Published online Dec 15, 1996. doi: 10.3748/wjg.v2.i4.247
Revised: August 9, 1996
Accepted: August 27, 1996
Published online: December 15, 1996
- Citation: Zhu JF, Xu SX, Zhang XH, Shong LP, Shan LC. Laparoscopy guided combined treatment of advanced hepatic carcinoma. World J Gastroenterol 1996; 2(4): 247-248
- URL: https://www.wjgnet.com/1007-9327/full/v2/i4/247.htm
- DOI: https://dx.doi.org/10.3748/wjg.v2.i4.247
Laparoscopic surgery, owing to its advantages of minor trauma and rapid recovery, has been accepted by surgeons all over the world in a quite short time. The technique has been used in the field of hepatic surgery. Laparoscopic liver resection[1,2], liver cyst fenestration[3] and liver abscess drainage[4] have been performed in recent years. Here we report a case of unresectable liver cancer treated by laparoscopic technique which includes laparoscopic hepatic artery ligation, alcohol and interleukin (IL)-2 injection into the tumor and a drug delivery system (DDS) implant through an omental vein.
A 47-year-old woman was admitted with a 1-mo history of pain in the right upper quadrant of the abdomen in March 1996. She had neither fever nor jaundice. Physical examination showed good general condition, and no enlarged lymph nodes were palpable. The sclerae were anicteric and the heart and lungs were normal. The liver was palpable 3 cm below the hypochondrium and 8 cm below the xiphoid process. Computed tomography (CT) showed a 12 cm × 10 cm × 8 cm mass in the right hepatic lobe. The porta hepatis and inferior vena cava were pushed to the left. There was no carcinomatous embolus in the portal vein as determined by ultrasonography. Blood tests showed normal liver function and serum bilirubin level. The concentration of alpha-feto protein (AFP) was 27180 μg/mL. The diagnosis of primary hepatic carcinoma was made according to the above-mentioned data. Preoperative CT scan showed that the tumor was unresectable. It was determined that hepatic artery ligation, alcohol and IL-2 intratumor injection and a DDS implant through an omental vein would be performed laparoscopically.
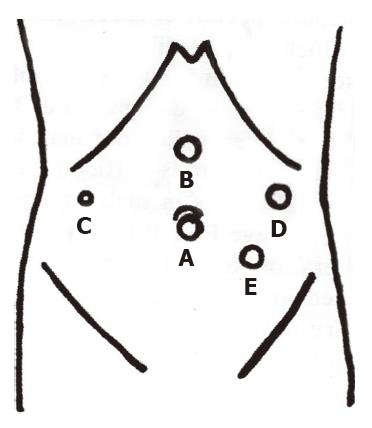
The operation was performed with the patient in the supine position, the surgeon standing on the left side of the patient and an assistant on either side. The videomonitor was set on the right. After induction of general anesthesia, pneumoperitoneum was created by umbilical puncture using a Veress needle, and intra-abdominal pressure was controlled at 14 mmHg. A straight 0° telescope attached to the videocamera (Karl Storz, Tuttlingen, Germany) was inserted through a 10-mm umbilical trocar (port A). Under the guidance of a laparoscope, four other cannulas were inserted. A 10-mm trocar (port B) inserted 5 cm below the xyphoid was used to provide an auxiliary operating channel for grasping instruments first and then be enlarged with an 18-mm trocar used to pull out the omentum for insertion of the DDS tube. A 5-mm cannula in the right hypochondrium (below the enlarged liver) was for the assistant′s grasping forceps for operating field exposure (Port C). Port D (10 mm) was used as the primary operating channel and port C for insertion of a 10-mm five-blade laparoscopic retractor (Figure 1).
After insertion of the trocars, the table was tilted 20° head-up. Laparoscopic inspection showed that the whole right lobe was occupied by the tumor; the liver was translocated to the left; and the porta hepatis was displaced to the left of the round ligament. An assistant grasped the funder of the gallbladder and turned the liver upward. The stomach and duodenum were pushed down with the five-blade retractor and the hepatoduodenal ligament was exposed. The hepatic artery pulsation could be seen clearly on the videomonitor. The serous coat of the hepatoduodenal ligament was opened up, the fat tissue was pushed away, and the proper hepatic artery was identified and ligated with two titanium clips. The color of the liver darkened after the blood stream was blocked. Percutaneous puncture of the liver tumor was performed with a long fine needle from several different points. Forty milliliters of absolute alcohol and one million unit of IL-2 were injected into the tumor. A rubber drainage tube was placed beside the porta hepatis which was delivered out of the abdominal cavity through port C. Port B was dilated with an 18-mm trocar and the greater omentum was pulled out. A larger omental vein was separated and the DDS tube was inserted into the vein about 20 cm long along the way of right gastroepiploic vein to the portal vein. The tube was fixed properly and the body of DDS was fixed near the port. Finally, the trocars were removed. The operation lasted three hours. The postoperative recovery was uneventful.
The most effective treatment for liver carcinoma is resection. The hepatic artery blocking is a choice of treatment for unresectable hepatic tumor at present. About 90%-95% of tumor blood supply comes from the hepatic artery. The blood stream in the normal part of the liver decreases by only 35%, while that in the tumor part declines by over 90% after the hepatic artery ligation. Thus, the tumor tissue necroses owing to ischemia. Intratumor alcohol injection is an effective approach to promoting the necrosis of tumor, therefore it can be an aspect of the combined treatment for liver cancer. The omental vein tube placement provides an approach to regional chemotherapy which makes high concentrations of antineoplastic agents accumulate in the tumor tissue, therefore the general toxic reactions can be diminished. Completing the above-mentioned operations under the guidance of a laparoscope is in accordance with the principle of treatment for advanced liver cancer. The indications of surgery are the same as those of open surgery, that is, no jaundice, ascites or cancerous embolus in the main portal vein so as to prevent irreversible postoperative hepatic failure.
Determining the positions of ports is the prerequisite for a successful operation. The basic principle is to place the ports below the edge of the enlarged liver except those for insertion of laparoscope and retractor. The main operating port can only be placed in the left hypochondrium because of obvious left translocation of porta hepatis. It is convenient to place port B on the midline, which can be dilated with an 18-mm trocar to pull out the greater omentum for the DDS tube placement into the omental vein, apart from being used as an auxiliary port. The omentum that has been pulled out may sometimes become contracture and pachynsis. It is difficult to find appropriate vessels to insert the DDS tube in such circumstances. Hence it may be essential to enlarge port B by a small incision.The key point for this operation is to free the hepatic artery which should be identified and operated carefully. The portal vein and bile duct injury must be avoided. It is quite important to prepare enough blood and get everything ready for open surgery. The tumor, due to its huge and fragile properties, is easy to bleed when injured. Under such circumstances, iatrogenic diffusion may occur. Therefore, great attention should be paid to avoiding injury to the tumor by trocars and instruments.
Laparoscopic surgery has been accepted widely owing to its advantages of less trauma and rapid recovery. It has special merits for patients with advanced liver cancer whose general resistance and tolerance to operative strike have been greatly decreased. We conclude that it is feasible to perform the combined operation guided by laparoscope in patients with unresectable liver cancer.
Original title:
S- Editor: A L- Editor: Wang TQ E- Editor: Li RF
| 1. | Eubanks S. The role of laparoscopy in diagnosis and treatment of primary or metastatic liver cancer. Semin Surg Oncol. 1994;10:404-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Schöb OM, Schlumpf RB, Uhlschmid GK, Rausis C, Spiess M, Largiadèr F. Experimental laparoscopic liver resection with a multimodal water jet dissector. Br J Surg. 1995;82:392-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Morino M, De Giuli M, Festa V, Garrone C. Laparoscopic management of symptomatic nonparasitic cysts of the liver. Indications and results. Ann Surg. 1994;219:157-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 109] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Yanaga K, Kitano S, Hashizume M, Ohta M, Matsumata T, Sugimachi K. Laparoscopic drainage of pyogenic liver abscess. Br J Surg. 1994;81:1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |