Published online Sep 21, 2014. doi: 10.3748/wjg.v20.i35.12701
Revised: April 29, 2014
Accepted: June 12, 2014
Published online: September 21, 2014
Processing time: 179 Days and 9.2 Hours
Patients with esophageal cancer often require esophagectomy with esophagogastrostomy. However, the incidence of complications, such as hemorrhage, during operations for esophageal cancer is high, even with minimally invasive surgery. Without the appropriate interventions, the risk of major intraoperative and postoperative hemorrhage is very high in patients with esophageal cancer and hemophilia. We report the case of a 45-year-old man with esophageal cancer and hemophilia B who underwent a successful hybrid, minimally invasive Ivor-Lewis esophagectomy with appropriate perioperative management.
Core tip: The incidence of complications, such as hemorrhage, in operations for esophageal cancer is high, even with minimally invasive surgery. Without the appropriate interventions, the risk of major intraoperative and postoperative hemorrhage is very high in patients with esophageal cancer and hemophilia. We report the case of a 45-year-old man with esophageal cancer and hemophilia B who underwent a successful hybrid, minimally invasive Ivor-Lewis esophagectomy with appropriate perioperative management.
- Citation: Zhang GF, Chai Y, Li WS, Huang LS, Shen G. Successful esophagectomy in a patient with combined esophageal cancer and hemophilia B. World J Gastroenterol 2014; 20(35): 12701-12703
- URL: https://www.wjgnet.com/1007-9327/full/v20/i35/12701.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i35.12701
Patients with esophageal cancer often require esophagectomy with esophagogastrostomy; these procedures entail open and minimally invasive surgeries. The incidence of postoperative complications, such as postoperative hemorrhage, in operations for esophageal cancer is high, even with minimally invasive surgery[1,2]. Without the appropriate interventions, the risk for major intraoperative and postoperative hemorrhage, even for minor procedures such as oral surgery, is very high in patients with hemophilia. Although studies describing the perioperative management for reducing the risk for postoperative hemorrhage in hemophilia patients have been published, no case reports are available on the perioperative management of patients with esophageal cancer and hemophilia who have undergone esophagectomy; thus, the treatment options for these patients remain unclear[3]. We present the case of a 45-year-old man with esophageal cancer and hemophilia B who underwent a successful hybrid, minimally invasive Ivor-Lewis esophagectomy. We also discuss the surgical management of patients with esophageal cancer combined with hemophilia.
The patient, a 45-year-old man, was admitted because of a 1-month history of dysphagia. No significant abnormalities were identified on physical examination, and no superficial bleeding or bruising was noted. After admission, an endoscopy indicated a mass lesion 35 cm from the incisors, and the pathological results suggested esophageal squamous cell carcinoma. The patient’s surgical history included the removal of an abdominal hematoma 10 years earlier. The patient denied other significant medical history. The post-admission coagulation test results showed an activated partial thromboplastin time of 59.8 s (normal: 22-40 s) and a thrombin time of 20.1 s (normal: 13-18 s). However, normal prothrombin time, bleeding time, international normalized ratio, and d-dimer values were noted. The patient’s platelet count and liver function tests were normal. In further coagulation factor tests, the coagulation factor IX level was only 4.1% (normal: 50%-150%), whereas the levels of factors VIII, XI, and XII were normal. The patient’s antinuclear antibodies and immunoglobulins were all within the reference ranges. Based on these results, the patient was diagnosed with esophageal squamous cell carcinoma combined with hemophilia B.
The main goal of the preoperative preparation was to improve the activity of coagulation factor IX in this patient. The patient received an intravenous infusion of 1200 U of prothrombin complex twice per day. The coagulation factor IX level was remeasured 3 d later. The activity of coagulation factor IX improved to 44.1%, and surgery was arranged for the patient.
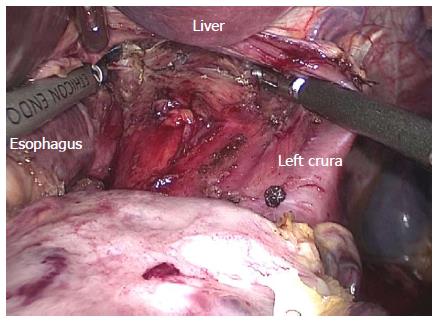
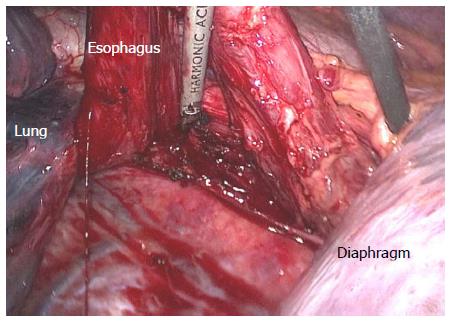
We performed a hybrid, minimally invasive Ivor-Lewis esophagectomy. First, the gastric mobilization, abdominal lymph node dissection, and jejunostomy were performed under laparoscopy with the patient in the supine position (Figure 1). Then, the esophageal mobilization and resection, thoracic lymph node dissection, gastric conduit construction, and esophagogastrostomy were performed via a sixth intercostal thoracotomy with the patient in the left lateral decubitus position (Figure 2).
The entire operation lasted 175 min; the abdominal procedures took 50 min, and the thoracic procedures took 125 min. The amount of intraoperative blood loss was 200 mL. The patient received a postoperative continuous infusion of 1200 U prothrombin complex concentrate once per day. On postoperative day 4, the activity of coagulation factor IX was determined to be 42%, and the infusion was discontinued after 10 postoperative days.
The patient had an uneventful postoperative recovery with no significant postoperative hemorrhage. He was extubated 22 h after the operation. The chest tube was removed on postoperative day 7. Esophagography was performed 6 d after the operation, with no contrast media leakage. The patient resumed food intake by postoperative day 7. The postoperative pathological examination results revealed stage IIIA cancer; thus, radiotherapy was initiated at postoperative week 4. The patient has been undergoing follow-up for 19 mo, and no metastases have been observed by computed tomographic examination.
Even with the use of minimally invasive methods, perioperative complications are common in esophageal cancer surgeries[1,2]. Patients, especially those with a preoperative coagulopathy, are vulnerable to major intraoperative and postoperative hemorrhage. Although recent reports on the surgical treatment for patients with hemophilia have been published, no detailed case reports are available regarding major operations, such as esophagectomy. In this report, we present the case of an esophageal cancer patient with hemophilia B who underwent a successful hybrid, minimally invasive esophagectomy with perioperative intravenous infusion of a prothrombin complex concentrate to replenish and maintain the activity of coagulation factor IX at ≥ 40% of the normal value. We believe that surgical procedures could be safely performed in patients with hemophilia if the patients are provided with the appropriate perioperative management.
Some patients might not be aware that they have hemophilia before an operation. Therefore, further tests and hemophilia screens are essential for patients with preoperative coagulopathies to control the risk of intraoperative and postoperative hemorrhage[4]. In this case, the patient was diagnosed with hemophilia B after further tests for coagulation factor IX levels, which were measured as only 4.1% of the normal value, despite the fact that the preoperative PTT was only 10 s longer than the reference range and the results of the other tests, including prothrombin time, bleeding time, and platelet count, were all normal.
For patients with a coagulopathy, the selection of an appropriate surgical approach is important. First, the procedure should be consistent with oncological principles, and a radical resection should be performed if possible. Second, the operation should be completed quickly and safely, and the duration of the operation should be minimized to reduce the intraoperative loss of coagulation factors[5]. Finally, the procedure should be as minimally invasively as possible. In this case, we used a hybrid Ivor-Lewis esophagectomy to complete the gastric mobilization and jejunostomy in the abdomen under laparoscopy. In the thorax, we completed the esophageal mobilization and resection, mediastinal lymph node dissection, gastric conduit construction, and esophagogastrostomy via a right lateral thoracotomy under direct vision, which required less time than thoracoscopy. We believe that this surgical approach is consistent with the above-mentioned principles.
Currently, the appropriate perioperative supplementation of coagulation factors is controversial[6]. Direct supplementation of the deficient coagulation factors is the most direct and effective treatment; however, the direct infusion of coagulation factor concentrates is costly, involves a complicated sourcing process, and requires preoperative evaluations, including inhibitor screening[7]. The direct infusion of plasma (1200 mL/d) requires a large amount of fluid and might cause problems associated with long-term plasma transfusion, such as allergies and fever[5]. Perioperative intravenous infusions of the prothrombin complex concentrate that we used to replenish coagulation factor IX is a simple method, and the medication is easy to obtain. Based on the recommendations from the literature, we re-evaluated the coagulation factor IX levels after 3-4 d of preoperative infusions of the prothrombin complex concentrate. When the level improved to > 40% of the normal value, surgery was planned. The recommended duration of postoperative infusions of the prothrombin complex concentrate remains inconclusive. We believe that the infusions should be discontinued 1-2 d after removal of the chest tube to avoid intrathoracic hemorrhage upon extubation.
A 45-year-old man was admitted with a 1-month history of dysphagia.
No significant abnormalities were found during physical examination.
Benign esophageal tumor, achalasia of the cardia, and benign esophageal stricture were diagnosed.
The coagulation factor IX level was only 4.1% (normal: 50%-150%); however, the levels of factors VIII, XI, and XII were normal.
The endoscopy results indicated a mass lesion 35 cm from the incisors, and the pathological results suggested esophageal squamous cell carcinoma.
After the coagulation factor IX activity improved to 44.1% following intravenous infusions of prothrombin complex, a hybrid, minimally invasive Ivor-Lewis esophagectomy was performed.
No case reports are available on the perioperative management of patients with esophageal cancer and hemophilia undergoing esophagectomy.
Hemophilia B is a blood clotting disorder caused by a mutation in the Factor IX gene, leading to a deficiency in Factor IX.
For patients with combined esophageal cancer and hemophilia B, surgical treatment could be safely performed with appropriate perioperative management.
This article presents a case of an esophageal cancer patient with hemophilia B who underwent a successful hybrid, minimally invasive esophagectomy following perioperative intravenous infusions of a prothrombin complex concentrate to replenish coagulation factor IX.
P- Reviewer: Peltec A, Raggi C, Rodriguez-Castro KI, Ratnasari N, Sirin G S- Editor: Qi Y L- Editor: A E- Editor: Du P
| 1. | Luketich JD, Pennathur A, Awais O, Levy RM, Keeley S, Shende M, Christie NA, Weksler B, Landreneau RJ, Abbas G. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg. 2012;256:95-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 647] [Cited by in RCA: 623] [Article Influence: 47.9] [Reference Citation Analysis (0)] |
| 2. | Yamamoto M, Weber JM, Karl RC, Meredith KL. Minimally invasive surgery for esophageal cancer: review of the literature and institutional experience. Cancer Control. 2013;20:130-137. [PubMed] |
| 3. | Kulkarni R. Comprehensive care of the patient with haemophilia and inhibitors undergoing surgery: practical aspects. Haemophilia. 2013;19:2-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Skinner MW, Myles E. World Federation of Hemophilia: 50 years of advancing treatment for all. Haemophilia. 2013;19:475-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Makris M, Kasper C. The World Federation of Hemophilia guideline on management of haemophilia. Haemophilia. 2013;19:1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Lillicrap D. The World Federation of Hemophilia and research. Haemophilia. 2012;18 Suppl 4:24-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Skinner MW. Haemophilia: provision of factors and novel therapies: World Federation of Hemophilia goals and achievements. Br J Haematol. 2011;154:704-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |