Published online Nov 21, 2014. doi: 10.3748/wjg.v20.i43.16282
Revised: July 4, 2014
Accepted: July 24, 2014
Published online: November 21, 2014
Processing time: 163 Days and 24 Hours
AIM: To develop a technique of sleeve-wrapping the pedicled omentum around the esophagogastric anastomosis for preventing and localizing leakage.
METHODS: This study includes data from 86 patients who were diagnosed with esophageal cancer and underwent the technique of sleeve-wrapping the pedicled omentum around esophagogastric anastomosis after esophagectomy between November 2011 and July 2013. The early complications that occurred during follow-up were analyzed.
RESULTS: Postoperative complications included pulmonary complications (13/86; 15.1%) and abdominal or thoracic wound infection (3/86; 3.5%). Complications that occurred during follow-up included one case of anastomosis leakage (limited by omentum; 1.2%) and five case of anastomosis stricture (5.8%). No deaths occurred. All complications were resolved through traditional treatment. No additional surgery was needed.
CONCLUSION: Sleeve-wrapping of the pedicled omentum around esophagogastric anastomosis after esophagectomy is safe and effective for preventing and localizing anastomosis leakage without increasing anastomosis stricture.
Core tip: This study describes sleeve-wrapping of the pedicled omentum around esophagogastric anastomosis after esophagectomy to prevent and localize anastomosis leakage for the treatment of esophageal carcinoma. A total of 86 patients with esophageal carcinoma were operated upon with the new anastomosis technique at our institute, and only one patient developed anastomotic leakage, which was limited by the omentum, and successfully cured by conservative treatment. A better understanding of this may provide a good alternative method for anastomosis after esophagogastrectomy of esophageal cancer.
- Citation: Liu QX, Deng XF, Hou B, Min JX, Dai JG. Preventing and localizing esophagogastric anastomosis leakage by sleeve-wrapping of the pedicled omentum. World J Gastroenterol 2014; 20(43): 16282-16286
- URL: https://www.wjgnet.com/1007-9327/full/v20/i43/16282.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i43.16282
Esophagectomy for early- and middle-stage esophageal tumors remains the standard for curative or palliative therapy. For patients with node-negative esophageal carcinoma who have had resection, it is possible to achieve five-year survival rates of 43%-54%[1,2]. Esophagogastric anastomotic leakage is considered a life-threatening postoperative complication, especially when it occurs in the chest. Postoperative anastomotic leakage rates of 2%-20% have recently been reported for esophagectomy with cervical anastomosis. Cervical anastomoses have a higher leakage rate than intrathoracic anastomoses, but leaks from the latter are usually more life threatening[3-5].
Anatomical factors implicated in anastomotic leakage include inadequate blood supply, lack of serosa, and fragile longitudinal muscle layers, which make it difficult to attain watertight suturing for the esophagogastric anastomoses. Anastomosis for esophageal reconstruction is of central importance in the practice of esophageal surgery. Most anastomoses can be successful when the site is tension free and nourished with an excellent blood supply. Various technical innovations have been reported for prevention of anastomotic leakage, including wrapping the stomach around the anastomosis, stapling devices, tunnel esophagogastrostomy, triangulating stapling technique, and wrapping an omental graft around the anastomosis[6-8]. However, the outcomes are still disappointing or controversial and no standardized treatment strategy has been settled.
Here, we introduce our initial experience with a modified esophagogastric anastomosis technique (sleeve-wrapping of the pedicled omentum around esophagogastric anastomosis) after esophagectomy for preventing and localizing anastomosis leakage.
This study protocol was approved by the Ethics Committee of the Third Military Medical University, Chongqing, China and all the patients gave written informed consent. Between November 2011 and July 2013, a total of 86 patients with esophageal carcinoma were operated upon with the new anastomosis technique at our institute. The distance from the incisors to the tumors ranged from 21 to 37 cm; and the longitudinal dimension ranged from 1 to 5 cm. The average length of hospital stay was 17.5 d (range: 10-29 d). The patient characteristics are shown in Table 1.
| Characteristics | Value |
| Male/female, n | 21/66 |
| Age, yr | 63 ± 8 |
| Site of tumor, n | |
| Upper thoracic | 17 |
| Middle thoracic | 39 |
| Lower thoracic | 31 |
| Tumor size, cm | 3 ± 1.5 |
| Stage of tumor, n | |
| I | 12 |
| IIa | 21 |
| IIb | 43 |
| III | 11 |
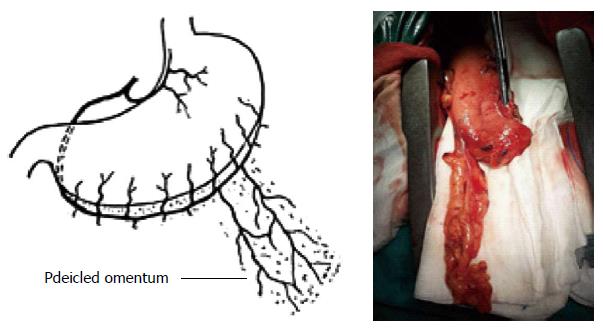
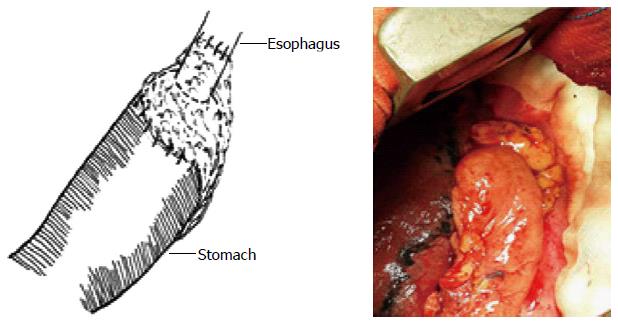
The patients were placed in the left vertical supine position with the right chest wall turned towards the surgeon. The esophagus was circumferentially mobilized and the tumor was dissected at the appropriate level through a right thoracotomy, with proximal and distal margins > 5 cm. The operative procedure also included removal of the lymph nodes along the celiac axis, left gastric artery, and lesser curve of the stomach. The right gastroepiploic artery was carefully preserved and the omentum was freed from the transverse colon and divided at the edge adherent to the colon so that both arterial communications and sufficient length of omentum were fully preserved. We mobilized 10-15 cm of pedicled omentum, with ≥ 6 cm remaining attached to the mobilized stomach on the terminal gastroepiploic arcade, close to the prospective line of gastric resection (Figure 1). We inserted a gastric tube with a diameter of 3 cm, with resection of the lesser curvature through midline laparotomy. The stomach was pulled through the anterior mediastinum for end-to-side esophagogastric anastomoses for ease of construction and standardization of the procedure. The curved circular stapler (CDH Ethicon; Johnson & Johnson, New Brunswick, NJ, United States) was used for end-to-side esophagogastric anastomoses in which a double ring of staples was produced with inversion of the esophageal and stomach borders. After the esophagogastric anastomosis was completed, a long and intact pedicled omentum was loosely sleeve-wrapped around the esophagogastric suture line. Subsequently, several sutures of the omentum were placed in the position of the residual esophagus and stomach, to ensure an esophagogastric anastomosis without tension (Figure 2). A nasogastric tube was inserted into the duodenum, and a vacuumed drainage tube was placed before the incision was closed.
All patients were observed after discharge every month thereafter for one year. Barium swallow examination and endoscopy were performed in all of the patients at follow-up to detect anastomotic leakage and benign anastomotic stricture. Diagnosis of anastomotic stricture was confirmed by endoscopy, where a 10-mm-diameter flexible endoscope could not pass.
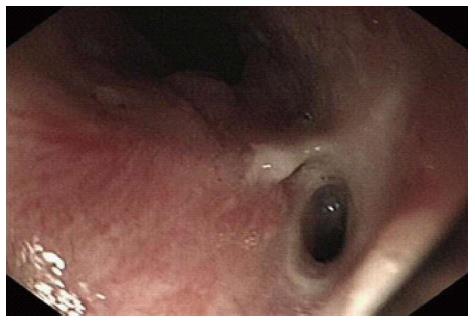
The average operative time of this procedure in 86 patients was 234 ± 28 min (mean ± standard deviation). Thirteen patients (13/86; 15.1%) developed postoperative pulmonary complications and they were all treated conservatively with bronchodilators, chest physiotherapy, and antibiotics. Abdominal or thoracic wound infection developed in three patients who responded to conservative management and were discharged within 24 ± 5 d postoperatively. Five patients developed anastomotic stricture. Only one patient developed anastomotic leakage, which was limited by the omentum, and successfully cured by conservative treatment. In this patient, we clearly noticed the function of the pedicled omentum in preventing and localizing anastomotic leakage. When the patient exhibited symptoms that were highly suspicious of anastomotic leakage, barium swallow examination and endoscopy were performed. In the X-ray film we did not observe anastomotic leakage (Figure 3). However, endoscopy of revealed anastomotic leakage, which seemed to be blocked by the omentum (Figure 4). This patient was managed conservatively with enteral nutrition and the anastomotic leakage closed spontaneously in 10 d.
Esophageal resection with gastric tube reconstruction is currently considered the standard treatment for curative or palliative care in patients with esophageal cancer[9]. It is reported that the five-year survival rates in patients with esophageal carcimona who have had resection with node-negative disease are between 43% and 54%[10]. However, esophagogastric anastomotic leakage between the remaining esophagus and gastric tube is still a life-threatening complication after esophageal resection, especially when the leakage occurs in the chest. The wound-healing process of esophageal anastomosis mimics that of wound healing in other tissues, which includes three phases: inflammation (0-4 d), proliferation (5-10 d), and remodeling (> 10 d)[11]. The use of a pedicled omentum may be effective in promoting these three phases. In our series, patients who were treated by the new technique had a quicker recovery and lower leakage rate compared with patients who underwent conventional anastomosis (1.2% vs 4%-10%[12-17]). In previous studies, the omentum or pedicled omentum was used simply to cover the esophagogastric anastomosis to avoid anastomosis leakage[18,19]. Compared with previous methods, the present technique has three advantages: (1) the right gastroepiploic artery was carefully preserved and the omentum was freed from the transverse colon and divided at the edge adherent to the colon, so that the length of the pedicled omentum and the arterial communications were preserved more fully; (2) two or three branches of the right gastroepiploic artery were preserved on the pedicled omental flap, which can provide an adequate blood supply; and (3) after wrapping the pedicled omental flap around the esophagogastric anastomosis, several sutures were placed to maintain the position of the omentum between the stomach and esophagus to ensure an anastomosis without tension.
Patients with stage I-III cancer are suitable candidates for our procedure. Careful preoperative workup for cervical, thoracic and mediastinal lymph node metastases is important. The length of the segment transected should be determined according to the length of the tumor, but the margin should be > 5 cm to reduce the chance of residual tumor. Both cervical and thoracic anastomoses are for this technique, though it is mainly used for thoracic anastomosis. Although leakage is more frequent with cervical anastomoses, these heal spontaneously with conservative management.
Based on the uncomplicated performance and shorter operating time of our procedure, it is applicable to all patients undergoing esophagectomy for esophageal cancer, and even to elderly patients. In our group, the procedure was performed safely in 15 patients > 75 years of age, of whom the eldest (85 years-old) had a smooth recovery. Anastomotic leakage occurred in one patient aged 65 years, but we were pleased to observe by barium swallow examination that the contrast agent did not leak from the esophageal lumen. Also, endoscopic examination showed that the omentum successfully blocked anastomotic leakage. This patient was managed conservatively and recovered in 10 d.
In conclusion, sleeve-wrapping the pedicled omentum around esophagogastric anastomoses is a feasible procedure for esophagectomy of esophageal cancer. The major advantages of the procedure are that it has a lower postoperative anastomotic leakage rate and shorter recovery time, and even when anastomotic leakage occurs, it can reduce the mortality and healing time.
The authors thank the study participants as well as all the researchers and staff for their contributions to this study.
Esophagectomy is still the standard treatment for patients with esophageal carcinoma. However, conventional esophagogastrostomy after esophagectomy is associated with a high frequency of esophagogastric anastomotic leakage that contributes to high morbidity and mortality. The purpose of this study was to develop a technique of sleeve-wrapping the pedicled omentum around esophagogastric anastomosis after esophagectomy for preventing and localizing anastomosis leakage.
Various modified technical innovations have been reported for preventing anastomotic leakage, including wrapping the stomach around the anastomosis, stapling devices, tunnel esophagogastrostomy, triangulating stapling technique, and wrapping the omental graft around the anastomosis. However, the outcomes are still disappointing or controversial and no standardized treatment strategy has been settled.
In previous studies, the omentum or pedicled omentum was used simply to cover the esophagogastric anastomosis to avoid anastomosis leakage. The present technique has three advantages over previous methods: (1) the right gastroepiploic artery was carefully preserved and the omentum was freed from the transverse colon and divided at the edge adherent to the colon, so that the length of the pedicled omentum and the arterial communications were preserved more fully; (2) two or three branches of the right gastroepiploic artery were preserved in the pedicled omental flap, which can provide an adequate blood supply; and (3) after wrapping of the pedicled omental flap around the esophagogastric anastomosis, several sutures were placed to maintain the position of the omentum between the stomach and esophagus to ensure an anastomosis without tension.
The study results suggest that sleeve-wrapping the pedicled omentum around an esophagogastric anastomosis is a feasible procedure for esophagectomy of esophageal cancer.
Pedicled omentum is the omentum that is freed from the transverse colon and divided at the edge adherent to the colon, with arterial communications.
This is a well-written and scientific description of esophageal anastomotic techniques from a single institution over a relatively short time frame. The methodology and results are clear and helpful. This paper describes an interesting method for anastomoses after esophagectomy for squamous cell carcinoma of the thoracic esophagus. The authors are to be congratulated on their excellent results.
P- Reviewer: Bintintan VV, Huang XB, Pal S S- Editor: Gou SX L- Editor: AmEditor E- Editor: Liu XM
| 1. | Tabira Y, Yasunaga M, Sakaguchi T, Yamaguchi Y, Okuma T, Kawasuji M. Outcome of histologically node-negative esophageal squamous cell carcinoma. World J Surg. 2002;26:1446-1451. [PubMed] |
| 2. | Tachibana M, Kinugasa S, Yoshimura H, Shibakita M, Tonomoto Y, Dhar DK, Nagasue N. Clinical outcomes of extended esophagectomy with three-field lymph node dissection for esophageal squamous cell carcinoma. Am J Surg. 2005;189:98-109. [PubMed] |
| 3. | Hulscher JB, Tijssen JG, Obertop H, van Lanschot JJ. Transthoracic versus transhiatal resection for carcinoma of the esophagus: a meta-analysis. Ann Thorac Surg. 2001;72:306-313. [PubMed] |
| 4. | Honda M, Kuriyama A, Noma H, Nunobe S, Furukawa TA. Hand-sewn versus mechanical esophagogastric anastomosis after esophagectomy: a systematic review and meta-analysis. Ann Surg. 2013;257:238-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 114] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 5. | Urschel JD. Esophagogastrostomy anastomotic leaks complicating esophagectomy: a review. Am J Surg. 1995;169:634-640. [PubMed] |
| 6. | Takemura M, Yoshida K, Fujiwara Y. Modified triangulating stapling technique for esophagogastrostomy after esophagectomy for esophageal cancer. Surg Endosc. 2013;27:1249-1253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Dai JG, Zhang ZY, Min JX, Huang XB, Wang JS. Wrapping of the omental pedicle flap around esophagogastric anastomosis after esophagectomy for esophageal cancer. Surgery. 2011;149:404-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Yuan Y, Wang KN, Chen LQ. Esophageal anastomosis. Dis Esophagus. 2014;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Zheng QF, Wang JJ, Ying MG, Liu SY. Omentoplasty in preventing anastomotic leakage of oesophagogastrostomy following radical oesophagectomy with three-field lymphadenectomy. Eur J Cardiothorac Surg. 2013;43:274-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Swanson SJ, Batirel HF, Bueno R, Jaklitsch MT, Lukanich JM, Allred E, Mentzer SJ, Sugarbaker DJ. Transthoracic esophagectomy with radical mediastinal and abdominal lymph node dissection and cervical esophagogastrostomy for esophageal carcinoma. Ann Thorac Surg. 2001;72:1918-1924; discussion 1924-1925. [PubMed] |
| 11. | Shomaf M. Histopathology of human intestinal anastomosis. East Mediterr Health J. 2003;9:413-421. [PubMed] |
| 12. | Craig SR, Walker WS, Cameron EW, Wightman AJ. A prospective randomized study comparing stapled with handsewn oesophagogastric anastomoses. J R Coll Surg Edinb. 1996;41:17-19. [PubMed] |
| 13. | Law S, Fok M, Chu KM, Wong J. Comparison of hand-sewn and stapled esophagogastric anastomosis after esophageal resection for cancer: a prospective randomized controlled trial. Ann Surg. 1997;226:169-173. [PubMed] |
| 14. | Laterza E, de’ Manzoni G, Veraldi GF, Guglielmi A, Tedesco P, Cordiano C. Manual compared with mechanical cervical oesophagogastric anastomosis: a randomised trial. Eur J Surg. 1999;165:1051-1054. [PubMed] |
| 15. | Okuyama M, Motoyama S, Suzuki H, Saito R, Maruyama K, Ogawa J. Hand-sewn cervical anastomosis versus stapled intrathoracic anastomosis after esophagectomy for middle or lower thoracic esophageal cancer: a prospective randomized controlled study. Surg Today. 2007;37:947-952. [PubMed] |
| 16. | Luechakiettisak P, Kasetsunthorn S. Comparison of hand-sewn and stapled in esophagogastric anastomosis after esophageal cancer resection: a prospective randomized study. J Med Assoc Thai. 2008;91:681-685. [PubMed] |
| 17. | Zhang YS, Gao BR, Wang HJ, Su YF, Yang YZ, Zhang JH, Wang C. Comparison of anastomotic leakage and stricture formation following layered and stapler oesophagogastric anastomosis for cancer: a prospective randomized controlled trial. J Int Med Res. 2010;38:227-233. [PubMed] |
| 18. | Ohwada S, Ogawa T, Kawate S, Koyama T, Yamada T, Yoshimura S, Sato Y, Tomizawa N, Ohya T, Morishita Y. Omentoplasty versus no omentoplasty for cervical esophagogastrostomy following radical esophagectomy. Hepatogastroenterology. 2002;49:181-184. [PubMed] |
| 19. | Thakur B, Zhang CS, Tan ZB. Omentoplasty versus no omentoplasty for esophagogastrostomy after surgery for cancer of cardia and esophagus. Indian J Cancer. 2004;41:167-169. [PubMed] |