Published online Jul 14, 2014. doi: 10.3748/wjg.v20.i26.8736
Revised: January 31, 2014
Accepted: March 6, 2014
Published online: July 14, 2014
Processing time: 188 Days and 1.6 Hours
Intraductal papillary mucinous neoplasm of the bile duct (IPNB) is recognized as a precancerous lesion; however, both its pathogenesis and progression remain unclear. We present here a case of IPNB arising from the gallbladder accompanied by bile duct tumor thrombus in a 79-year-old female. The resected specimen revealed a tubulopapillary adenoma with no malignant cells. This case suggests that even in the absence of malignant cells, these tumors can behave as malignant tumors requiring aggressive treatment. Even if no malignant cells are present, intraepithelial neoplasms occurring in the ampullopancreatobiliary tract can behave as malignant tumors.
Core tip: Intraductal papillary mucinous neoplasm of the bile duct (IPNB) has relatively recently been recognized as a separate disease entity with an unclear pathogenesis. We present a case of IPNB developing from the gallbladder accompanied by a bile duct tumor thrombus in a 79-year-old female. Although this is not a malignant lesion, it has the potential to mimic a malignant lesion, and hence needs aggressive treatment.
- Citation: Yamamoto K, Yamamoto F, Maeda A, Igimi H, Yamamoto M, Yamaguchi R, Yamashita Y. Tubulopapillary adenoma of the gallbladder accompanied by bile duct tumor thrombus. World J Gastroenterol 2014; 20(26): 8736-8739
- URL: https://www.wjgnet.com/1007-9327/full/v20/i26/8736.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i26.8736
Intraductal papillary mucinous neoplasm (IPMN) of the bile duct (IPNB) is a disease entity that was proposed in 2001 by Chen et al[1]. IPNB is regarded as a counterpart of IPMN of the pancreas, and is considered to be a precancerous lesion[2-5]. A similar spectrum of lesions also exists in the gallbladder[6]. However, these lesions have yet to be fully characterized and their pathogenesis and progression remain unclear. Most reported cases of invasive IPNB ultimately become cancerous. Generally, the tumors accompanied by a bile duct tumor thrombus are cancerous. Here we report a rare gallbladder tumor without cancerous changes accompanied by a bile duct tumor thrombus.
A 79-year-old female presented to our hospital for an incidentally-diagnosed gallbladder tumor. No abnormalities were seen in blood test results, including tumor markers. Laboratory data (normal range) were as follows: aspartate aminotransferase, 18 U/L (5-35 U/L); alanine aminotransferase, 14 U/L (5-30 U/L); alkaline phosphatase, 151 U/L (115-359 U/L); gamma-glutamyl transferase, 20 U/mL (0-50 U/mL); lactate dehydrogenase, 170 U/L (106-211 U/L); albumin, 4.0 g/dL (3.7-5.5 g/dL); and total bilirubin, 0.64 g/dL (0.2-1.0 g/dL). The concentrations of carcinoembryonic antigen and carbohydrate antigen 19-9 were 2.2 ng/mL (< 5.0 ng/mL) and 4.0 U/mL (< 37.0 U/mL), respectively. No serological evidence of hepatitis B or C was seen.
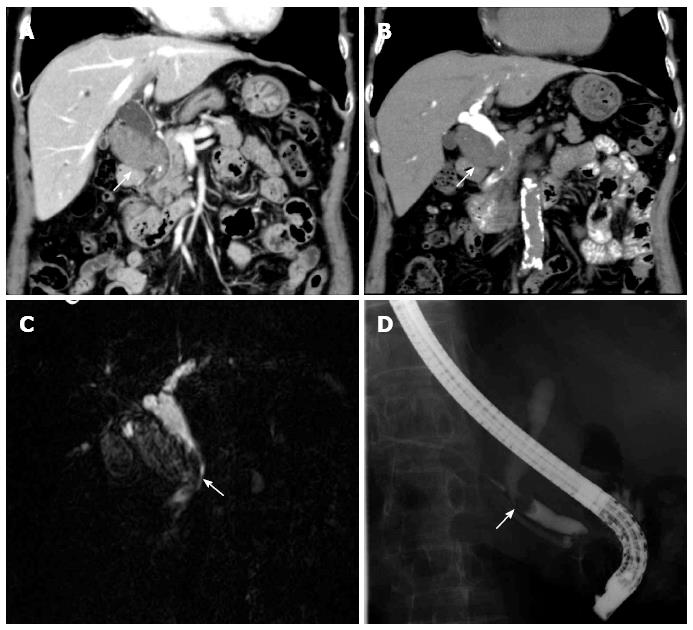
Contrast enhanced computed tomography (CT) revealed a tumor measuring 40 mm in diameter in the cystic duct, accompanied by a common bile duct tumor thrombus (Figure 1A). Drip infusion cholangiographic CT revealed a defect in the common bile duct (Figure 1B). Magnetic resonance cholangiopancreatography and endoscopic retrograde cholangiopancreatography revealed similar findings (Figure 1C and D). Cytological examination revealed the absence of malignant cells in bile. Without the evidence of malignant cells, we diagnosed it as gallbladder cancer or bile duct cancer because of the common bile duct tumor thrombus.
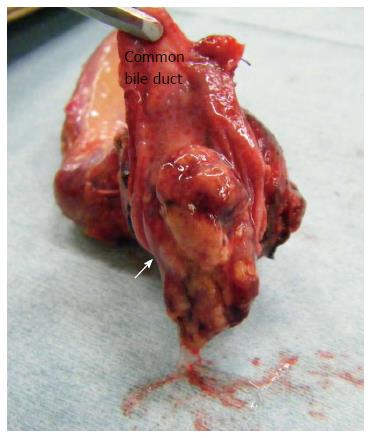
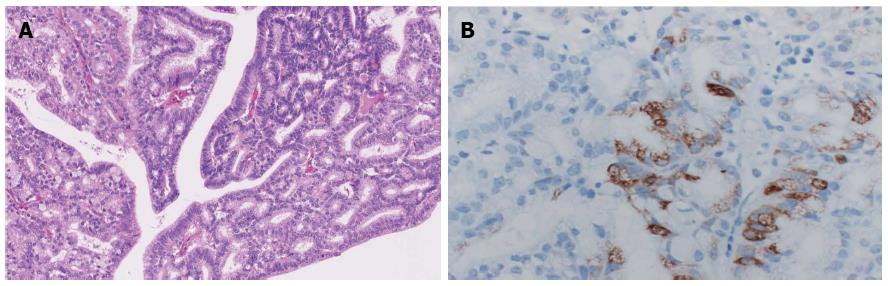
The patient underwent choledochectomy and cholecystectomy. Macroscopic examination of the resected specimen revealed a 40-mm tumor located in the neck of the gallbladder and a 30-mm tumor thrombus in the common bile, with rich mucilage (Figure 2). Microscopically, hematoxylin and eosin staining demonstrated the tumor to be a pyloric type tubulopapillary adenoma with moderate epithelial atypia, without evidence of stromal invasion (Figure 3). On immunological staining, the tumor cells were positive for MUC5AC, but negative for MUC1 and CK20.
Recently, intraepithelial neoplasms occurring in the ampullopancreatobiliary tract have attracted a substantial amount of attention. These include the so-called IPNB, IPMN of the pancreas, intraductal tubulopapillary neoplasms (ITPN) of the pancreas, intra-ampullary-tubular neoplasms (IAPN) and intracystic papillary neoplasms (ICPN) of the gallbladder[1-6]. IPNB, IPMN, and ITPN are recognized by the World Health Organization[7]. IPNB, on the other hand, is a relatively recently proposed (in 2001) disease entity[1] which has been shown to be histologically similar to IPMN[2-5]. A similar spectrum of lesions also exists in IAPN and ICPN; however, these have not been fully characterized[6].
IPNBs are histologically classified as low- or intermediate-grade intraepithelial neoplasia corresponding to adenomas or borderline malignancy, high grade intraepithelial neoplasia corresponding to carcinoma in situ, or as having an associated invasive carcinoma[5,6]. The neoplasms are regarded as precancerous lesions; therefore, radical resection is recommended in operable patients[4,5,8,9].
In our case, although the epithelial atypia was moderate, it was accompanied by a bile duct tumor thrombus. The neoplasms accompanied with tumor thrombus are often ordinary invasive carcinoma[10,11]. What is curious is that no symptoms of biliary tract obstruction were observed in our patient, although we cannot rule out the possibility that such symptoms could have occurred in the immediate future. Furthermore, it is reported that pyloric type adenocarcinoma of the gallbladder has a poor prognosis[12]. So, in our case, surgical treatment is considered reasonable and proper.
Even if no malignant cells are present, intraepithelial neoplasms occurring in the ampullopancreatobiliary tract can behave as malignant tumors. Hence, these patients should be treated aggressively.
A 79-year-old female with an incidentally-diagnosed gallbladder tumor accompanied by bile duct tumor thrombus.
The patient was diagnosed with gallbladder carcinoma by the imaging study.
Differential diagnoses were bile duct carcinoma invaded to the gallbladder, malignant lymphoma and intraductal papillary mucinous neoplasm of the bile duct.
All of the laboratory tests were within normal limits.
Computed tomography revealed a tumor measuring 40 mm in diameter in the cystic duct, accompanied by a common bile duct tumor thrombus. Drip infusion cholangiographic-computed tomography, magnetic resonance imaging, endoscopic retrograde cholangiopancreatography revealed a defect in the common bile duct.
Cytological examination revealed the absence of malignant cells in bile. Microscopically, resected specimen revealed a pyloric type tubulopapillary adenoma with moderate epithelial atypia.
The patient underwent choledochectomy and cholecystectomy.
Intraductal papillary mucinous neoplasms of the bile duct are histologically classified as low- or intermediate-grade intraepithelial neoplasia corresponding to adenomas or borderline malignancy, high grade intraepithelial neoplasia corresponding to carcinoma in situ, or as having an associated invasive carcinoma. The neoplasms accompanied with tumor thrombus are often ordinary invasive carcinoma.
Intraductal papillary mucinous neoplasm of the bile duct is a recently recognized disease entity whose behavior is still unclear.
Although the epithelial atypia was moderate, it was accompanied by a bile duct tumor thrombus. Even if no malignant cells are present, intraepithelial neoplasms occurring in the ampullopancreatobiliary tract can behave as malignant tumors. Hence, these patients should be treated aggressively.
This article applies the validity of surgical treatment for intraepithelial neoplasms occurring in the ampullopancreatobiliary tract, even if it is an adenoma.
P- Reviewer: Wang DS S- Editor: Gou SX L- Editor: Wang TQ E- Editor: Wang CH
| 1. | Chen TC, Nakanuma Y, Zen Y, Chen MF, Jan YY, Yeh TS, Chiu CT, Kuo TT, Kamiya J, Oda K. Intraductal papillary neoplasia of the liver associated with hepatolithiasis. Hepatology. 2001;34:651-658. [PubMed] |
| 2. | Bickenbach K, Galka E, Roggin KK. Molecular mechanisms of cholangiocarcinogenesis: are biliary intraepithelial neoplasia and intraductal papillary neoplasms of the bile duct precursors to cholangiocarcinoma? Surg Oncol Clin N Am. 2009;18:215-24, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Nakanuma Y, Zen Y, Harada K, Ikeda H, Sato Y, Uehara T, Sasaki M. Tumorigenesis and phenotypic characteristics of mucin-producing bile duct tumors: an immunohistochemical approach. J Hepatobiliary Pancreat Sci. 2010;17:211-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Rocha FG, Lee H, Katabi N, DeMatteo RP, Fong Y, D’Angelica MI, Allen PJ, Klimstra DS, Jarnagin WR. Intraductal papillary neoplasm of the bile duct: a biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas? Hepatology. 2012;56:1352-1360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 183] [Article Influence: 14.1] [Reference Citation Analysis (2)] |
| 5. | Kubota K, Nakanuma Y, Kondo F, Hachiya H, Miyazaki M, Nagino M, Yamamoto M, Isayama H, Tabata M, Kinoshita H. Clinicopathological features and prognosis of mucin-producing bile duct tumor and mucinous cystic tumor of the liver: a multi-institutional study by the Japan Biliary Association. J Hepatobiliary Pancreat Sci. 2014;21:176-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 6. | Adsay V, Jang KT, Roa JC, Dursun N, Ohike N, Bagci P, Basturk O, Bandyopadhyay S, Cheng JD, Sarmiento JM. Intracholecystic papillary-tubular neoplasms (ICPN) of the gallbladder (neoplastic polyps, adenomas, and papillary neoplasms that are ≥1.0 cm): clinicopathologic and immunohistochemical analysis of 123 cases. Am J Surg Pathol. 2012;36:1279-1301. [PubMed] |
| 7. | Kloppel G, Hruban RH, Longnecker DS, Adler G, Kern SE, Partanen TJ. Ductal adenocarcinoma of the pancreas. Pathology and genetics of tumours of the digestive system. Lyon: IARC Press 2000; 221. |
| 8. | Nanashima A, Kinoshita N, Nakanuma Y, Zen Y, Sumida Y, Abo T, Hidaka S, Takeshita H, Yasutake T, Hayashi T. Clinicopathological features of “intraductal papillary neoplasm of the bile duct” and patient outcome after surgical resection. Hepatogastroenterology. 2008;55:1167-1173. [PubMed] |
| 9. | Jung G, Park KM, Lee SS, Yu E, Hong SM, Kim J. Long-term clinical outcome of the surgically resected intraductal papillary neoplasm of the bile duct. J Hepatol. 2012;57:787-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 78] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Midorikawa Y, Kubota K, Komatsu Y, Hasegawa K, Koike Y, Mori M, Makuuchi M. Gallbladder carcinoma with a tumor thrombus in the common bile duct: an unusual cause of obstructive jaundice. Surgery. 2000;127:473-474. [PubMed] |
| 11. | Xin-Wei Y, Jue Y, Bao-Hua Z, Feng S. An unusual gallbladder carcinoma with tumor thrombus in the common bile duct. J Cancer Res Ther. 2013;9:122-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Albores-Saavedra J, Chablé-Montero F, Méndez-Sánchez N, Mercado MÁ, Vilatoba-Chapa M, Henson DE. Adenocarcinoma with pyloric gland phenotype of the extrahepatic bile ducts: a previously unrecognized and distinctive morphologic variant of extrahepatic bile duct carcinoma. Hum Pathol. 2012;43:2292-2298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |