Published online Jun 14, 2014. doi: 10.3748/wjg.v20.i22.6878
Revised: February 17, 2014
Accepted: March 19, 2014
Published online: June 14, 2014
Processing time: 219 Days and 19.8 Hours
AIM: To explore the technique for laparoendoscopic single-site distal pancreatectomy.
METHODS: Laparoendoscopic single-site spleen-preserving distal pancreatectomy was performed in pigs using a novel flexible multichannel port, a curved laparoscopic multifunctional operative device and a fish hook retractor, which provided a favorable operative field.
RESULTS: Six pigs were involved in this study, and five survived the procedure. The first animal died following injury to the superior mesenteric vein and uncontrolled intraoperative bleeding. Except for this failure, the mean operative time was 155 min (range: 102-236 min). A steep learning curve was observed in the study, with a mean operative time of 177 min in the first two operations vs 134 min in the last three operations. The mean blood loss was 50 mL, and the postoperative course was uneventful. The animals were sacrificed three weeks after the procedures, and no pancreatic leakage or abdominal infection was found macroscopically.
CONCLUSION: Laparoendoscopic single-site distal pancreatectomy is a safe and feasible procedure and can be implemented in humans in selected cases at qualified surgical centers.
Core tip: Laparoendoscopic single-site surgery (LESS) is a rapidly evolving field in minimally invasive surgery. LESS requires specialized instruments and is a technically demanding procedure that is particularly challenging for pancreatic surgery. We present our surgical technique for laparoendoscopic single-site distal pancreatectomy in pigs using a novel flexible multichannel port, a curved laparoscopic multifunctional operative device and a fish hook retractor, which provided a favorable operative field. It is a safe and feasible procedure and can be implemented in humans in selected cases. To our knowledge, this is the first surgical series of laparoendoscopic single-site distal pancreatectomy in pigs reported in the literature.
- Citation: Wang D, Ji ZL, Jiang XH, Wang JM, Tan YY, Wang Y, Wen YZ. Laparoendoscopic single-site distal pancreatectomy in pigs. World J Gastroenterol 2014; 20(22): 6878-6883
- URL: https://www.wjgnet.com/1007-9327/full/v20/i22/6878.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i22.6878
Laparoendoscopic single-site surgery (LESS) is an emerging technique that has been suggested as a promising alternative to conventional laparoscopic surgery for the management of many common diseases[1,2]. LESS requires specialized instruments and is a technically demanding procedure that is particularly challenging for sophisticated operations, such as pancreatic surgery[3-6]. In this study, we present a surgical technique for laparoendoscopic single-site spleen-preserving distal pancreatectomy (LESS-SPDP) in pigs using articulating instruments and specially designed devices. This is the first report of this procedure in pigs and may provide a basis for performing advanced LESS in human beings.
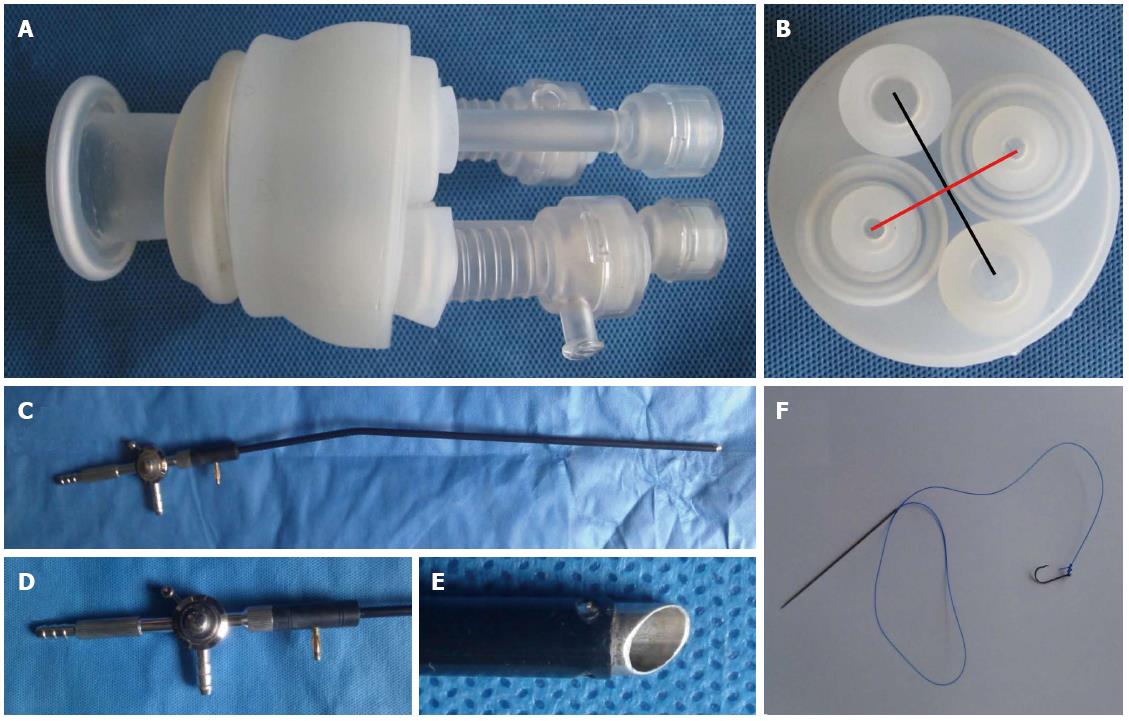
A novel flexible multichannel port (designed by us, and manufactured by Kang Mei Sci and Tech, Jiangsu, China) was introduced in this study. The port consists of a wound retractor and a valve component as well as trocars. The retractor is a cylindrical sleeve of silicon material with distal and proximal rings. The distance between the two rings is approximately 3 cm and can extend to approximately 4.5 cm with increasing abdominal wall thickness. The valve component acts like a cap and has four channels that allow the laparoscope and instruments of different sizes (5-10 mm) to pass through. The remarkable advantages of the cap component are the wide distance between the channels and the flexible characteristics, which provide a broad operative fulcrum and are particularly suitable for articulated instruments (Figure 1A and B).
A laparoscopic multifunctional operative device (LMOD or Ji-rod) was built, according to the author’s patent, and had already been used in laparoscopic surgery[7]. We modified the standard LMOD to a curved LMOD (C-LMOD). It is a combination of an electric coagulation device and irrigation equipment, with a curve of approximately 20°-30° near the handle to avoid extraperitoneal counteraction and improve ergonomic maneuvering in LESS (Figure 1C-E). The C-LMOD has the same functions as the LMOD for intraoperative cutting, coagulation, curettage, dissection, irrigation and aspiration.
Transabdominal stay sutures by fish hooks were introduced in this study. A midsized fish hook has a hole on the tail, and the barb at the tip was removed. A straight needle with a 2-0 Prolene was tied on the fish hook hole (Figure 1F). The fish hook retractor is effective and reliable for traction. There are two methods to release the fish hook. One method is by introducing a Prolene straight needle stay suture, tying the hook through the port. The straight needle punctures the abdominal wall with a grasper from the abdominal cavity to the exterior. The hook is placed in the organ or peritoneum, and pulling the suture provides enough operating space. The second method is to insert the straight needle from the planned skin incision site into the abdominal cavity, using a grasper to pull the needle out through the port; the suture is then tied to the hook hole on the exterior. Finally, the hook is introduced into the abdominal cavity for retraction.
To avoid collisions and to rebuild the operative triangulation, articulating instruments were utilized in the procedure, including graspers and scissors (YouShi, ZheJiang, China), ENDO GIA staplers (Covidien, MA, United States) and a 5-mm flexible EndoEye™ laparoscope (Olympus, Center Valley, United States).
Six domestic pigs (range: 25-31 kg) were included in this study to explore the feasibility of LESS-SPDP. The protocol was approved and recorded by the Ethics Committee of Southeast University Medical School.
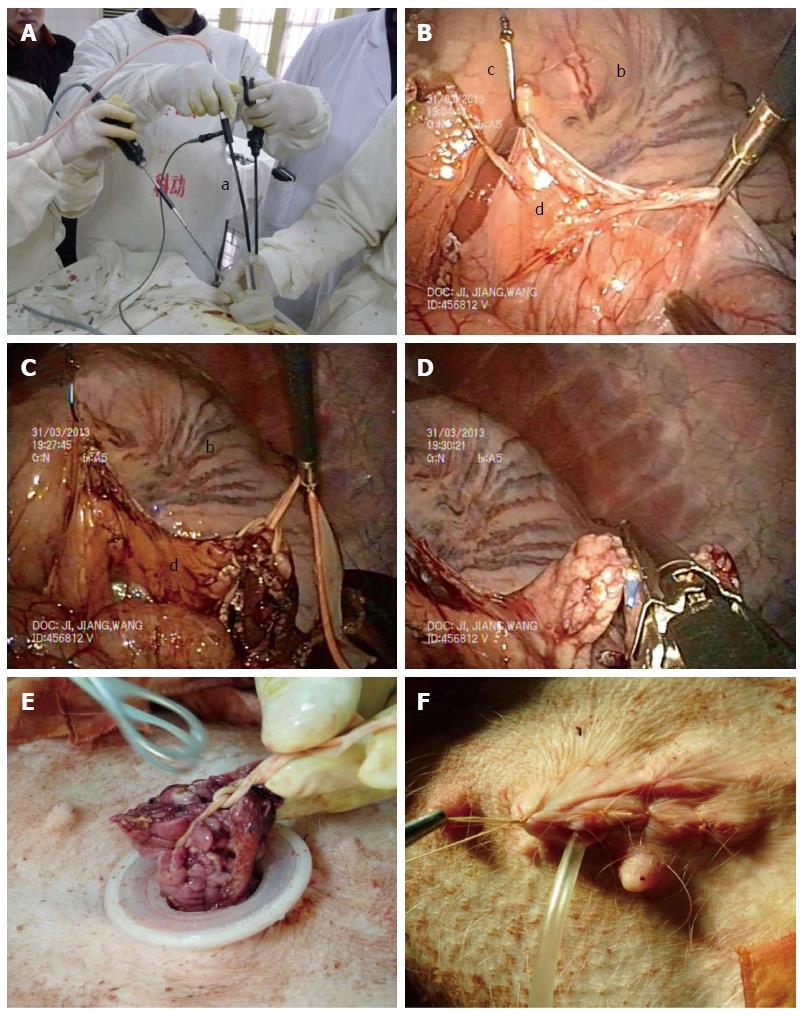
A pig was placed in a supine and reverse Trendelenburg position, with the right side rotated down, after the induction of general anesthesia. The surgeon stood on the pig’s tail side; the cameraman and assistant were on the surgeon’s right and left side, respectively. After skin preparation, an approximately 2.5 cm longitudinal incision was made in the abdominal wall near the umbilicus. The Hasson method[8] was applied to enter the abdominal cavity, and a wound retractor was inserted into the incision. The valve component covered the outer ring of the retractor, and the trocars were passed through the valve. The gas tube was connected to the port, and a pneumoperitoneum was established at 6-8 mmHg.
The EndoEye™ laparoscope, articulating graspers and C-LMOD were inserted into the abdominal cavity through the port. To obtain convenient operative triangulation and avoid extraperitoneal clashing, instruments were inserted into the abdomen in an inverted-pyramid position on the valve, i.e., the laparoscope was at the bottom and the articulating instrument and the C-LMOD were on the top channels (Figure 2A). The gastrocolic ligament was divided to expose the pancreas, as in the conventional technique. To obtain a sufficient operating space and ensure an adequate laparoscopic view, the greater curvature of the stomach and the pancreatic capsule were suspended towards the xiphoid using two fish hook retractors (Figure 2B). The suspending position was identified by palpating the abdominal wall, and the suspending distance depended on the exposure. The gastric epithelium and pancreatic capsule were strong enough to be retracted with the fish hooks. At the point where transection of the pancreas would be carried out, the inferior edge of the pancreatic capsule was incised and a tunnel was created beneath the body of the pancreas from the caudal to cephalad using the C-LMOD; thus, the pancreatic parenchyma was mobilized from the retroperitoneal and splenic vessels (Figure 2C). The superior mesenteric and splenic vessels were important during the procedure, and the C-LMOD was used to dissect the pancreatic parenchyma away from these vessels, using blunt dissection with the slope on the tip. A flexible sling was passed through the tunnel by an articulating grasper to lift the pancreas ventrally, and the pancreas was transected using a 60-mm ENDO GIA stapler (Figure 2D). The distal pancreas was removed using a medial-to-lateral method, i.e., the resection was performed from the body of the pancreas to the tail. The short transverse branches of the splenic vessels were individually isolated and sealed by titanium clips. After the distal pancreas was completely mobilized from the retroperitoneum, it was extracted through the wound retractor as an intact piece (Figure 2E). If the proximal pancreatic stump was not satisfying, it was reinforced with fibrin glue. The fish hook retractors were removed, and a drainage catheter was placed in the pancreatic bed through the sole incision. The incision was closed with absorbable sutures (Figure 2F).
Six pigs were involved in this study, and five survived the procedure. The first animal died following injury to the superior mesenteric vein and uncontrolled intraoperative bleeding. Except for this failure, the mean operative time was 155 min (range: 102-236 min). A steep learning curve was observed in the study, with a mean operative time of 177 min in the first two operations vs 134 min in the last three operations. The mean blood loss was 50 mL, and the postoperative course was uneventful. A liquid diet was begun on the second postoperative day after fasting for 24 h. A normal diet was begun on the third day, and the weight of the pigs began to increase after 10.6 d (range: 6-15 d). The animals were sacrificed three weeks after the procedure, and no pancreatic leakage or abdominal infection was found macroscopically.
LESS is a positive development in the field of minimally invasive surgery, requiring only one incision that is disguised within the umbilical folds, which is in contrast to the, at least three, necessary incisions for conventional laparoscopic surgery. The potential advantages of LESS are its comparable safety, improved cosmetic results, decreased complications, reduced postoperative pain and shorter postoperative stay[9,10]. Given the complexity of this novel technique, LESS is performed mostly in common procedures, such as appendectomy and cholecystectomy. For complicated pancreatic surgery, dedicated instruments and advanced skills are necessary to compensate for the shortcomings of LESS.
A number of multichannel access ports have been introduced for use in LESS[11,12]. From the literature, we can conclude that a wide distance between the channels of the multichannel port provides a broad fulcrum, which is important for LESS[13,14]. This is the main characteristic of our novel port. The distance between the channels is wider than most of the available multichannel devices and has been demonstrated to reduce instrumental collision in our procedures. Another advantage of the novel multichannel cannula is the flexible characteristics that are especially suitable for articulated instruments and devices with larger diameters, such as the 12-mm ENDO GIA stapler used in this study, while maintaining the pneumoperitoneum perfectly without the trocars.
To avoid the frequent replacement of instruments, we redesigned the LMOD to the C-LMOD. As described previously[7], the LMOD has many functions, including scraping, dissecting, cutting, coagulating, irrigating and aspirating. By using this device, we can perform many types of manipulations without instrumental substitution. The C-LMOD can evacuate smoke quickly to maintain clear laparoscopic vision, while the electrocautery is in use. This is useful in LESS. In our experience, articulating devices are necessary to provide intraperitoneal triangulation and avoid extraperitoneal collisions. The next step for the development of the C-LMOD is to cooperate with a medical device manufacture to design an articulating laparoscopic multifunctional operative device.
The introduction of two working instruments and a laparoscope parallel to one another through one incision results in extraperitoneal collisions and a lack of intraperitoneal triangulation[11]. Specially designed articulating instruments and laparoscopes can reestablish the triangulation and provide a favorable laparoscopic view[15]. There are only four such case reports in Pubmed[3-6]. Consistent with our technique, articulating instruments were involved in all of these studies. The changes in the operative manner produce a significant learning curve for both the surgeon and the camera operator[16]. In our surgical series, the operative time decreases as more cases are performed. It is worth noting that LESS should be performed by experienced laparoscopic surgeons, and it is better for the camera operator to have experience operating a flexible endoscope before operating the articulating flexible EndoEye™ laparoscope. For novices, adequate training on a simulator is necessary to become familiar with rules of LESS and the specially designed devices.
Retraction is another key point in our technique. Although articulating graspers could perform some retraction, a suitable operative field should be provided by another device at a more favorable angle. In the studies by Barbaros et al[3] and Kuroki et al[4], the body of the stomach was taped using a loop to maintain the exposure of the pancreas. In the technique of Chang et al[5], three Prolene straight needle stay sutures were placed superficial to the posterior gastric wall and were slung to the anterior abdominal wall to expose the pancreas. Several other retractors have been described in the literature, such as Endograb™ (Virtual Ports, Misgav, Israel) and a magnetic anchoring and guidance system[17,18]. In our experience, suture retractions are simple and easy and are most frequently used in LESS. There is a problem with the release of suture retractors, i.e., there must be suitable space to pass through the tissue using a straight needle. In the pancreatectomy procedure, suture retractors are very difficult to release because of the limited operative field. The fish hook retractor is a refinement of the suture retractor, and can be released in a narrow space. In our technique, the pancreatic capsule is retracted toward the anterior abdominal wall to dissect the tunnel beneath the body of the pancreas. This cannot be achieved with straight needle stay sutures. Another advantage of the fish hook retractor is that the straight needle only passes through the abdominal wall once when releasing a retractor, compared to twice when releasing a suture retractor[19]. Unintentional injuries to other organs must be avoided during the procedure.
To our knowledge, this is the first surgical series of LESS-SPDP in pigs reported in the literature. Consistent with the sporadic case reports, we verified the critical technique involved in LESS-SPDP, reestablishing operative triangulation and generating a favorable operative field. It is a safe and feasible procedure and can be implemented in humans in selected cases at qualified surgical centers.
We thank Nakesh Bhatoolaul, a medical student at Southeast University, for his help improving the English of the manuscript. We also thank KangBo Co. Ltd. China for the development of the C-LMOD.
Laparoendoscopic single-site surgery (LESS) is an emerging technique that has been suggested as a promising alternative to conventional laparoscopic surgery for the management of many common diseases. The potential advantages of LESS are its comparable safety, improved cosmetic results, decreased complications, reduced postoperative pain and shorter postoperative stay. Given the complexity of this novel technique, LESS is performed mostly in common procedures, such as appendectomy and cholecystectomy.
For complicated surgery, dedicated instruments and advanced skills are necessary to compensate for the shortcomings of LESS. In the area of LESS, the research hotspot is to design and develop multichannel access cannula platform, intraoperative retractions and functional integration of commonly used instruments.
The curved laparoscopic multifunctional operative device (C-LMOD) can evacuate smoke quickly to maintain clear laparoscopic vision, while the electrocautery is in use. Although articulating graspers could perform some retraction, a suitable operative field should be provided by another device at a more favorable angle. The fish hook retractor is a refinement of the suture retractor, and can be released in a narrow space. Another advantage of the fish hook retractor is that the straight needle only passes through the abdominal wall once when releasing a retractor, compared to twice when releasing a suture retractor.
Using the novel flexible multichannel port, C-LMOD and fish hook retractors, surgeons can obtain a favorable operative field, and can try some complicated operations.
LESS is a positive development in the field of minimally invasive surgery, requiring only one incision that is disguised within the umbilical folds, which is in contrast to the, at least three, necessary incisions for conventional laparoscopic surgery. Articulating instruments: The articulating design of the instruments is a revolutionary development for LESS, enabling surgeons to obtain the best angle for retraction and dissection. The two articulating instruments in both hands must be crossed over at the fulcrum, with the instrument in the right hand operating at the left side and vice versa, conflicting with the existing operating rules.
This is a well written manuscript presenting a technique for single-port distal pancreatectomy. Clearly, single-port surgery of the pancreas is in an experimental phase, and careful assessment is mandatory before its application in humans.
P- Reviewers: Casadesus D, Nentwich MF S- Editor: Zhai HH L- Editor: Wang TQ E- Editor: Ma S
| 1. | Phillips MS, Marks JM, Roberts K, Tacchino R, Onders R, DeNoto G, Rivas H, Islam A, Soper N, Gecelter G. Intermediate results of a prospective randomized controlled trial of traditional four-port laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy. Surg Endosc. 2012;26:1296-1303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 123] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 2. | Lee SW, Milsom JW, Nash GM. Single-incision versus multiport laparoscopic right and hand-assisted left colectomy: a case-matched comparison. Dis Colon Rectum. 2011;54:1355-1361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Barbaros U, Sümer A, Demirel T, Karakullukçu N, Batman B, Içscan Y, Sarıçam G, Serin K, Loh WL, Dinççağ A. Single incision laparoscopic pancreas resection for pancreatic metastasis of renal cell carcinoma. JSLS. 2010;14:566-570. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Kuroki T, Adachi T, Okamoto T, Kanematsu T. Single-incision laparoscopic distal pancreatectomy. Hepatogastroenterology. 2011;58:1022-1024. [PubMed] |
| 5. | Chang SK, Lomanto D, Mayasari M. Single-port laparoscopic spleen preserving distal pancreatectomy. Minim Invasive Surg. 2012;2012:197429. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Misawa T, Ito R, Futagawa Y, Fujiwara Y, Kitamura H, Tsutsui N, Shiba H, Wakiyama S, Ishida Y, Yanaga K. Single-incision laparoscopic distal pancreatectomy with or without splenic preservation: how we do it. Asian J Endosc Surg. 2012;5:195-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Ji ZL, Peng SY, Cai XJ. A Laparoscopic Multifunctional Operative Device in Laparoscopic Hepatectomy. Chir Gastroenterol. 2004;20:308-312. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Gunderson CC, Knight J, Ybanez-Morano J, Ritter C, Escobar PF, Ibeanu O, Grumbine FC, Bedaiwy MA, Hurd WW, Fader AN. The risk of umbilical hernia and other complications with laparoendoscopic single-site surgery. J Minim Invasive Gynecol. 2012;19:40-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Wang D, Wang Y, Ji ZL. Laparoendoscopic single-site cholecystectomy versus conventional laparoscopic cholecystectomy: a systematic review of randomized controlled trials. ANZ J Surg. 2012;82:303-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Pfluke JM, Parker M, Stauffer JA, Paetau AA, Bowers SP, Asbun HJ, Smith CD. Laparoscopic surgery performed through a single incision: a systematic review of the current literature. J Am Coll Surg. 2011;212:113-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Romanelli JR, Earle DB. Single-port laparoscopic surgery: an overview. Surg Endosc. 2009;23:1419-1427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 248] [Article Influence: 15.5] [Reference Citation Analysis (2)] |
| 12. | Ahmed I, Paraskeva P. A clinical review of single-incision laparoscopic surgery. Surgeon. 2011;9:341-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 13. | Brown-Clerk B, de Laveaga AE, LaGrange CA, Wirth LM, Lowndes BR, Hallbeck MS. Laparoendoscopic single-site (LESS) surgery versus conventional laparoscopic surgery: comparison of surgical port performance in a surgical simulator with novices. Surg Endosc. 2011;25:2210-2218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Kanehira E, Siozawa K, Kamei A, Tanida T. Development of a novel multichannel port (x-Gate(®)) for reduced port surgery and its initial clinical results. Minim Invasive Ther Allied Technol. 2012;21:26-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Santos BF, Reif TJ, Soper NJ, Hungness ES. Effect of training and instrument type on performance in single-incision laparoscopy: results of a randomized comparison using a surgical simulator. Surg Endosc. 2011;25:3798-3804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Philipp SR, Miedema BW, Thaler K. Single-incision laparoscopic cholecystectomy using conventional instruments: early experience in comparison with the gold standard. J Am Coll Surg. 2009;209:632-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 111] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 17. | Schlager A, Khalaileh A, Shussman N, Elazary R, Keidar A, Pikarsky AJ, Ben-Shushan A, Shibolet O, Horgan S, Talamini M. Providing more through less: current methods of retraction in SIMIS and NOTES cholecystectomy. Surg Endosc. 2010;24:1542-1546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Joseph RA, Salas NA, Donovan MA, Reardon PR, Bass BL, Dunkin BJ. Single-site laparoscopic (SSL) cholecystectomy in human cadavers using a novel percutaneous instrument platform and a magnetic anchoring and guidance system (MAGS): reestablishing the “critical view”. Surg Endosc. 2012;26:149-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |