Published online Apr 21, 2014. doi: 10.3748/wjg.v20.i15.4457
Revised: September 6, 2013
Accepted: September 15, 2013
Published online: April 21, 2014
Processing time: 316 Days and 14.3 Hours
Transmural migrated retained sponges usually impact at the level of the ileo-cecal valve leading to a small bowel obstruction. Once passed through the ileo-cecal valve, a retained sponge can be propelled forward by peristaltic activity and eliminated with feces. We report the case of a 52-year-old female with a past surgical history and recurrent episodes of abdominal pain and constipation. On physical examination, a generalized resistance was observed with tenderness in the right flank. Contrast-enhanced multi-detector computed tomography findings were consistent with a perforated right colonic diverticulitis with several out-pouchings at the level of the ascending colon and evidence of free air in the right parieto-colic gutter along with an air-fluid collection within the mesentery. In addition, a ring-shaped hyperdense intraluminal material was also noted. At surgery, the ascending colon appeared irregularly thickened and folded with a focal wall interruption and a peri-visceral abscess at the level of the hepatic flexure, but no diverticula were found. A right hemi-colectomy was performed and on dissection of the surgical specimen a retained laparotomy sponge was found in the bowel lumen.
Core tip: Transmural migrated retained sponges usually impact at the level of the ileo-cecal valve leading to a small bowel obstruction. We report the case of a 52-year-old female with a past surgical history and recurrent episodes of abdominal pain. Contrast-enhanced multi-detector computed tomography findings were consistent with a perforated right colonic diverticulitis with additional evidence of hyperdense intra-luminal material. At surgery, a right hemi-colectomy was performed and on dissection of the surgical specimen a retained laparotomy sponge was found in the bowel lumen.
- Citation: Camera L, Sagnelli M, Guadagno P, Mainenti PP, Marra T, Scotto di Santolo M, Fei L, Salvatore M. Colonic perforation by a transmural and transvalvular migrated retained sponge: Multi-detector computed tomography findings. World J Gastroenterol 2014; 20(15): 4457-4461
- URL: https://www.wjgnet.com/1007-9327/full/v20/i15/4457.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i15.4457
Retained foreign bodies represent a relatively uncommon complication of abdominal or pelvic surgery with a reported incidence of 1 every 1000-1500 operations. However, the real frequency of retained foreign bodies may be higher because of underreporting due to medico-legal concerns[1].
The commonest retained foreign bodies are surgical sponges left behind during abdominal or pelvic surgery, mainly after emergency or gynaecological interventions[2]. Clinical manifestations of retained surgical sponges can be extremely variable and often non-specific with patients being either asymptomatic or complaining of recurrent and/or intermittent episodes of abdominal pain occurring from the immediate post-operative period to several years after surgery[3].
This is largely based on the type of reaction, fibrinous or exudative, induced by the retained sponge in the surrounding tissues. In the former, the retained sponge is also referred to as gossypiboma[2]. Imaging characteristics of gossypibomas have been well described on both abdominal plain film[4] and cross-sectional imaging[5,6].
More rarely, the retained sponge may migrate into the gut lumen as a result of an exudative reaction leading to a fistula within the bowel wall[7-9]. In this instance, the patient will manifest signs and symptoms of small bowel obstruction as the retained sponge impacts at the level of the ileo-cecal valve[10].
Herein, we report a case of a 52-year old woman with multi-detector computed tomography (CT) findings consistent with a perforated right colonic diverticulitis who was found at surgery to have a retained sponge migrated into both the ascending and proximal transverse colon through the ileo-cecal valve.
A 52-year-old female was admitted to our hospital with a 5-d history of abdominal pain and constipation with tenderness in the right flank.
Her past medical history included a hysterectomy performed 5 years before for uterine fibromatosis with several episodes of intermittent abdominal pain and alternate alvus thereafter. Abdominal ultrasonography showed a concentric wall thickening at the level of both the terminal ileum and the ascending colon. Based on these clinical and instrumental findings, a presumed diagnosis of inflammatory bowel disease was formulated and the patient received treatment with mesalazine (500 mg × 3/d). An abdominal magnetic resonance imaging (MRI) scan was also performed and no remarkable findings were noted.
On physical examination, a pale abdomen was observed with a generalized resistance, more evident in the right flank, with no rebound. Laboratory tests were unremarkable except for mild leucocytosis (WBC 15.8 × 103/mL) and increased levels (17.2 mg/dL; n.v. < 1.0 mg/dL) of C-reactive protein. At this time, a contrast-enhanced CT scan was performed after oral administration of 1 L of 2% diluted Diatrizoate-Dimeglumine (Gastrografin, Bayer, Berlin, Germany).
Multi-detector row CT (Aquilion 64, Toshiba, Japan) was performed using a detector configuration of 2 mm × 16 mm, section thickness 5 mm, table speed of 36 mm/s and a gantry rotation time of 0.75 (pitch factor = 0.844), 120 kVp and automatic dose modulation. A mono-phasic caudo-cranial acquisition was performed 80 s. after iv bolus injection of 150 mL of non-ionic iodinated contrast medium (Ultravist 370; Bayer, Berlin, Germany) at a rate of 2 mL/s.
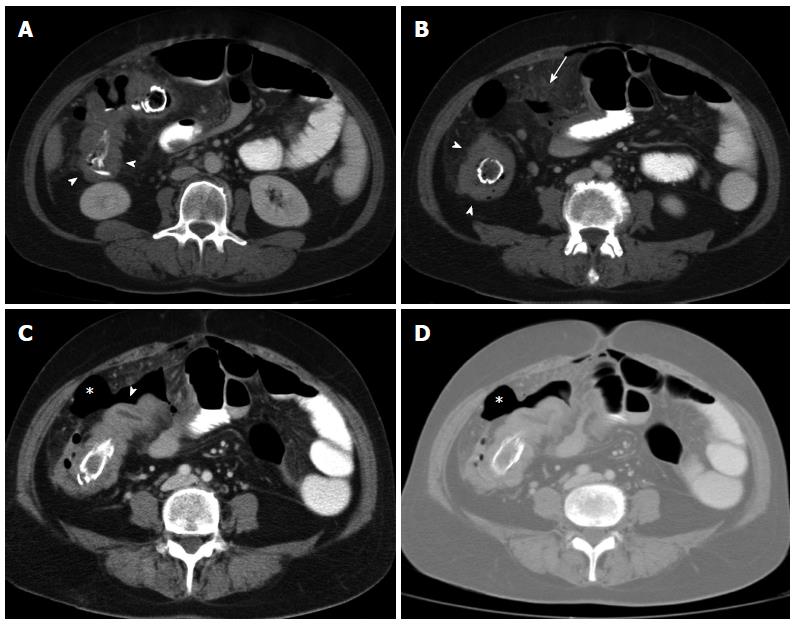
On contrast-enhanced CT, concentric wall thickening was seen at the level of both the ascending and proximal transverse colon with several out-pouchings consistent with colonic diverticula (Figure 1A) and associated hyperplasic ileo-colic lymph nodes (Figure 1B). A small air-fluid collection was also observed within the mesentery with associated fat-stranding (Figure 1B). Extra-luminal air was also evident at a more caudal level (Figure 1C) as best shown on the pulmonary window setting (Figure 1D). CT findings were considered to be consistent with a perforated right colonic diverticulitis. However, a ring-shaped hyperdense intra-luminal material was also noted in both the ascending colon and the proximal transverse colon (Figure 1A-D).
The patient underwent urgent laparotomy. At surgery, there was free air discharge on opening the peritoneum with evidence of multiple adhesions between the terminal ileum, the adjacent small bowel loops and the right colon. The latter appeared irregularly thickened and folded with evidence of a focal wall interruption and a peri-visceral abscess at the level of the hepatic flexure. A right hemi-colectomy was performed and on dissection of the surgical specimen a retained laparotomy sponge was found within the bowel lumen (Figure 2).
Retrospective Maximum Intensity Projection reconstructed images clearly showed the transmural and transvalvular migrated sponge extending from the ileo-cecal valve to the proximal transverse colon (Figure 3).
The post-operative period was uneventful and the patient was discharged the following week.
Surgical sponges are the commonest foreign bodies left behind after abdominal or pelvic operations. However, while a retained sponge certainly represents an unusual complication, its reported incidence is underestimated due to medico-legal concerns[1].
As the cotton matrix is inert, the fate of a retained surgical sponge is largely dependent on the type of reaction induced by the foreign material in the surrounding tissues[3]. The first type is an aseptic fibrinous reaction which generates adhesions and encapsulation of the cotton matrix. This usually results in a foreign body granuloma often referred to as gossypiboma, from the Latin word Gossypium, meaning cotton, and the Swahili word boma, meaning place of concealment[6]. This type of reaction is the most common and often clinically asymptomatic. As a result, gossypibomas are usually incidentally detected on both abdominal plain films as well as cross-sectional imaging and exhibit characteristic features[4-6].
More rarely, a surgical sponge may induce an exudative reaction leading to a phlegmon or abscess formation resulting in the erosion and perforation of a hollow viscus followed by migration of the foreign body into the gut lumen[7]. This process can take several years in which the patient most often manifests unspecific symptoms such as intermittent abdominal pain, weight loss, nausea, anorexia and even mild fever[7-9].
Most commonly, the sponge migrates into the small bowel lumen where it is pushed forward by peristaltic activity and, as long as it does not encounter adhesions or strictures, it reaches the ileo-cecal valve where it usually becomes impacted leading to a small bowel obstruction[10]. Once the sponge passes through the ileo-cecal valve it can be propelled forward and eliminated with feces[11]. To the best of our knowledge, there is no reported case in which a transmural and transvalvular migrated surgical sponge manifested clinically with a colonic perforation.
Our patient had long been complaining of recurrent episodes of abdominal pain which had been erroneously thought to be consistent with an inflammatory bowel disease. As we do not have any explanation as to how such a diagnosis could only be based on clinical and ultrasonographic findings, the patient was under treatment with mesalazine (500 mg × 3/d) and underwent an abdominal MRI scan 3 mo prior to admission at our Institution. As the MRI report did not mention any pathological signal alteration within the peritoneal cavity, we can reasonably assume that the perforation found at surgery was recent.
As far as the missed MRI diagnosis of an intra-luminal foreign body is concerned, it is well known that retained surgical sponges can be difficult to detect on MR images due to the diamagnetic properties of the radiopaque filaments and the very few free protons contained in the cotton matrix[12]. In our case, we can reasonably argue that the surgical sponge was likely mistaken for normal fecal content given its intraluminal localization, whereas an intra-abdominal gossypiboma may appear as a well-defined mass of mixed signal intensities on MR images[13].
Surgical findings accounted for the concentric wall thickening observed at the level of both the ascending and proximal transverse colon (Figure 1A) as well as the fluid collection and the nearby fat stranding depicted within the mesentery (Figure 1B). At surgery, however, no diverticula were found. Following dissection of the surgical specimen (Figure 2), it was assumed that the retained sponge eroded the colonic wall from the inside. As it is unknown why the perforation occurred at the level of the proximal transverse rather than the ascending colon, it can be argued that it involved the more distal portion of the retained intraluminal sponge because it had been lying there for a longer period of time.
As far as the oral administration of water-soluble iodinated contrast medium is concerned, this is still a controversial practice in the clinical setting of an adhesive small bowel obstruction. As the patient had a past surgical history with recurrent episodes of abdominal pain and constipation, it was wrongly assumed to be an adhesive small bowel obstruction by the on-call radiologist. Indeed, a recent meta-analysis showed a beneficial effect of orally administered Gastrografin in terms of both reducing the need for surgery and shortening hospital stay for patients with adhesive small bowel obstruction[14].
However, in the present case, the presence of intraluminal contrast agent did not affect the correct interpretation of CT images as it did not reach the ileo-cecal valve as shown by the coronal Maximum Intensity Projection (MIP) reconstructed image (Figure 3).
As the latter was not obtained in the prospective image analysis, the present case underscores the added diagnostic value of the coronal reformatted or reconstructed multidetector CT (MDCT) images in the setting of acute abdomen[15]. If it had been generated prospectively, the coronal MIP image (Figure 3) would have pointed to the correct diagnosis of an iatrogenic perforation as assessed by laparotomy (Figure 2).
We report the case of a transmural and transvalvular migration of a retained surgical sponge which manifested with a colonic perforation.
To the best of our knowledge, no such cases have been reported in the literature.
P- Reviewers: KeeseM, Sun ZH S- Editor: Qi Y L- Editor: Webster JR E- Editor: Wang CH
| 1. | Lincourt AE, Harrell A, Cristiano J, Sechrist C, Kercher K, Heniford BT. Retained foreign bodies after surgery. J Surg Res. 2007;138:170-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 167] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 2. | McIntyre LK, Jurkovich GJ, Gunn ML, Maier RV. Gossypiboma: tales of lost sponges and lessons learned. Arch Surg. 2010;145:770-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Kaiser CW, Friedman S, Spurling KP, Slowick T, Kaiser HA. The retained surgical sponge. Ann Surg. 1996;224:79-84. [PubMed] |
| 4. | O’Connor AR, Coakley FV, Meng MV, Eberhardt SC. Imaging of retained surgical sponges in the abdomen and pelvis. AJR Am J Roentgenol. 2003;180:481-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 86] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Kalovidouris A, Kehagias D, Moulopoulos L, Gouliamos A, Pentea S, Vlahos L. Abdominal retained surgical sponges: CT appearance. Eur Radiol. 1999;9:1407-1410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Manzella A, Filho PB, Albuquerque E, Farias F, Kaercher J. Imaging of gossypibomas: pictorial review. AJR Am J Roentgenol. 2009;193:S94-S101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 94] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 7. | Düx M, Ganten M, Lubienski A, Grenacher L. Retained surgical sponge with migration into the duodenum and persistent duodenal fistula. Eur Radiol. 2002;12 Suppl 3:S74-S77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 44] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Dhillon JS, Park A. Transmural migration of a retained laparotomy sponge. Am Surg. 2002;68:603-605. [PubMed] |
| 9. | Godara R, Marwah S, Karwasra RK, Goel R, Sen J, Singh R. Spontaneous transmural migration of surgical sponges. Asian J Surg. 2006;29:44-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Tandon A, Bhargava SK, Gupta A, Bhatt S. Spontaneous transmural migration of retained surgical textile into both small and large bowel: a rare cause of intestinal obstruction. Br J Radiol. 2009;82:e72-e75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Alis H, Soylu A, Dolay K, Kalayci M, Ciltas A. Surgical intervention may not always be required in gossypiboma with intraluminal migration. World J Gastroenterol. 2007;13:6605-6607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in CrossRef: 19] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Kim HS, Chung TS, Suh SH, Kim SY. MR imaging findings of paravertebral gossypiboma. AJNR Am J Neuroradiol. 2007;28:709-713. [PubMed] |
| 13. | Kim CK, Park BK, Ha H. Gossypiboma in abdomen and pelvis: MRI findings in four patients. AJR Am J Roentgenol. 2007;189:814-817. [PubMed] |
| 14. | Branco BC, Barmparas G, Schnüriger B, Inaba K, Chan LS, Demetriades D. Systematic review and meta-analysis of the diagnostic and therapeutic role of water-soluble contrast agent in adhesive small bowel obstruction. Br J Surg. 2010;97:470-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 143] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 15. | Zangos S, Steenburg SD, Phillips KD, Kerl JM, Nguyen SA, Herzog C, Schoepf UJ, Vogl TJ, Costello P. Acute abdomen: Added diagnostic value of coronal reformations with 64-slice multidetector row computed tomography. Acad Radiol. 2007;14:19-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |