Published online Dec 15, 1996. doi: 10.3748/wjg.v2.i4.243
Revised: March 9, 1996
Accepted: March 20, 1996
Published online: December 15, 1996
AIM: To study the pathological changes in the pancreas of acute fulminant pancreatitis patients suffering from sudden death.
METHODS: Pancreatic duct specimens taken at autopsy from 30 patients with acute fulminant pancreatitis were examined under a light microscope for histopathological changes, with those of 30 other patients who died of other diseases as controls.
RESULTS: Among the 30 cases of acute fulminant pancreatitis, 29 (96.7%) were non-inflammatory including hemorrhagic necrotic type (2 cases) and one were inflammatory. The pathological findings showed that all the above types had pancreatic ductal changes, including the accumulation of shed ductal epithelial cells, eosinophilic materials in the ductal lumen and the presence of ductules in the wall of the pancreatic duct. In the control group, except for 1 case presenting ductules, there were no other changes observed.
CONCLUSION: Abnormal structural changes can cause damage to the ductal system of the pancreas, leading to an escape of activated proteolytic and lipolytic enzymes into the interstitial tissues and resulting in edema, ischemia, hemorrhage, necrosis and development of acute fulminant pancreatitis, which is an important cause of sudden death.
- Citation: Hu SX, Tang RJ, Zuo DY, Chen PH. Histopathological study of pancreatic duct in acute fulminant pancreatitis. World J Gastroenterol 1996; 2(4): 243-245
- URL: https://www.wjgnet.com/1007-9327/full/v2/i4/243.htm
- DOI: https://dx.doi.org/10.3748/wjg.v2.i4.243
There have been no uniform explanations for the causes of acute fulminant pancreatitis[1]. We have suggested that there must be certain relationship between the development of acute fulminant pancreatitis and structural abnormalities of the pancreatic duct[2]. For further observations of the abnormal structural characteristics of the pancreatic duct, a more detailed histopathological study was made on 30 cases of acute fulminant pancreatitis, so as to find out the pathological basis of sudden death in acute fulminant pancreatitis.
Specimens of pancreatic tissues from 30 patients were collected during the period of 1956-1987 by autopsy within 3-7 h after death. All the diagnoses were proved to be acute fulminant pancreatitis through autopsy, and their records were relatively complete. Specimens were taken from the head, body and tail of the pancreas, fixed in formalin solution and embedded in paraffin. Serial sections and HE staining were made for all; Foot Argyrol Fiber and van Gieson collagen staining for some. All the specimens were examined under a light microscope. Specimens of 30 other patients who died of diseases not involving the pancreas were taken as controls. The patients studied were 22 men and 8 women, ranging in age from 3 to 65 years (mean age: 30.2; 25 patients under 20). All the patients died within a few minutes to 24 h after the onset of symptoms, which occurred after playing cards, or watching performance or manual labour each in 3 cases; intake of a large amount of cold boiled water and a full meal each in 2 cases; ascariasis in the pancreatic duct, pregnancy, surgical operation, blood transfusion, drug injection, drinking wine, sexual intercourse, making speech in public and playing basket ball each in 1 case. No predisposing causes were found in 8 cases. Clinical symptoms included roaring in 5 cases, moaning, dyspnea and convulsion each in 4 cases, restlessness in 3 cases, sighing in 2 cases, coma in 1 case and records of symptoms not available in 8 cases. Twenty-five patients died during sleep at night, 2 patients died during a nap after lunch in the afternoon and 3 patients died suddenly at rest after manual labour.
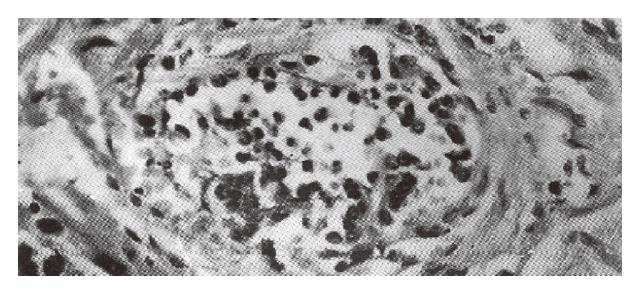
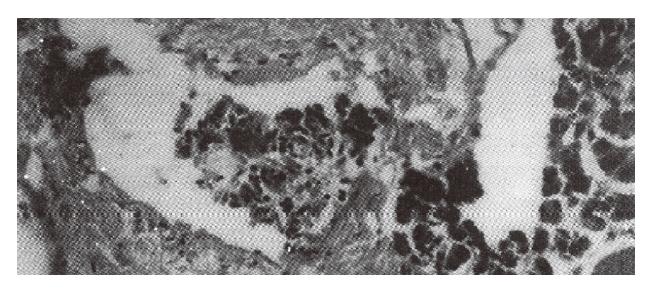
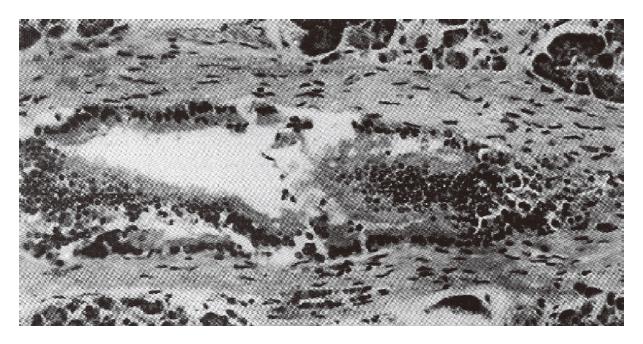
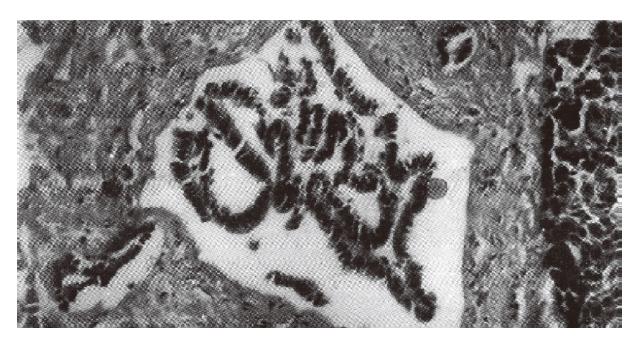
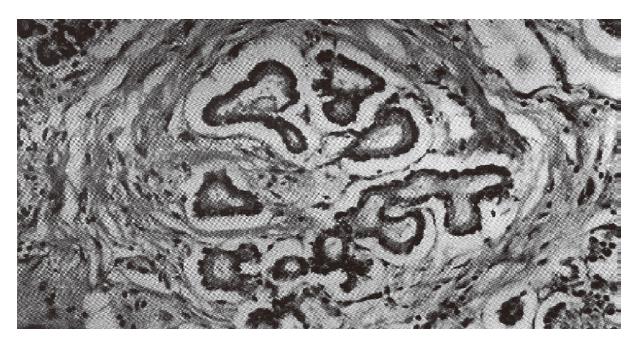
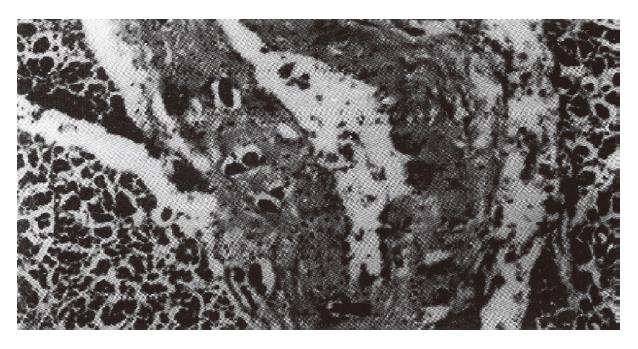
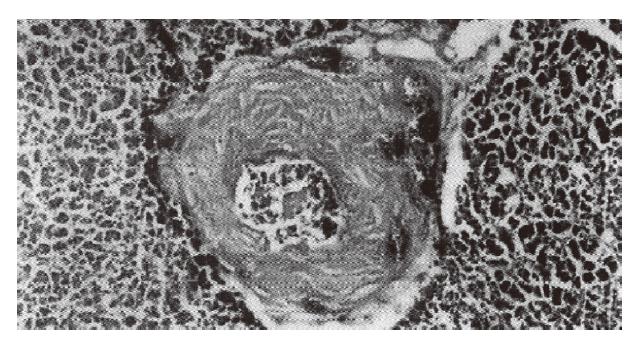
Among the 30 cases of acute fulminant pancreatitis, 29 (96.7%) were non-inflammatory. Of which, 23 (79.3%) belonged to hemorrhagic necrotic type (Figure 1), characterized by the accumulation of a large number of shed epithelial cells in the pancreatic duct lumina in all cases (Figure 2), a plenty of red blood cells in 9 cases (Figure 3), eosinophilic material in 6 cases (Figure 4), and eosinocytes in 4 cases (Figure 5), and the presence of necrosis of the pancreatic duct epithelium in the hemorrhagic areas, papillary proliferation or squamous epithelial metaplasia of the pancreatic duct epithelium in 17 cases (Figures 6 and 7). Pancreatic ductules in the wall of pancreatic ducts were present in 20 cases (Figures 8 and 9), with as many as 6 intramural ductules seen in 1 case (Figure 10). And hemorrhage occurred in the wall of pancreatic ducts in 12 cases (Figure 11). Four cases (13.8%) were of lipo-necrotic type with necrosis and shedding of the epithelial cells of the pancreatic ducts occurring in all the cases; eosinophilic material in the pancreatic duct lumina in 3 cases and pancreatic ductules in the wall of pancreatic ducts in 1 case. Two cases (6.9%) were of edematous type with eosinophilic material presenting in the pancreatic duct lumina in all and the shedding of epithelial cells in 1 case. Only 1 (3.3%) of the 30 cases belonged to the inflammatory type, which was of hemorrhagic necrotic type with the accumulation of eosinophilic material and inflammatory cells in the pancreatic duct lumina and the shedding of non-necrotic epithelial cells; infiltration of inflammatory cells was found in and around the wall of pancreatic ducts with ductules presenting in the wall of pancreatic ducts. In the control group, except for intramural ductules found in 3 cases, no other pathological changes were seen.
Our study showed that the histopathological changes in the pancreatic ducts in non-inflammatory and inflammatory pancreatitis of the same hemorrhagic necrotic type were essentially the same. As to non-inflammatory pancreatitis, changes in different types were markedly different, e.g., hemorrhagic necrotic type, lipo-necrotic type and edematous type. These findings are of considerable prophylactic and therapeutic significance for clinical practices.
There have been various theories about the etiology of acute fulminant pancreatitis in the literature[3-5], but most were based on experimental materials, only a few on autopsy data. The results of our study showed that there were characteristic lesions of the pancreatic duct in acute fulminant pancreatitis, and would provide a histopathological basis for interpretation of these theories. Specially worthy of notice is the presence of pancreatic ductules in the wall of pancreatic ducts as revealed in this study. Are they structural abnormalities or just normal branches of the pancreatic duct? We consider them as structural abnormalities, not normal branched pancreatic ducts, since (1) they were observed in cross sections, not in longitudinal sections; (2) in one cross section, 6 tubules may be seen at most; and (3) 22 (73.3%) of the 30 cases of acute fulminant pancreatitis developed intramural pancreatic ductules, whereas in the control group intramural ductules were only seen in 3 cases. The differences are statistically significant (P < 0.01). We conclude that the abnormal structural changes of the pancreatic duct as described above are important etiologic factors responsible for the damage to the ductal system of the pancreas, which makes the activated proteolytic enzymes escape into the interstitial tissues of the gland and results in the development of edema, ischemia, hemorrhage and necrosis of the pancreatic tissues. This may also bean important cause of sudden death in acute fulminant pancreatitis.
Original title:
S- Editor: Cao LB L- Editor: Wang TQ E- Editor: Li RF
| 1. | Huang ZQ, Gu ZY. Progress in hepatic, biliary and pancreatic surgery, 1sted. Beijing: Renmin Junyi Chubanshe 1989; 250-254. |
| 2. | Hu SX. Pathomorphological study of the pancreatic and extrapancreatic lesions in acute fulminant pancreatitis (in chin). Huanan Guofang Yixue Zazhi. 1980;3:5-7. |
| 3. | Beger HG. Surgical management of necrotizing pancreatitis. Surg Clin North Am. 1989;69:529-549. [PubMed] |
| 4. | Lack EE. The pancreas and extrahepatic biliary system. Principles and practice of surgical pathology, Vol 2, 2nd ed. New York: Churchill livingstone 1990; 1347-1396. |
| 5. | Bradley EL, Allen K. A prospective longitudinal study of observation versus surgical intervention in the management of necrotizing pancreatitis. Am J Surg. 1991;161:19-24; discussion 24-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 222] [Article Influence: 6.5] [Reference Citation Analysis (0)] |