upon device insertion, and one case of postoperative intraluminal bleeding. Another study following 38 patients also reported one case of intraluminal bleeding[18]; 36% of these patients also chose to undergo a revisional LNF. Mortality has not been reported to date.
The relatively high failure rates of TIF in comparison to LNF indicate that a subset of refractory patients will eventually seek revisional procedures. Only three studies have been published assessing the outcomes of revisional LNF. An early study from the Netherlands in 2010[19] identified 11 patients who underwent LNF from 88 patients who underwent TIF. Three of these patients were found to have complete disruption of fasteners; another five patients had partial disruptions. Following revision, all patients had normalized esophageal acid exposure, but there was not a significant improvement on the quality of life, primarily associated with dysphagia refractory to dilation in three patients. Complications included two instances of gastric perforation, one conversion to an open procedure, and the development of a sub-phrenic abscess in one patient requiring surgical exploration.
A subsequent publication from the Netherlands followed 15 patients who underwent revisional laparoscopic anti-reflux surgery from a cohort of 43 patients who received a TIF at their institution[25]. Seventy-six percent of these patients had disruption of TIF fasteners; all revisional procedures were performed laparoscopically without a need to convert to an open surgery. There was one reported instance of gastric perforation during dissection of the endoscopic fundoplication. Similar with the previous study, dysphagia occurred in 33% of patients; 27% required one or more pneumo-dilations for their symptoms. While there was a statistically significant improvement in quality-of-life measures in comparison to baseline, significance was not achieved when comparing post-TIF and post-revisional LNF scores.
A recent study by Perry et al[26] evaluated outcomes pertaining to the safety of performing a revisional procedure; 66 TIF patients were followed, 7 of whom underwent a LNF. Two of these patients had persistent symptoms immediately after TIF, while the remaining five developed recurrent symptoms between 5 and 33 mo. All patients were found to have partially dislodged TIF fasteners (Figure 1D), with one patient noted to have a significant hiatal hernia. There were no instances of gastric or esophageal perforations. Median operative time was 97 (48-122) min, with an estimated blood loss of 10 (0-50) mL. All patients were discharged on the first post-operative day.
All of these studies documented technically challenging revisional operations involving significant lysis of adhesions, which were implicated in the reported instances of gastric perforations and conversions to open surgeries. Our intra-operative findings were in concordance, but as was concluded by Perry et al[26], the absence of operative complications in our patients would suggest that revisional LNF can be safely performed in experienced hands. Additionally, the higher rates of dysphagia and the inferiority of symptom resolution in comparison to primary LNF were not observed in our patients.
Disrupted TIF fasteners were also observed in our patients, which is in agreement with these previous studies that have proposed disruption as the primary mechanism of TIF failure. There is no literature describing how this disruption occurs, which may be associated with inadequate endoscopic technique or a limitation of the device itself. However, significant hiatal hernias were present in 3 of our 5 patients, which may suggest that there are potentially identifiable anatomical variables that are predictive of fastener disruption and/or TIF failure.
Our study is limited by the small number of patients, and the short duration of follow-up. However, it is one of the two studies that has been done on this issue and reported in the United States. Larger studies following patients post-TIF are certainly warranted to adequately counsel patients on the potential benefits and adverse outcomes of undergoing a revisional laparoscopic intervention. Our findings have led us to conclude that revisional LNF under an experienced surgeon is a feasible and safe option in a patient who has persistent GERD after a TIF, without additional risk of operative morbidity.
Gastroesophageal reflux disease (GERD) is pathology of significant prevalence, with an estimated 10%-20% of the United States population. Transoral incisionless fundoplication (TIF) has been employed as a less-invasive alternative be effective in refractory GERD and few series have also reported substantial treatment failure rate.
To outline the feasibility and safety of laparoscopic Nissen fundoplication following transoral incisionless fundoplication.
TIF is associated with persistent GERD in few subset of patients. Even though the results of TIF failure cannot be generalized, patients do explore other option. Laparoscopic Nissen has been the gold standard treatment for managing GERD even in patients who have had other antireflux procedures. In expert hands, it can be done without any major morbidity or mortality.
Patients with persistent GERD after TIF should undergo Nissen fundoplication by experienced people in high volume centers.
The numbers presented in this study are very small so care must be taken before generalizing these results. More studies need to be conducted to evaluate more options after failed TIF.
P- Reviewer: Agresta F, Chan KWE, Fernandez-Pineda I, Prasad A S- Editor: Gou SX L- Editor: A E- Editor: Liu XM
| 1. | Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2013;108:308-328; quiz 329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1136] [Cited by in RCA: 1119] [Article Influence: 93.3] [Reference Citation Analysis (0)] |
| 2. | Agréus L, Svärdsudd K, Talley NJ, Jones MP, Tibblin G. Natural history of gastroesophageal reflux disease and functional abdominal disorders: a population-based study. Am J Gastroenterol. 2001;96:2905-2914. [PubMed] |
| 3. | Fedorak RN, Veldhuyzen van Zanten S, Bridges R. Canadian Digestive Health Foundation Public Impact Series: gastroesophageal reflux disease in Canada: incidence, prevalence, and direct and indirect economic impact. Can J Gastroenterol. 2010;24:431-434. [PubMed] |
| 4. | Frank L, Kleinman L, Ganoczy D, McQuaid K, Sloan S, Eggleston A, Tougas G, Farup C. Upper gastrointestinal symptoms in North America: prevalence and relationship to healthcare utilization and quality of life. Dig Dis Sci. 2000;45:809-818. [PubMed] |
| 5. | Ip S, Chung M, Moorthy D, Yu WW, Lee J, Chan JA, Bonis PA, Lau J. Comparative effectiveness of management strategies for gastroesophageal reflux disease: Update [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US) 2011; 11-EHC049-E. [PubMed] |
| 6. | Inadomi JM, McIntyre L, Bernard L, Fendrick AM. Step-down from multiple- to single-dose proton pump inhibitors (PPIs): a prospective study of patients with heartburn or acid regurgitation completely relieved with PPIs. Am J Gastroenterol. 2003;98:1940-1944. [PubMed] |
| 7. | Carlsson R, Dent J, Watts R, Riley S, Sheikh R, Hatlebakk J, Haug K, de Groot G, van Oudvorst A, Dalväg A. Gastro-oesophageal reflux disease in primary care: an international study of different treatment strategies with omeprazole. International GORD Study Group. Eur J Gastroenterol Hepatol. 1998;10:119-124. [PubMed] |
| 8. | Jobe BA, O’Rourke RW, McMahon BP, Gravesen F, Lorenzo C, Hunter JG, Bronner M, Kraemer SJ. Transoral endoscopic fundoplication in the treatment of gastroesophageal reflux disease: the anatomic and physiologic basis for reconstruction of the esophagogastric junction using a novel device. Ann Surg. 2008;248:69-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Demyttenaere SV, Bergman S, Pham T, Anderson J, Dettorre R, Melvin WS, Mikami DJ. Transoral incisionless fundoplication for gastroesophageal reflux disease in an unselected patient population. Surg Endosc. 2010;24:854-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Ihde GM, Besancon K, Deljkich E. Short-term safety and symptomatic outcomes of transoral incisionless fundoplication with or without hiatal hernia repair in patients with chronic gastroesophageal reflux disease. Am J Surg. 2011;202:740-746; discussion 746-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 11. | Narsule CK, Burch MA, Ebright MI, Hess DT, Rivas R, Daly BD, Fernando HC. Endoscopic fundoplication for the treatment of gastroesophageal reflux disease: initial experience. J Thorac Cardiovasc Surg. 2012;143:228-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Nguyen A, Vo T, Nguyen XM, Smith BR, Reavis KM. Transoral incisionless fundoplication: initial experience in patients referred to an integrated academic institution. Am Surg. 2011;77:1386-1389. [PubMed] |
| 13. | Velanovich V. Endoscopic, endoluminal fundoplication for gastroesophageal reflux disease: initial experience and lessons learned. Surgery. 2010;148:646-651; discussion 651-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Cadière GB, Buset M, Muls V, Rajan A, Rösch T, Eckardt AJ, Weerts J, Bastens B, Costamagna G, Marchese M. Antireflux transoral incisionless fundoplication using EsophyX: 12-month results of a prospective multicenter study. World J Surg. 2008;32:1676-1688. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 110] [Article Influence: 6.9] [Reference Citation Analysis (1)] |
| 15. | Cadière GB, Van Sante N, Graves JE, Gawlicka AK, Rajan A. Two-year results of a feasibility study on antireflux transoral incisionless fundoplication using EsophyX. Surg Endosc. 2009;23:957-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 16. | Hoppo T, Immanuel A, Schuchert M, Dubrava Z, Smith A, Nottle P, Watson DI, Jobe BA. Transoral incisionless fundoplication 2.0 procedure using EsophyX™ for gastroesophageal reflux disease. J Gastrointest Surg. 2010;14:1895-1901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Repici A, Fumagalli U, Malesci A, Barbera R, Gambaro C, Rosati R. Endoluminal fundoplication (ELF) for GERD using EsophyX: a 12-month follow-up in a single-center experience. J Gastrointest Surg. 2010;14:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Witteman BP, Strijkers R, de Vries E, Toemen L, Conchillo JM, Hameeteman W, Dagnelie PC, Koek GH, Bouvy ND. Transoral incisionless fundoplication for treatment of gastroesophageal reflux disease in clinical practice. Surg Endosc. 2012;26:3307-3315. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 19. | Furnée EJ, Broeders JA, Draaisma WA, Schwartz MP, Hazebroek EJ, Smout AJ, van Rijn PJ, Broeders IA. Laparoscopic Nissen fundoplication after failed EsophyX fundoplication. Br J Surg. 2010;97:1051-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Schindlbeck NE, Klauser AG, Berghammer G, Londong W, Müller-Lissner SA. Three year follow up of patients with gastrooesophageal reflux disease. Gut. 1992;33:1016-1019. [PubMed] |
| 21. | Vigneri S, Termini R, Leandro G, Badalamenti S, Pantalena M, Savarino V, Di Mario F, Battaglia G, Mela GS, Pilotto A. A comparison of five maintenance therapies for reflux esophagitis. N Engl J Med. 1995;333:1106-1110. [PubMed] |
| 22. | Fass R, Sifrim D. Management of heartburn not responding to proton pump inhibitors. Gut. 2009;58:295-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 240] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 23. | Kellokumpu I, Voutilainen M, Haglund C, Färkkilä M, Roberts PJ, Kautiainen H. Quality of life following laparoscopic Nissen fundoplication: assessing short-term and long-term outcomes. World J Gastroenterol. 2013;19:3810-3818. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 53] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (5)] |
| 24. | Wendling MR, Melvin WS, Perry KA. Impact of transoral incisionless fundoplication (TIF) on subjective and objective GERD indices: a systematic review of the published literature. Surg Endosc. 2013;27:3754-3761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Witteman BP, Kessing BF, Snijders G, Koek GH, Conchillo JM, Bouvy ND. Revisional laparoscopic antireflux surgery after unsuccessful endoscopic fundoplication. Surg Endosc. 2013;27:2231-2236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Perry KA, Linn JG, Eakin JL, Onders RP, Velanovich V, Melvin WS. Transoral incisionless fundoplication does not significantly increase morbidity of subsequent laparoscopic Nissen fundoplication. J Laparoendosc Adv Surg Tech A. 2013;23:456-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |