Published online Oct 14, 2014. doi: 10.3748/wjg.v20.i38.13942
Revised: June 12, 2014
Accepted: July 11, 2014
Published online: October 14, 2014
Processing time: 188 Days and 0.1 Hours
AIM: To improve the diagnostic accuracy in patients with symptoms and signs of appendicitis, but without confirmative computed tomography (CT) findings.
METHODS: We retrospectively reviewed the database of 224 patients who had been operated on for the suspicion of appendicitis, but whose CT findings were negative or equivocal for appendicitis. The patient population was divided into two groups: a pathologically proven appendicitis group (n = 177) and a non-appendicitis group (n = 47). The CT images of these patients were re-evaluated according to the characteristic CT features as described in the literature. The re-evaluations and baseline characteristics of the two groups were compared.
RESULTS: The two groups showed significant differences with respect to appendiceal diameter, and the presence of periappendiceal fat stranding and intraluminal air in the appendix. A larger proportion of patients in the appendicitis group showed distended appendices larger than 6.0 mm (66.3% vs 37.0%; P < 0.001), periappendiceal fat stranding (34.1% vs 8.9%; P = 0.001), and the absence of intraluminal air (67.6% vs 48.9%; P = 0.024) compared to the non-appendicitis group. Furthermore, the presence of two or more of these factors increased the odds ratio to 6.8 times higher than baseline (95%CI: 3.013-15.454; P < 0.001).
CONCLUSION: Appendiceal diameter and wall thickening, fat stranding, and absence of intraluminal air can be used to increased diagnostic accuracy for appendicitis with equivocal CT findings.
Core tip: When equivocal computed tomography (CT) findings for appendicitis are encountered, the diagnostic accuracy can be enhanced by identifying several characteristic CT features: appendiceal diameter ≥ 6.0 mm, appendiceal wall thickening ≥ 2.0 mm, periappendiceal fat stranding, and the absence of intraluminal air. Therefore, radiologists, surgeons and physicians should apply these criteria when encountering patients with equivocal CT findings for appendicitis.
- Citation: Park G, Lee SC, Choi BJ, Kim SJ. Stratified computed tomography findings improve diagnostic accuracy for appendicitis. World J Gastroenterol 2014; 20(38): 13942-13949
- URL: https://www.wjgnet.com/1007-9327/full/v20/i38/13942.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i38.13942
Appendectomy is the most common acute abdominal surgical procedure worldwide. Appendicitis is mainly diagnosed based on meticulous history taking and physical examination. However, a substantial proportion of patients do not present with classic signs and symptoms[1-3], and there are many other conditions that resemble appendicitis. The introduction of computed tomography (CT) has dramatically improved the diagnostic accuracy for appendicitis, with a sensitivity of 90%-100% and a specificity of 91%-99%[4-6]. The CT criteria for appendicitis are mainly comprised of an appendiceal diameter greater than 6[7-9] or 7 mm[10-12] with thickening and enhancement of the circumferential wall, which may give a halo or target appearance. Although CT improves diagnostic accuracy, there can still be equivocal findings. Over time, several CT features have been described as indicators for a diagnosis of acute appendicitis. However, their significance and frequencies have not been extensively studied.
The purpose of this study was to systematically stratify CT findings in order to improve the diagnostic accuracy of appendicitis. To achieve this, we first reviewed the literature and searched CT findings relating to appendicitis. Thereafter, we examined the incidences of misdiagnosis within the database from our institution in which CT interpretation was negative or equivocal for appendicitis and re-evaluated them based on the criteria. Finally, we attempted to find the characteristic CT features supporting appendicitis by comparing the final pathologic results.
This study included a cohort of patients who underwent either appendectomy or an operation including appendectomy with the suspicion of acute appendicitis at the Department of Surgery, Daejeon St. Mary’s Hospital between January 2006 and November 2012. The patients were initially identified from a prospectively collected database that included correct diagnoses and treatments. Thereafter, the electronic medical records were thoroughly reviewed to collect additional information, such as patient’s histories, laboratory findings, and pathologic results. We obtained approval from the ethics committee of Daejeon St. Mary’s Hospital, the Catholic University of South Korea (IRB code: DC13RISI0025).
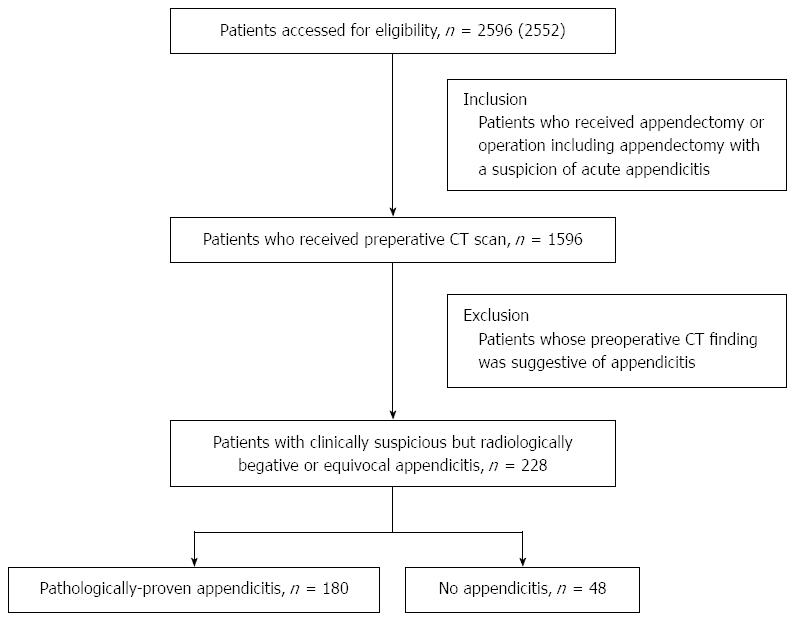
A total of 2596 patients were screened for eligibility (Figure 1). Of these, we selected 1596 patients with preoperative CT scans. Of these, we excluded 1372 patients whose CT interpretations coincided with the diagnosis. Accordingly, the final study group included 224 patients with negative or equivocal CT findings for appendicitis, and were thereafter operated on for suspected appendicitis. We then stratified these patients into a pathologically proven appendicitis group (PA group; n = 177) and a non-appendicitis group (NA group; n = 47).
Throughout the study period, only one radiologist (G Park) with more than ten years of experience in abdominal imaging interpreted the CT findings. The diagnostic criteria for appendicitis from CT scans included a distended appendix more than 7 mm in diameter and circumferential wall thickening and enhancement, often shown as a target or halo appearance.
During the day, CT images were obtained using a 64-slice multidetector CT (MDCT), and at night, they were obtained using a 6-slice MDCT scanner (Sensation 64 and Emotion 6, respectively; Siemens, Erlangen, Germany). Oral contrast medium was not administered, instead CT enhancement was accomplished using a 70 s delay after intravenous contrast media infusion, consisting of 110 mL of iopromide (Ultravist; Bayer Healthcare Pharmaceuticals, Berlin, Germany), iodixanol 270 contrast (Visipaque; GE Healthcare, Princeton, NJ), or iohexol (Iobrix 350; Taejoon Pharmaceutical, Kyungkido, South Korea) through an antecubital vein at 4 mL/s. CT parameters for the 6-slice MDCT scanner were collimation 2 mm, pitch 1.2, and rotation time 0.8 s, and the parameters for the 64-slice MDCT scanner were collimation 1.2 mm, pitch 1.4, and rotation time 0.5 s. Axial section data were reconstructed at a thickness of 3 mm with 3 mm increments.
We thoroughly reviewed the literature related to CT features of appendicitis and non-appendicitis[1-3,6,13,14]. The CT features related with appendicitis included: appendiceal diameter ≥ 6.0 mm, appendiceal wall thickening (≥ 2.0 mm), appendiceal wall enhancement, and presence of appendicolith, periappendiceal fat string, periappendiceal fluid collection, and periappendiceal lymphadenopathy. The CT features related with non-appendicitis included the presence of intraluminal air and/or coexisting inflammatory lesions. To avoid selection bias, the radiologist was not given information about the patient’s final diagnosis. The CT images were provided to the radiologist as a random sequence using a PACS (Maroview; Infinitt, Seoul, South Korea) in stack mode.
Appendiceal diameter was defined as the maximum diameter of the appendix observed in full magnification view, and appendiceal wall thickness was defined as a wall thickness of ≥ 2 mm in the full magnification view. Appendiceal wall enhancement was defined as attenuation of the appendiceal wall that was subjectively equal to or greater than that of the normal bowel wall[15]. Mesenteric lymphadenopathy was defined as at least one lymph node larger than 1.0 cm in the short axis diameter or as a cluster of at least four lymph nodes of any size in the right lower quadrant[16]. Coexisting inflammatory lesions referred to the inflammatory lesions seen in the CT scan that could be related with right low quadrant pain, such as diverticulitis or ovarian cysts.
Numeric data are presented as mean and standard deviation or as median and range. Continuous variables were analyzed with independent t-tests, and proportions were compared with Pearson χ2 or Fisher’s exact tests, as appropriate. For data that were not normally distributed, Wilcoxon rank-sum tests were used to examine differences in central tendency. Statistical analyses were performed with SPSS version 18.0 (SPSS Inc., Chicago, IL, United States). Two-tailed P values < 0.05 were considered statistically significant.
We analyzed the database of 224 patients who underwent operations with the suspicion of appendicitis based on clinical manifestations despite negative or equivocal CT interpretation. Of these, 177 patients had appendicitis and 47 patients did not. There were 88 men and 136 women with a mean age of 35.3 ± 20.1 years. The mean body mass index was 22.3 ± 3.5 kg/m2. Most patients (88.8%) did not present with high fever (≥ 37.8 °C). The mean serum leukocyte count was 10357 ± 4208/mm3. Baseline and clinical features, including findings obtained from history taking, physical examination, and laboratory results, were similar between the NA and PA groups (Table 1), except for platelet count (P = 0.005), creatinine level (P = 0.036) and serum bilirubin concentration (P = 0.020).
| Characteristics | Total population | Negative appendicitis | Pathologically proven appendicitis | P value |
| (n = 224) | (n = 47) | (n = 177) | ||
| Age (yr) | 0.052 | |||
| < 15 | 26 (11.6) | 10 (21.3) | 16 (9.0) | |
| 15-64 | 169 (75.4) | 33 (70.2) | 136 (76.9) | |
| ≥ 65 | 29 (13.0) | 4 (8.5) | 25 (14.1) | |
| Gender | 0.092 | |||
| Male | 88 (39.3) | 13 (27.7) | 75 (42.4) | |
| Female | 136 (60.7) | 34 (72.3) | 102 (57.6) | |
| Body mass index (kg/m2) | 0.635 | |||
| < 20 | 52 (27.1) | 12 (31.6) | 40 (26.0) | |
| 20-25 | 106 (55.2) | 21 (55.2) | 85 (55.2) | |
| > 25 | 34 (17.7) | 5 (13.2) | 29 (18.8) | |
| Comorbidity | 0.350 | |||
| Charlson index = 0 | 217 (96.9) | 47 (100.0) | 170 (96.0) | |
| Charlson index > 0 | 7 (3.1) | 0 (0.0) | 7 (4.0) | |
| Symptom duration before presentation | 0.740 | |||
| < 72 h | 129 (58.1) | 26 (55.3) | 103 (58.9) | |
| ≥ 72 h | 93 (41.9) | 21 (44.7) | 72 (41.1) | |
| Body temperature (°C) | 0.755 | |||
| < 37.8 | 119 (88.8) | 28 (87.5) | 91 (89.2) | |
| ≥ 37.8 | 15 (11.2) | 4 (12.5) | 11 (10.8) | |
| Presenting symptom | 0.507 | |||
| Abdominal pain | 219 (97.8) | 47 (100.0) | 172 (97.2) | |
| Indigestion | 1 (0.4) | 0 (0.0) | 1 (0.6) | |
| Fever/chill | 4 (1.8) | 0 (0.0) | 4 (2.2) | |
| Pain migration | 0.507 | |||
| No | 114 (53.3) | 26 (57.8) | 88 (52.1) | |
| Yes | 100 (46.7) | 19 (42.2) | 81 (47.9) | |
| Degree of tenderness | 0.383 | |||
| Mild | 4 (1.8) | 0 (0.0) | 4 (2.3) | |
| Moderate | 217 (96.9) | 47 (100.0) | 170 (96.0) | |
| Severe | 3 (1.3) | 0 (0.0) | 3 (1.7) | |
| RLQ localization of pain | 0.559 | |||
| Discrete | 205 (91.5) | 42 (89.4) | 163 (92.1) | |
| Obscure | 19 (8.5) | 5 (10.6) | 14 (7.9) | |
| Lab findings, median (range) | ||||
| WBC count (× 103/mm3) | 9.55 (4.0-29.1) | 9.3 (4.6-25.9) | 9.6 (4.0-29.1) | 0.833 |
| Platelet count (× 103/mm3) | 250 (157- 564) | 277 (202-564) | 241 (157-341) | 0.005 |
| Creatinine (mg/dL) | 0.64 (0.41- 1.11) | 0.56 (0.41-0.69) | 0.70 (0.46-1.11) | 0.036 |
| Albumin (g/dL) | 4.30 (3.3-5.4) | 4.40 (3.3-5.2) | 4.30 (3.3-5.4) | 0.989 |
| Total bilirubin (mg/dL) | 0.50 (0.2-1.5) | 0.55 (0.2-1.5) | 0.77 (0.2-2.2) | 0.020 |
| Neutrophil fraction | 0.359 | |||
| < 80% | 160 (72.4) | 36 (78.3) | 124 (70.9) | |
| ≥ 80% | 61 (27.6) | 10 (21.7) | 51 (29.1) | |
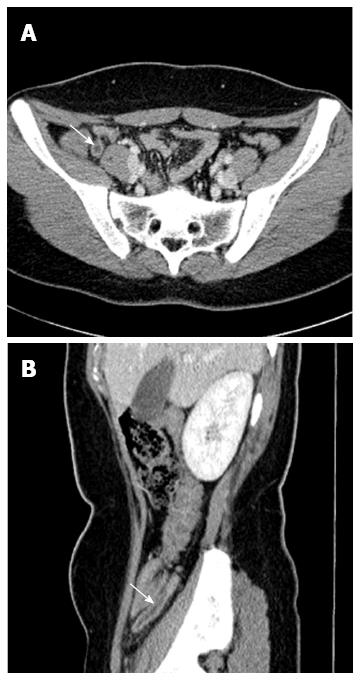
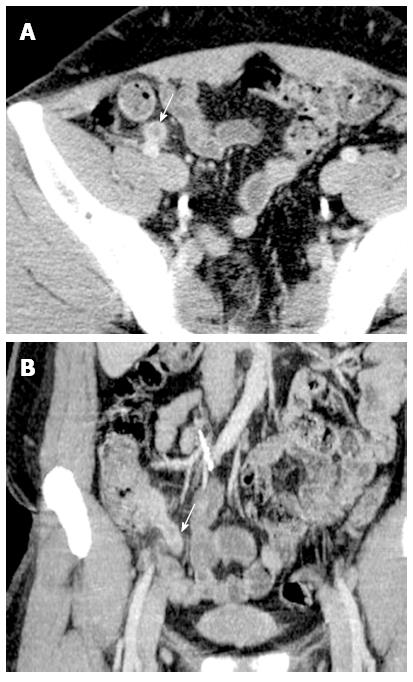
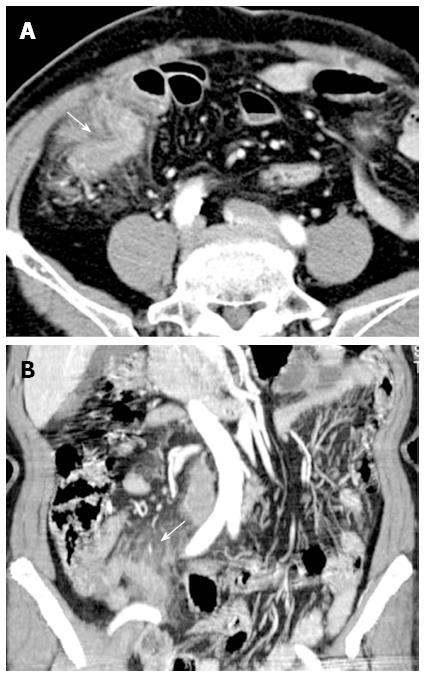
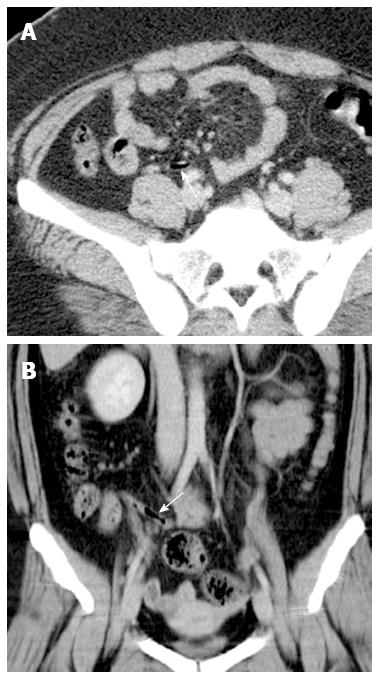
We re-evaluated the CT scans of the 224 patients included in the study (Table 2). Of these, the features indicative of appendicitis were appendiceal visualization, appendiceal diameter ≥ 6.0 mm, appendiceal wall enhancement (Figure 2), appendiceal wall thickening ≥ 2.0 mm (Figure 3), presence of appendicolith, periappendiceal fat stranding (Figure 4), periappendiceal fluid collection, and mesenteric lymphadenopathy. The features excluding appendicitis were the presence of intraluminal air (Figure 5) and coexisting inflammatory lesion(s). Of the features indicating appendicitis, the two groups showed significant differences in appendiceal diameter ≥ 6.0 mm and positive periappendiceal fat stranding (P < 0.001). Of the features excluding appendicitis, the two groups showed significant differences in the presence of intraluminal air (P = 0.024). There was no significant difference in the presence of co-existing inflammatory lesion(s) between the two groups. Ileocolitis (n = 37, 27.6%), terminal ileitis (n = 10, 7.5%), and periappendiceal fluid collections (n = 4, 3.0%) were the most frequently encountered lesions (Table 3).
| Total population | Negative appendicitis | Pathologically proven appendicitis | P value | |
| (n = 224) | (n = 46) | (n = 178) | ||
| Appendiceal visualization | 1.000 | |||
| No | 6 (2.7) | 1 (2.2) | 5 (2.8) | |
| Yes | 218 (97.3) | 45 (97.8) | 173 (97.2) | |
| Appendiceal diameter | < 0.001 | |||
| < 6.0 mm | 89 (39.7) | 29 (63.0) | 60 (33.7) | |
| ≥ 6.0 mm | 135 (60.3) | 17 (37.0) | 118 (66.3) | |
| Thickness of appendiceal wall | 0.175 | |||
| < 2.0 mm | 54 (24.1) | 15 (32.6) | 39 (21.9) | |
| ≥ 2.0 mm | 170 (75.9) | 31 (67.4) | 139 (78.1) | |
| Appendiceal wall enhancement | 0.059 | |||
| No | 138 (63.3) | 34 (75.6) | 104 (63.3) | |
| Yes | 80 (36.7) | 11 (24.4) | 69 (39.9) | |
| Presence of intraluminal air | 0.024 | |||
| No | 139 (63.8) | 22 (48.9) | 117 (67.6) | |
| Yes | 79 (36.2) | 23 (51.1) | 56 (32.4) | |
| Presence of appendicolith | 1.000 | |||
| No | 206 (94.5) | 43 (95.6) | 163 (94.2) | |
| Yes | 12 (5.5) | 2 (4.4) | 10 (5.8) | |
| Presence of periappendiceal fat stranding | 0.001 | |||
| No | 155 (71.1) | 41 (91.1) | 114 (65.9) | |
| Yes | 63 (28.9) | 4 (8.9) | 59 (34.1) | |
| Presence of periappendiceal fluid collection | 0.669 | |||
| No | 216 (96.4) | 44 (95.7) | 172 (96.6) | |
| Yes | 8 (3.6) | 2 (4.3) | 6 (3.4) | |
| Presence of periappendiceal lymphadenopathy | 1.000 | |||
| No | 200 (89.3) | 41 (89.1) | 159 (89.3) | |
| Yes | 24 (10.7) | 5 (10.9) | 19 (10.7) | |
| Presence of coexisting lesions | 0.084 | |||
| No | 169 (75.4) | 30 (65.2) | 139 (78.1) | |
| Yes | 55 (24.6) | 16 (34.8) | 39 (21.9) | |
| Coexisting lesions | Incidence (n) | % (n = 224) |
| Ileocolitis | 37 | 17.0 |
| Terminal ileitis | 10 | 4.5 |
| Periappendiceal fluid collection | 4 | 1.0 |
| Pelvic inflammatory disease | 2 | 0.9 |
| Epiploic appendigitis | 1 | 0.4 |
Based on the three factors significant for appendicitis in equivocal CT findings, we further evaluated the combination effect of these factors (Table 4). Of all possible combinations, we found that the greatest intergroup difference was seen when they were divided into low-risk (0-1 risk factor) and high-risk groups (2-3 risk factors). The probability of appendicitis in the high-risk group was 6.832 times higher than the low-risk group (95%CI: 3.013-15.454; P = 0.001).
Although several characteristic CT features for appendicitis have been revealed, their significance and frequencies have not been extensively studied. In this study, we applied these factors individually to the CT scans of which previous interpretations were negative or equivocal for appendicitis. As a result, we could arrange their priority. We identified three factors related to appendicitis: appendiceal diameter ≥ 6.0 mm, periappendiceal fat stranding, and the absence of intraluminal air. The patients who had two or more of these factors showed a significantly higher probability of appendicitis. We think that the application of our criteria would improve diagnostic accuracy of appendicitis, leading to a reduction in the rates of negative appendectomy and complications associated with delayed appendectomy.
The classical diagnostic criteria of appendicitis include appendiceal diameter of ≥ 7 mm; however, we found that the appendiceal diameter of 6 mm would be more helpful when encountered with equivocal CT findings. Actually, it is possible to have appendicitis with a 5-mm-appendiceal diameter, and to not have appendicitis with a 10-mm-appendiceal diameter. Therefore, appendiceal diameter alone is insufficient in making a diagnosis and should be supported by other more specific features.
Appendiceal wall thickening strongly suggests appendiceal inflammation. Administration of intravenous contrast media is essential for visualizing the appendiceal wall. Because all the patients in this study underwent contrast-enhanced CT scanning, we could estimate the presence of the appendiceal wall thickening. Our results indicate that appendiceal wall thickening did not strongly suggest appendicitis in patients with equivocal CT features. However, we think that further and more intensive study is required to validate this factor.
The extension of appendiceal inflammation to nearby mesenteric fat results in fat inflammation surrounding the appendix. Such fat inflammation is manifested as periappendiceal fat stranding on the CT scan. In previous studies, periappendiceal fat stranding was reported in more than 70% of patients with appendicitis[13,17,18]. In the present study, we showed that the presence of periappendiceal fat stranding is also a useful differential parameter when other CT findings are equivocal.
We also estimated whether it is helpful to detect intraluminal air in appendicitis when encountered in equivocal CT scans. The luminal obstruction by inspissated stool or lymphoid hyperplasia is believed to be the major cause of appendicitis[19]. The luminal obstruction promotes bacterial overgrowth and increases mucus secretion, leading to intraluminal distention and wall pressure elevation. Consequently, intraluminal air, which used to be easily observed in the normal appendix, can disappear in patients with appendicitis[20]. In a previous report, appendiceal intraluminal air was detected in 86% of patients without appendicitis and 15% of patients with appendicitis[14]. In this study, we also found that the presence of intraluminal air was a useful indicator for appendicitis in situations with the equivocal CT scans.
We acknowledge that this study had several limitations. First, because it was a retrospective study, our results should be confirmed by prospective trials. Next, due to the nature of this study, the study population size was relatively small (n = 224). However, the use of a single radiologist eliminates the possibility for differences in CT interpretation. Even when the patients suspicious for appendicitis visited the hospital after work hours and were immediately evaluated by the on-duty radiologist, the CT findings were re-assessed and confirmed by the radiologist in charge.
In conclusion, we found that when we encountered equivocal CT findings for appendicitis, the diagnostic accuracy would be enhanced by several characteristic CT features: appendiceal diameter ≥ 6.0 mm, appendiceal wall thickening ≥ 2.0 mm, periappendiceal fat stranding, and the absence of intraluminal air, rather than presence, as an indicator for appendicitis. By the application of these criteria, we could improve the diagnostic accuracy of appendicitis up to 6.8 times in patients with equivocal CT features. These characteristic CT features are not difficult to detect with instruction. Therefore, we recommend that not only radiologists, but also surgeons and physicians, could improve diagnostic accuracy of appendicitis by using these criteria.
The introduction of computed tomography (CT) has improved the diagnostic accuracy of appendicitis. However, CT may overlook about 10% patients with appendicitis because of its limited sensitivity and specificity. Therefore, clinicians frequently encounter patients who show equivocal CT findings for appendicitis, but who also have clinical manifestations of appendicitis.
Since CT scanning became widely used in the diagnosis of appendicitis, several CT features indicating appendicitis have been proposed; however, they have been used rather sporadically to date. Systematic utilization of these CT features would provide better discrimination between patients with and without appendicitis.
First, this study population was specifically chosen, and therefore well suited to the study. Of the 2596 patients who underwent appendectomy during a 6-y-period, the authors selected 224 patients who showed negative or equivocal CT findings for appendicitis, but thereafter were operated on for suspected appendicitis. Next, they thoroughly reviewed the literature concerning CT features of appendicitis, and determined the most reliable parameters. Thereafter, they systematically applied these features to the patient population. Finally, all the related CT images were re-evaluated by one radiologist with specialist experience in abdominal imaging. To avoid selection bias, the radiologist who re-evaluated CT images was not given information about the patient’s final diagnosis.
The authors have developed criteria which are useful when encountering patients with equivocal CT features: Appendiceal diameter ≥ 6.0 mm, appendiceal wall thickening ≥ 2.0 mm, periappendiceal fat stranding, and the absence of intraluminal air. By the application of these criteria, they could improve the diagnostic accuracy of appendicitis up to 6.8 times in patients with equivocal CT features.
The original article is well presented. The application of these criteria helps to improve the diagnostic accuracy in patients with symptoms and signs of appendicitis.
P- Reviewer: Kumar J S- Editor: Ding Y L- Editor: AmEditor E- Editor: Ma S
| 1. | Petrosyan M, Estrada J, Chan S, Somers S, Yacoub WN, Kelso RL, Mason RJ. CT scan in patients with suspected appendicitis: clinical implications for the acute care surgeon. Eur Surg Res. 2008;40:211-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Poh AC, Lin M, Teh HS, Tan AG. The role of computed tomography in clinically-suspected but equivocal acute appendicitis. Singapore Med J. 2004;45:379-384. [PubMed] |
| 3. | Wijetunga R, Tan BS, Rouse JC, Bigg-Wither GW, Doust BD. Diagnostic accuracy of focused appendiceal CT in clinically equivocal cases of acute appendicitis. Radiology. 2001;221:747-753. [PubMed] |
| 4. | Anderson SW, Soto JA, Lucey BC, Ozonoff A, Jordan JD, Ratevosian J, Ulrich AS, Rathlev NK, Mitchell PM, Rebholz C. Abdominal 64-MDCT for suspected appendicitis: the use of oral and IV contrast material versus IV contrast material only. AJR Am J Roentgenol. 2009;193:1282-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 61] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Krajewski S, Brown J, Phang PT, Raval M, Brown CJ. Impact of computed tomography of the abdomen on clinical outcomes in patients with acute right lower quadrant pain: a meta-analysis. Can J Surg. 2011;54:43-53. [PubMed] |
| 6. | Parks NA, Schroeppel TJ. Update on imaging for acute appendicitis. Surg Clin North Am. 2011;91:141-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Moteki T, Horikoshi H. New CT criterion for acute appendicitis: maximum depth of intraluminal appendiceal fluid. AJR Am J Roentgenol. 2007;188:1313-1319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Chalazonitis AN, Tzovara I, Sammouti E, Ptohis N, Sotiropoulou E, Protoppapa E, Nikolaou V, Ghiatas AA. CT in appendicitis. Diagn Interv Radiol. 2008;14:19-25. [PubMed] |
| 9. | Webb EM, Wang ZJ, Coakley FV, Poder L, Westphalen AC, Yeh BM. The equivocal appendix at CT: prevalence in a control population. Emerg Radiol. 2010;17:57-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Courtney M, Townsend J, Beauchamp BD, Mark Evers M, Mattox KL. Sabiston Textbook of surgery. The molecular basis of modern surgical practice. The appendix. 19th ed. Philadelphia: Elsevier 2012; 1281-1282. |
| 11. | Federle M, Jeffrey B, Woodward P, Borhani A. Diagnostic Imaging Abdomen. 2nd ed. Canada: Amirsys 2010; 26-28. |
| 12. | Sivit CJ, Siegel MJ, Applegate KE, Newman KD. When appendicitis is suspected in children. Radiographics. 2001;21:247-62; questionnaire 288-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 98] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 13. | Rao PM, Rhea JT, Novelline RA. Sensitivity and specificity of the individual CT signs of appendicitis: experience with 200 helical appendiceal CT examinations. J Comput Assist Tomogr. 1997;21:686-692. [PubMed] |
| 14. | Rettenbacher T, Hollerweger A, Macheiner P, Rettenbacher L, Frass R, Schneider B, Gritzmann N. Presence or absence of gas in the appendix: additional criteria to rule out or confirm acute appendicitis--evaluation with US. Radiology. 2000;214:183-187. [PubMed] |
| 15. | Applegate KE, Sivit CJ, Myers MT, Pschesang B. Using helical CT to diagnosis acute appendicitis in children: spectrum of findings. AJR Am J Roentgenol. 2001;176:501-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Foley TA, Earnest F, Nathan MA, Hough DM, Schiller HJ, Hoskin TL. Differentiation of nonperforated from perforated appendicitis: accuracy of CT diagnosis and relationship of CT findings to length of hospital stay. Radiology. 2005;235:89-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 17. | Jacobs JE, Birnbaum BA, Macari M, Megibow AJ, Israel G, Maki DD, Aguiar AM, Langlotz CP. Acute appendicitis: comparison of helical CT diagnosis focused technique with oral contrast material versus nonfocused technique with oral and intravenous contrast material. Radiology. 2001;220:683-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 119] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 18. | Raptopoulos V, Katsou G, Rosen MP, Siewert B, Goldberg SN, Kruskal JB. Acute appendicitis: effect of increased use of CT on selecting patients earlier. Radiology. 2003;226:521-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 42] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Prystowsky JB, Pugh CM, Nagle AP. Current problems in surgery. Appendicitis. Curr Probl Surg. 2005;42:688-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 44] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 20. | Rao PM, Rhea JT, Novelline RA. Appendiceal and peri-appendiceal air at CT: prevalence, appearance and clinical significance. Clin Radiol. 1997;52:750-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |