Published online Dec 7, 2014. doi: 10.3748/wjg.v20.i45.16984
Revised: June 25, 2014
Accepted: August 13, 2014
Published online: December 7, 2014
Processing time: 228 Days and 19 Hours
The incidence of colorectal cancer has been increasing in the developed world including South Korea and China. Colonoscopy allows for greater diagnostic specificity and sensitivity compared with other types of examinations, such as the stool occult blood test, barium enema, and computed tomography colonography. Therefore, in recent years, the demand for colonoscopies has grown rapidly. New beginners including primary care physicians may help meet the increasing demand by performing colonoscopies. However, it is a challenge to learn the procedure due to the long learning-curve and the high rate of complications, such as perforation and bleeding, as compared to gastroscopy. Thus, considerable training and experience are required for optimal performance of colonoscopies. In order to perform a complete colonoscopic examination, there were a few important things to learn and remember, such as the position of examinee (e.g., left and right decubitus, supine, and prone) and examiner (two-man method vs one-man standing method vs one-man sitting method), basic skills (e.g., tip deflection , push forward and pull back, torque, air suction and insufflation), advanced skills (e.g., jiggling and shaking, right and left turn shortening, hooking, and slide-by technique), assisting skills (e.g., position change of examinee, abdominal compression, breathing-holding, and liquid-infusion technique), and intubation techniques along the lower gastrointestinal tract. In this article, we attempt to describe the methods of insertion and advancement of the colonoscope to the new beginners including primary care physician. We believe that this article may be helpful to the new beginners who wish to learn the procedure.
Core tip: The demand for colonoscopy has been increasing every year. However, it is a challenge to learn the procedure due to its long learning curve and high rate of complications. Therefore, care must be taken in teaching, learning and practicing the procedure. Also, there are a few important things to learn and remember, such as the positions of the examinee and the examiner, basic skills, advanced skills, assisting skills, and intubation techniques along the lower gastrointestinal tract.
- Citation: Lee SH, Park YK, Lee DJ, Kim KM. Colonoscopy procedural skills and training for new beginners. World J Gastroenterol 2014; 20(45): 16984-16995
- URL: https://www.wjgnet.com/1007-9327/full/v20/i45/16984.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i45.16984
Colorectal cancer (CRC) is one of the most common malignancies in the developed world, including North America and Europe, and the incidence of CRC appears to be increasing in East Asian countries, including China and South Korea[1-3]. Since its first introduction in 1969, the colonoscopy has been accepted as a powerful screening tool for the early detection of CRC. Also, it plays an important role in the prevention of CRC through the diagnosis and removal of adenomatous polyps (premalignant lesions of CRC)[4-6]. As a result, the demand for screening colonoscopies is rapidly growing worldwide. However, the number of qualified endoscopists worldwide is not sufficient to meet the growing demand. One way of addressing this shortage of endoscopists may be to train new beginners to competency in colonoscopy. Actually, in clinical practice, trained beginners including primary care physicians can perform colonoscopy safely and effectively. Hence, they can contribute to meeting the growing demand for the procedure.
Trainees must acquire both technical and cognitive skills associated with the procedure. The technical skill subset, including mastery over manipulating the scope, is more essential than learning the cognitive skills, although beginners always attain their cognitive abilities first. Thus, we will focus on the technical skills of colonoscopic examinations for the new beginners including primary care physicians.
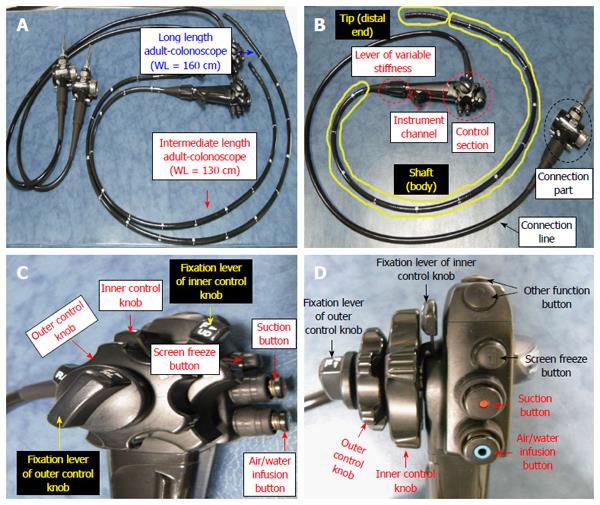
Just as learning the basics of vehicles can help one learn to drive, understanding the basics of the colonoscopy equipment can be helpful to an individual learning the procedure. Colonoscopy equipment consists of two major sections: the main body, including the CPU (central processing unit), and the colonoscope. The colonoscope is the main tool of the basic colonoscopic examination.
Unlike gastroscopes, colonoscopes have greater lengths and diameters (Table 1, Figure 1A). This is especially true in long adult-colonoscopes, which are used in cases where cecal intubation is difficult due to extensive stricture and/or curvature of the colon[7,8].
| Characteristic | Adult-gastroscope | Adult-colonoscope | |
| Intermediate length-type | Long length-type | ||
| Total length1 | 1350 mm (1.35 m) | 1650 mm (1.65 m) | 2000 mm (2 m) |
| Working length2 | 1030 mm (1.03 m) | 1330 mm (1.33 m) | 1680 mm (1.68 m) |
| Diameter | 9.2 mm | 12.9 mm | |
| Diameter of instrument channel | 2.8 mm | 3.7 mm | |
| Angulation range3 | Up 210°, Down 90°, Right 100°, Left 100° | Up 180°, Down 180°, Right 160°, Left 160° | |
The colonoscope (Figure 1B) consists of the control section (Figure 1C and D), an instrument channel (forcep, snare, injector, and clip device), a shaft (the portion of the instrument inserted into the patient), the tip (the distal end of shaft; controlled from the control section), a connection section, and the line. Some models also have a lever for variable stiffness.
As is the case with esophagogastroduodenoscopy (EGD), the left lateral decubitus position is the basic posture of the examinee during the colonoscopy (Figure 2A). Also, just as a correct posture is required for an athlete to attain better performance and to prevent injuries, it is important for the examiner (endoscopist) to adopt the appropriate posture while performing the colonoscopy. There are three different postures available to perform the colonoscopic examination: (1) two-man method; (2) one-man standing method; and (3) one-man sitting method (Table 2, Figure 2B-D)[9].
| Two-man method | One-man standing method | One-man sitting method | |
| The proportion of colonoscopists using methods | A few | Most | A few (More than two-man method) |
| Minimal number of assistants | Two people | One person | One person |
| Space | Relatively large | The smallest | Small |
| Colonoscope | Only long length adult-colonoscope | Both long length- and intermediate length- adult colonoscope (Intermediate-scope preferred) | Both long length- and intermediate length- adult colonoscope (Intermediate-scope preferred) |
| The role of colonoscopist | Only manipulation of the control section of colonoscope; most manipulations of colonoscope such as advance (push-forward) and withdrawal (pull-back) by assistant | All manipulations of colonoscope including advance, withdrawal, and handling of the control section | All manipulations of colonoscope including advance, withdrawal, and handling of the control section |
| The fatigue of colonoscopist | Low | High | Lowest |
| Location of examinee's anus | Below examiner's head | Below examiner's head | Examiner's head level (colonoscopist may be required to wear a mask for hygiene reasons) |
| The risk of perforation | Relatively high (colonoscopist cannot feel the colonoscope insertion) | Relatively low (colonoscopist can feel the colonoscope insertion) | Relatively low (colonoscopist can feel the colonoscope insertion) |
Tip deflection: Vertical (up/down) and lateral (left/right) tip deflection is a basic technique for colonoscopies, performed by using a control knob (Figure 1C and D)[10]. There are two control knobs in the control section of colonoscope. The larger outer control knob is used for vertical movement of the tip (Figure 3A and B) and the smaller inner knob is used for lateral movement of the tip (Figure 3C and D).
Push forward and pull back:“Push forward (PF)” is the action of pushing the colonoscope tip forward through the anus, whereas “pull back (PB)” is the action of pulling it backward (Figure 3E)[10]. PF is essential for advancing the colonoscope. However, paradoxically, PB is more important than PF for advancing the colonoscope. PB is helpful to resolve colonic loops and to keep the colonoscope straight and shortened.
Torque: Torque is applied by twisting the body of the colonoscope to the right (clockwise) or left (counter-clockwise) using the hand holding it. Applying torque can prevent loop formation. Applying torque when the tip is deflected upward also has the effect of turning the colonoscope to the left or right without using the left/right control knob.
Air insufflation and suction: Air infusion (Figure 3F and G) and suction (Figure 3H and I) are performed by using the air/water infusion valve and the suction valve buttons. The colon is an easily distensible mobile elastic tube which becomes long and tortuous when overinflated, enhancing the difficulty of the procedure. Hence, endoscopists must minimize air insufflation and suction frequently during the intubation period of the colonoscopy.
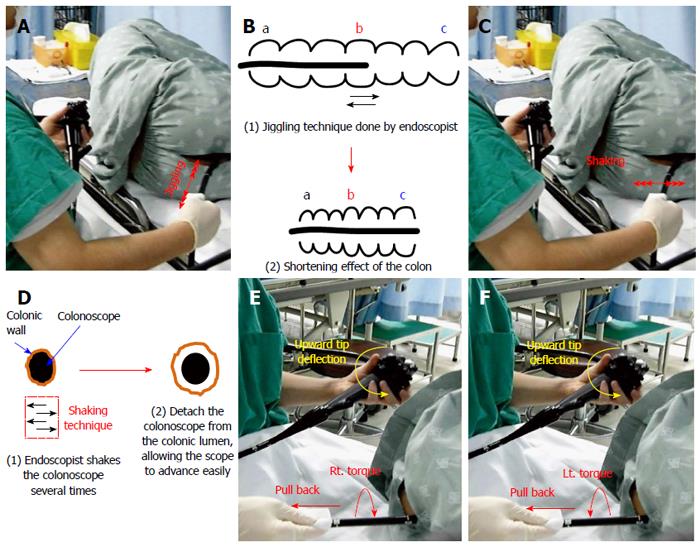
Jiggling and shaking: The jiggling technique involves moving the scope in and out in 5- to 10-cm increments (Figure 4A)[11]. A view of the lumen should be maintained while the maneuver is performed. The technique is helpful to shorten and straighten the colon. This technique is also helpful to proximally advance within the colon (Figure 4B). The shaking technique involves moving the scope left and right, which prevents the colonic lumen from adhering to the colonoscope (Figure 4C and D).
Right turn/left turn shortening: Right turn shortening (RTS) and left turn shortening (LTS) are complex and difficult techniques used in the colonoscopy procedure[11]. Turn shortening is a combined technique performed by the endoscopist; RTS requires a right torque of the scope and PB (Figure 4E and F), while LTS combines a left torque of the scope and PB. These techniques can resolve a loop formation of the colon and enhance proximal advancement of the scope by shortening the colon. RTS is more common than LTS during the procedure.
Hooking technique: The hooking technique involves a hook and pull-back motion of the scope, which is helpful in straightening the tortuous colonic segment. In this technique, the tip of the colonoscope is deflected 30 to 90 degrees behind a mucosal fold, and then the scope is withdrawn approximately 5 to 10 cm. This action pulls the segment of tortuous colon downward.
Slide-by technique: This technique is used to advance the colonoscope by repetitively pushing the tip slightly forward in the anticipated direction of the colon lumen, although the next direction of the colon is not visualized due to acute angulation and/or many folds of the colon. Also, it is usually used when there is a risk of a red-out sign. In most cases, this technique causes pain in the examinee. Thus, this technique should not be attempted by a beginner but only performed by an experienced endoscopist to avoid the high risk of iatrogenic perforation. If mucosal blanching occurs, it may be indicative of excessive scope force on the mucosa, and could result in perforation. In that situation, the colonoscope must be withdrawn.
The techniques described above are commonly used by the colonoscopists. The techniques described below are performed by the assistant or the examinee[12].
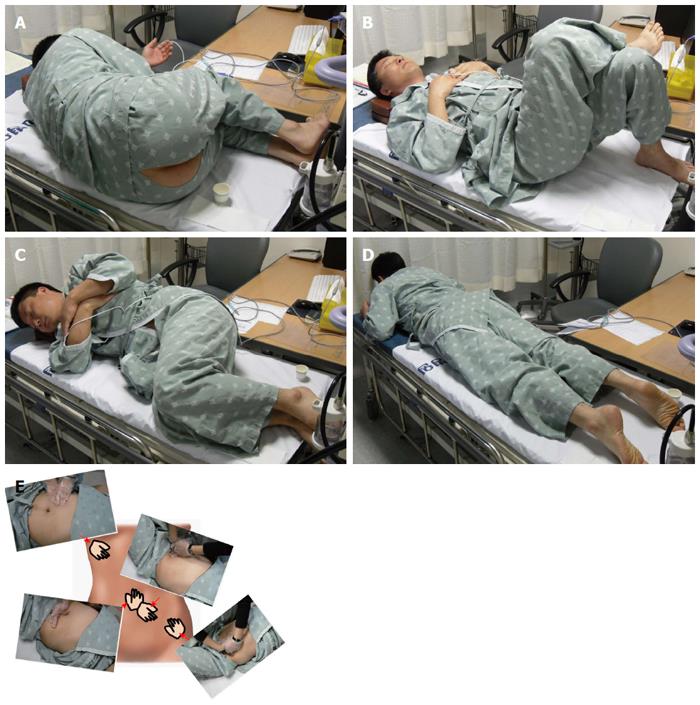
Position change of examinee: Colonoscopy is usually performed with the examinee in the left lateral decubitus position (Figure 5A) and ends in that position[13]. If difficulty arises, the position of the examinee can be changed to supine (Figure 5B), the right lateral decubitus position (Figure 5C), or rarely, the prone position (Figure 5D)[13-15]. The supine position is usually helpful during progression within the rectosigmoid junction (RSJ), sigmoid colon (SC), sigmoidodescending junction (SDJ), descending junction (DC), splenic flexure (SF), and transverse colon (TC), while supine or right lateral decubitus positions are usually indicated during the progression within the hepatic flexure (HF) or ascending colon (AC).
Abdominal compression: Abdominal compression is performed by an assistant, at the request of the endoscopist, by pressing the desired part of the abdomen using one or both hands to help advance the colonoscope (Figure 5E). Although compression may be applied to any part of the abdomen, the most common applied sites are the SC and the SDJ.
Others: Other useful colonoscopic techniques include liquid infusion and the breath-holding techniques. The liquid infusion technique is performed by injecting water or saline solution with a liquid injector, to open up an adhered colon lumen and lubricate its inner surface. The breath-holding technique occurs when the patient holds his or her breath in order to lower the diaphragm, de-angulating the SF and/or HF.
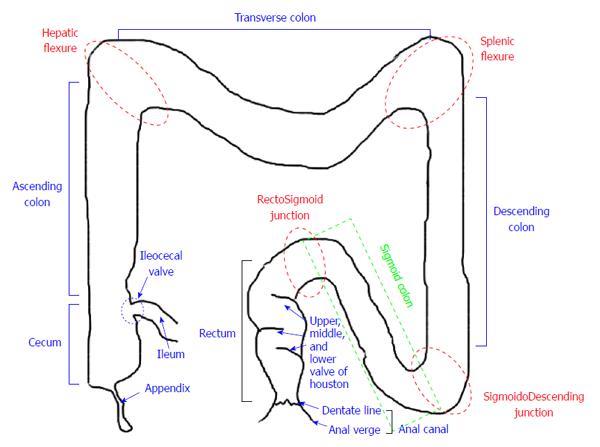
The large intestine (colon) is a long tubular organ that begins at the cecum (CC) and ends at the rectum (Figure 6). Therefore, the cecum is the proximal part of the colon and the rectum is the distal part. However, since the colonoscope is inserted from the anus and passes through the rectum first, the procedure will be explained in that order.
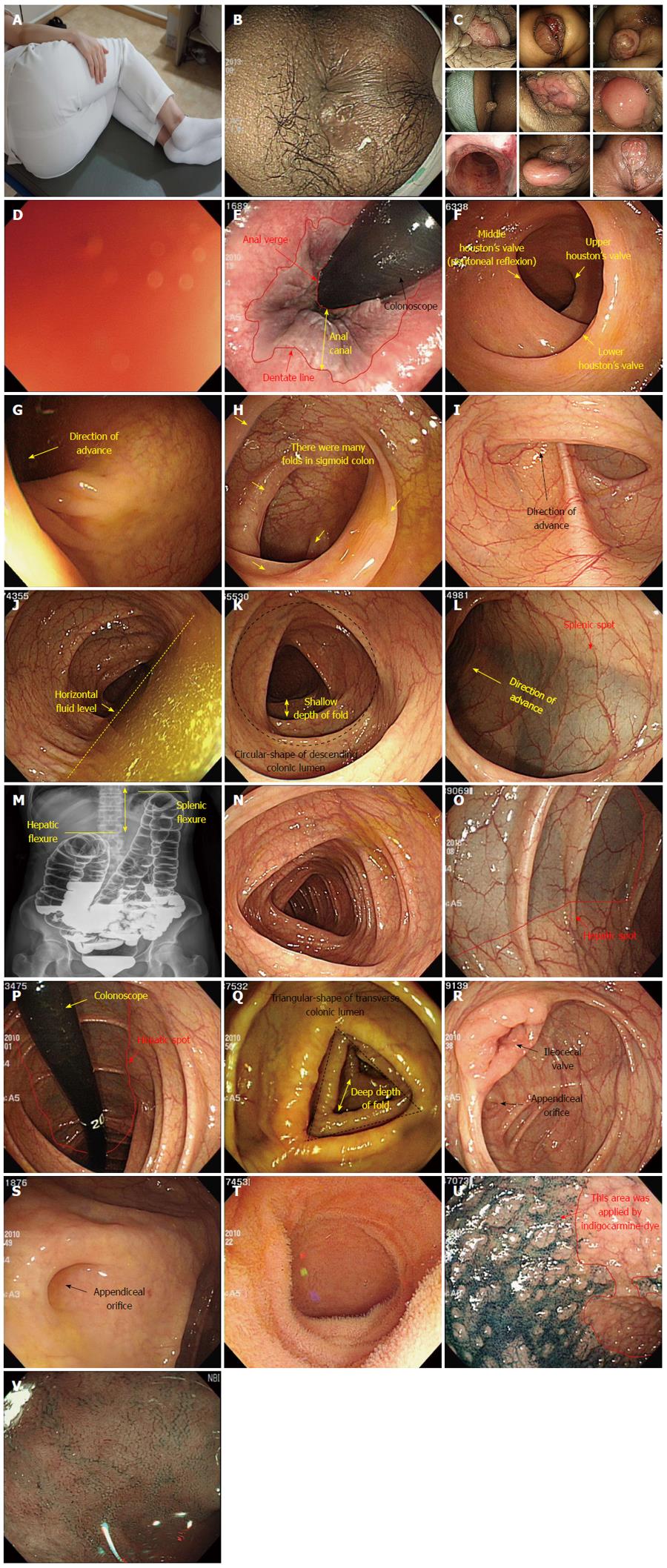
The patient is initially placed on the examination table in the left lateral decubitus position with knees bent and pulled up (Figure 7A). The examination begins with an inspection of the perianal region (Figure 7B). A simple inspection can detect various perianal lesions such as skin tags, scarring, anal fistulae and fissures, hemorrhoids, and prolapse (Figure 7C). Also, the digital rectal examination with topical anesthetic jelly (usually lidocaine jelly) should be performed to prelubricate the anal canal and relax the sphincters.
The anal canal is very short segment (about 2-3 cm) from the anal verge to the dentate line. When the colonoscope is intubated, a red-out sign usually occurs (Figure 7D). Thus, air inflation of the anus using the air/water infusion valve button is required. After aeration of the anus, the colonoscope can be inserted without red-out. The anal canal cannot be completely examined while intubating the colonoscope due to its short length and the anal sphincter. Once the scope has been withdrawn to the level of the distal rectum, it should be retroflexed. The retroflexion (the so-called U-turn maneuver) provides an opportunity to view the distal area of the rectum, which is difficult to observe during insertion (Figure 7E).
The rectum is the approximately 15 cm long colonic segment from the dentate line to the RSJ. It is easy to advance the colonoscope through this region because the rectum is attached to the retroperitoneal wall and has almost no mobility. Houston’s valves are characteristically observed in the rectum (Figure 7F). They usually exist in a left-right-left alignment. The colonoscope should progress easily through this segment using PF with left and right turns.
Generally, this region is the first challenging area in the colonoscope intubation. The success in passing through RSJ often determines the success of the colonoscopic examination itself. In most cases, the lumen opens to the left axis (Figure 7G) and the junction between the rectum and the SC often appears as an acute bend in the lumen. Advancing the colonoscope with only the pushing action may cause a loop to form, making it difficult to progress further. Therefore, it is generally helpful to advance the colonoscope while applying a left torque with mild pushing.
In general, the SC and SDJ are the most difficult segments to scope during insertion, as well as the most common sites of iatrogenic perforation, especially inexperienced and unskilled endoscopists. Thus, more attention must be paid when progressing through these areas[16]. The SC is situated intraperitoneally and is highly variable in length (ranging from 20 to 90 cm). Also, the SC has many folds making various curves (Figure 7H), and therefore, when the scope enters the SC, redundant folds obliterate the lumen. Adequate air insufflation may be necessary to visualize the lumen. SC looping unavoidable as the colonoscope pushes inward, but the endoscopist can minimize the loop formation using various techniques (jiggling, shaking, and RTS) with a continuous right torque. The basic technique in this region is to use left and right turns while performing half-suction, thus avoiding adhesion of the lumen. Also, manual abdominal compression by the assistant and changing the examinee’s position may be helpful. If progress has been made up to these segments with minimal loop formation during intubation, the inserted length of the colonoscope should be approximately 40 cm, depending on the patient. Sometimes, extensive turning of the scope tip, torquing, accordionization, and dithering techniques may be needed to negotiate the marked angle of SC. The endoscopist should avoid excessive aeration of SC, which occurs in cases of acute angulation of the SDJ (Figure 7I), making it difficult to advance the colonoscope. Once these areas are passed without or with minimal loop formation, it should not be difficult to progress up to the CC.
After the passing through the SDJ, the DC appears as a long tube, ringed with concentric haustra (Figure 7K). It usually has a horizontal fluid level, located to the right of the DC lumen (Figure 7J). In most cases, the DC is normally traversed in a few seconds with a short “straight” advance and PF usually suffices to pass through this area. The DC, which is attached to the retroperitoneal wall, has low mobility, as does the AC.
The SF can be recognized by the splenic spot seen through the colonic lumen (Figure 7L), although it is usually not as pronounced as in the HF. The SF is the highest section of the colon, located just below the diaphragm (Figure 7M). It is recommended to advance the colonoscope through this segment with the up/down control knob set to a neutral state to avoid the walking-stick phenomenon. If progression is difficult, the examiner may change the examinee’s position and/or have an assistant provide abdominal compression. Additionally, the breath-holding technique in the non-sedated examinee may also be helpful because it widens the angle of the SF by lowering the diaphragm.
The lumen of the TC is usually more triangular than that of the DC (Figure 7N) and it has much mobility, similar to the SC. Air suction is helpful in this area since the colonoscope advances relative to the air suction. If progression is difficult, the assistant should be instructed to perform abdominal compression on the umbilical area. This will prevent loop formation by inhibiting the descent of the TC to the pelvis.
In most cases, the end of the TC is easy to recognize because the hepatic spot can be seen through the mucosa (Figure 7O and P). The lumen of the AC of the next section is usually located on the right side. In most cases, insertion through this section can easily be performed by applying a right turn in the anticipated direction of the lumen together and air suction. If progression becomes difficult, shifting the examinee to a supine position may be helpful.
The AC is more triangular in shape and has thicker folds than the other colonic segments (Figure 7Q). Since it is attached to the retroperitoneal wall and has low mobility, advancing the colonoscope to the CC, the end point of the colon, can be achieved easily by simple straight pushing.
The CC spans the ileocecal valve (ICV) to the cecal base. It is important to check for the ICV (Figure 7R) and the appendix orifice (Figure 7S) in order to confirm the scope’s location in the CC. If progression becomes difficult, air suction in the lumen can usually resolve the problem. Otherwise, the examiner can alter the patient’s position, or instruct the assistant to perform abdominal compression.
The ICV can usually be seen on the left part of the colonoscopy screen when the colonoscope reaches the CC. It is usually closed, but the scope can pass through by deflecting its tip while approaching the ICV. To open the entrance, the examiner should repeatedly approach the ICV while using air suction[17]. Progression will cause a red-out sign followed by the visualization of the terminal ileum (Ti) once the ICV opens. The Ti is the end point of the small intestine and its characteristic villi can be observed by various methods such as water-filling (Figure 7R), indigocarmine-dye (Figure 7S), and narrow-band imaging mode (Figure 7T).
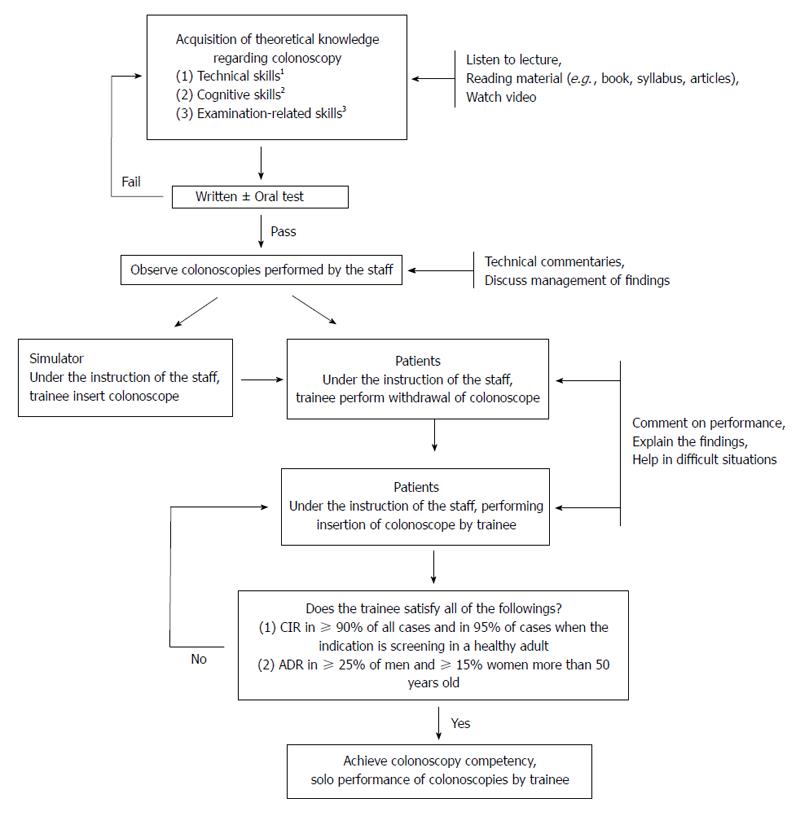
Colonoscopy requires practical skills obtained by extensive training[18]. Expertise in the procedure can be judged by technical aspects, such as ease and completeness of intubation, precision of observation, and the minimal degree of patient discomfort and pain during the examination[19]. On the basis of many studies in a variety of societies internationally, competency in the procedure is achieved by performing at least 30-200 colonoscopy procedures[19-22]. However, trainees may differ considerably in the rate at which they acquire the necessary psychomotor skills, although recent evidence suggests that most will arrive at procedural competency after performing 200 procedures[22]. In South Korea, the new beginners including primary care physicians can benefit from a comprehensive education program on colonoscopy (Figure 8).
South Korea is facing an increased prevalence of colorectal diseases including CRC, colorectal polyps, and inflammatory bowel diseases (IBD) due to changing behaviors, such as westernized dietary habits and lifestyle[23]. Under such circumstances, the demand of colonoscopy has been increasing annually. Currently, the demand cannot be met by specialists alone. Also, the issues of the efficiency and the productivity of endoscopists are increasingly being discussed in developed countries because of a rapidly rising demand for colonoscopic examination[24]. This demand often perceived as potentially overwhelming and is usually framed in the suggestion that there might not be enough endoscopists to meet this demand. An obvious solution may be to train more new beginners including primary care physicians. However, the colonoscopy procedure takes a long time to learn and can cause complications such as perforation, hemorrhage, and pain in examinees[22,25]. Therefore, care must be taken in teaching, learning, and practicing the procedure. We hope to improve the performance and training of colonoscopy for the new beginners by our manuscript.
P- Reviewer: Anadol Z, Nakase H, Sewitch MJ, Sinagra E S- Editor: Ma YJ L- Editor: A E- Editor: Wang CH
| 1. | Lee SH, Lee DJ. Comparison on colonoscopic parameters according to length of adult-colonoscope. Chin Med J (Engl). 2014;127:85-91. [PubMed] |
| 2. | Jang JY, Chun HJ. Bowel preparations as quality indicators for colonoscopy. World J Gastroenterol. 2014;20:2746-2750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (2)] |
| 3. | O’Farrell CM, Green BB, Reid RJ, Bowen D, Baldwin LM. Physician-patient colorectal cancer screening discussions by physicians’ screening rates. J Am Board Fam Med. 2012;25:771-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Dik VK, Moons LM, Siersema PD. Endoscopic innovations to increase the adenoma detection rate during colonoscopy. World J Gastroenterol. 2014;20:2200-2211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 57] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Zapka J, Klabunde CN, Taplin S, Yuan G, Ransohoff D, Kobrin S. Screening colonoscopy in the US: attitudes and practices of primary care physicians. J Gen Intern Med. 2012;27:1150-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Lee SH, Huh GY, Cheong YS. A case of endoscopic resection of a colonic semipedunculated leiomyoma. J Korean Soc Coloproctol. 2011;27:215-219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Varadarajulu S, Banerjee S, Barth BA, Desilets DJ, Kaul V, Kethu SR, Pedrosa MC, Pfau PR, Tokar JL, Wang A. GI endoscopes. Gastrointest Endosc. 2011;74:1-6.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Kim KM, Lee SH, Lee DJ, Kim KN, Seo SW, Lee HS, Lee DR. A randomized controlled trial of comparison on time and rate of cecal and termianl Ileal intubation according to adult-colonoscope length: intermediate versus long. J Korean Med Sci. 2014;29:98-105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Horiuchi A, Nakayama Y. Colonoscopy in the sitting position: lessons learned from self-colonoscopy by using a small-caliber, variable-stiffness colonoscope. Gastrointest Endosc. 2006;63:119-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Jung Y, Lee SH. How do I overcome difficulties in insertion? Clin Endosc. 2012;45:278-281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Church JM. Ancillary colonoscope insertion techniques. An evaluation. Surg Endosc. 1993;7:191-193. [PubMed] |
| 13. | Williams C. Position changes during colonoscopy: opening a can of worms? Gastrointest Endosc. 2007;65:270-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (1)] |
| 14. | Uddin FS, Iqbal R, Harford WV, Dunbar KB, Cryer BL, Spechler SJ, Feagins LA. Prone positioning of obese patients for colonoscopy results in shortened cecal intubation times: a randomized trial. Dig Dis Sci. 2013;58:782-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | De Silva AP, Kumarasena RS, Perera Keragala SD, Kalubowila U, Niriella M, Dassanayake AS, Pathmeswaran A, de Silva HJ. The prone 12 o’clock position reduces ileal intubation time during colonoscopy compared to the left lateral 6 o’clock (standard) position. BMC Gastroenterol. 2011;11:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Long HF. Sensitive sigmoidoscopy: a straight sigmoid technique. J Am Board Fam Pract. 1989;2:103-105. [PubMed] |
| 17. | Jeong SH, Lee KJ, Kim YB, Kwon HC, Sin SJ, Chung JY. Diagnostic value of terminal ileum intubation during colonoscopy. J Gastroenterol Hepatol. 2008;23:51-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 56] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Koch AD, Haringsma J, Schoon EJ, de Man RA, Kuipers EJ. Competence measurement during colonoscopy training: the use of self-assessment of performance measures. Am J Gastroenterol. 2012;107:971-975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Wilkins T, Jester D, Kenrick J, Dahl J. The current state of colonoscopy training in family medicine residency programs. Fam Med. 2004;36:407-411. [PubMed] |
| 20. | Rex DK. Quality in colonoscopy: cecal intubation first, then what? Am J Gastroenterol. 2006;101:732-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE, Hoffman B, Jacobson BC, Mergener K, Petersen BT. Quality indicators for colonoscopy. Am J Gastroenterol. 2006;101:873-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 532] [Cited by in RCA: 561] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 22. | Chung JI, Kim N, Um MS, Kang KP, Lee D, Na JC, Lee ES, Chung YM, Won JY, Lee KH. Learning curves for colonoscopy: a prospective evaluation of gastroenterology fellows at a single center. Gut Liver. 2010;4:31-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 23. | Goh LY, Leow AH, Goh KL. Observations on the epidemiology of gastrointestinal and liver cancers in the Asia-Pacific region. J Dig Dis. 2014;15:463-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (1)] |
| 24. | Rex DK, Lieberman DA. Feasibility of colonoscopy screening: discussion of issues and recommendations regarding implementation. Gastrointest Endosc. 2001;54:662-667. [PubMed] |
| 25. | Lee SH, Cheong YS. Successful endoscopic repair of an iatrogenic colonic perforation during diagnostic colonoscopy. J Am Board Fam Med. 2012;25:383-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |