Published online Sep 15, 1996. doi: 10.3748/wjg.v2.i3.149
Revised: July 10, 1996
Accepted: August 12, 1996
Published online: September 15, 1996
AIM: To report the first experience in China in the treatment of malignant biliary obstruction with expandable metal stent, which allows the insertion of an endoprosthesis as large as 1 cm in diameter.
METHODS: Between April 1994 and May 1996, we implanted expandable metal stents in 57 patients with incurable malignant biliary obstruction. Fifty-four patients underwent endoscopic procedure, and the other three patients received percutaneous transhepatic placement.
RESULTS: Insertion of the stent following guide wire positioning was successful in 95% of the patients. Two patients developed cholangitis after stent insertion and were successfully treated with conservative treatment. The jaundice was eliminated completely in 21 cases and markedly decreased in 23 cases within 2 wk after stent placement. However, nine patients had late cholangitis due to stent failure after a median interval of 147 d. Twenty-three cases underwent nasobiliary transient drainage, and three underwent plastic stent transient drainage prior to metal stent insertion. The advantages of transient drainage were drainage pre-assessment and infection control.
CONCLUSION: Our results show that an expandable metal stent is suitable for the unresectable malignant choledochal stenosis. It can eliminate jaundice and improve the patient’s quality of life. To get the highest benefit, however, the indication should be strictly selected. To get long-term patency, the proximal and distal end of the stent preceding the tumor should be no shorter than 2 cm. In the case of hilar cancer, Bismuth classification is helpful for the selection of the drainage site.
- Citation: Hu B, Zhou DY, Gong B, Zhang FM, Wang SZ, Chang HY, Wu MC. Metal stent implantation for palliation of malignant biliary obstruction: A report of 57 cases. World J Gastroenterol 1996; 2(3): 149-151
- URL: https://www.wjgnet.com/1007-9327/full/v2/i3/149.htm
- DOI: https://dx.doi.org/10.3748/wjg.v2.i3.149
Endoscopic biliary drainage with polyethylene endoprosthesis has become a well-established palliative treatment for patients with inoperable, malignant, and obstructive jaundice. The main drawback of this method is rapid incrustation or occlusion as a result of bacterial biofilm formation on the stent, and biliary sludge[1]. Drainage occlusion of the commonly used 7-12 Fr gauge plastic prosthesis occurs in 20% to 30% of cases within the first three mo and in up to 60% of cases within 6 mo[2]. Though larger stents may perform better, stents over 14 Fr have not been used in the biliary tract up to now because the maximum diameter of the stent depends upon the diameter of the working channel of the endoscope. The development of expandable metal stents allows the insertion of an endoprosthesis as large as 1 cm in diameter. Such an endoprosthesis, previously employed for vascular and urethral stricture, recently became available for biliary use.
In this paper, we report our first experience in China in the treatment of 57 patients with malignant bile duct stenosis using metal stents during the period from April 1994 to May 1996.
Fifty-seven patients (40 male and 17 female) with a median age of 56.1 years (range: 25 years to 85 years) were treated with a total of 60 expandable stents. In all patients, the malignant diseases led to invasive or compressive occlusion of the hepatocholedochal duct (Table 1). None were operable due to advanced stage, metastasis, post-operative recurrence of the disease, old age, or accompanying disease.
| Cause of bile duct obstruction | Location of stenosis | No. of patients | ||
| P | M | D | ||
| Cholangiocarcinoma | 30 | 3 | 1 | 34 |
| Gallbladder carcinoma | 3 | 1 | 0 | 4 |
| Hepatocellular carcinoma | 7 | 0 | 0 | 7 |
| Pancreatic carcinoma | 1 | 0 | 6 | 7 |
| Ampullary tumor | 0 | 0 | 2 | 2 |
| Metastasis | 3 | 0 | 0 | 3 |
| Total | 44 | 4 | 9 | 57 |
Two types (several kinds) of metal stents, self-expandable stents (Wallstent, Instent and Angiomed) and balloon-mounted stents (Strecker) were used.
General diagnostic endoscopic retrograde cholangiopancreato-graphy was first made using a side-view duodenoscope (TJF-30, 4.2 mm working channel, or JF-1T30, 3.2 mm working channel). When biliary stenosis was found, a 4 m long, 0.035 inch standard guide was inserted into papilla passing the strictured segment. No papillotomy was performed, but a simple dilation was made with a 10 Fr or 8.5 Fr Teflon dilator (Wilson-Cook) instead. Afterward, the delivery catheter with the constrained stent was inserted over the guide wire. The stent was released under continuous fluoroscopic and endoscopic control. If we were uncertain of the drainage effect in the patients with extensive stenosis or severe infection, a transient nasobiliary drainage was performed first. After a satisfactory drainage was achieved, or the bile duct inflammation was successfully controlled, another endoscopic procedure for the metal stent implantation was given.
In three patients, endoscopic transpapillary implantation was impossible because of previous Billroth II gastrectomy, cannulation failure of the ampulla of Vater, or duodenal stricture. Percutaneous transhepatic route was therefore chosen. One week after an ordinary percutaneous transhepatic biliary drainage (PTBD), the drainage tract was dilated to 10 Fr. A passage through biliary stenosis was made using a guide wire, and then the metallic stent was delivered into the biliary tree and released under fluoroscopy.
All patients were followed up as long as possible. Their general condition, laboratory findings, as well as recurrence of jaundice and fever were recorded.
Fifty-seven patients were implanted with a total of 60 metal stents. The success rate for metal endoprosthesis insertion was 95%. In three cases, there were technical problems during implantation of the first stent. In one of the patients, a Strecker stent failed to cannulate into papilla because its distal end had already been released. In another patient, a Wallstent could not be placed due to the breakage of its outer membrane. In the final patient, a Wallstent was released by mistake inside the working channel of the duodenoscope. However, in all three cases, another stent was successfully implanted the second time.
A transient rise in cholestasis parameters and fever indicating cholangitis as an early complication were seen in two (3.5%) patients. They were rapidly and effectively treated with antibiotics. No other complications related to stent insertion were found.
During the first two weeks after the placement of the stent, cholestasis parameters returned to normal in 21 cases, decreased significantly in 23 cases, and were unchanged or even elevated in two cases. Follow-up was unavailable for the remaining nine patients. However, during the long-term follow-up, nine patients had late cholangitis due to stent failure after a median interval of 146.7 d. The causes of stent failure were distal tumor overgrowth in four patients after a median interval of 127.5 d, tumor ingrowth through the meshes of the stent in four cases after a median of 150 d, and biliary sludge obstruction in one case after 210 d. The cholangitis was treated with a 9 Fr polyethylene stent through the metal stent in four patients, with a nasobiliary drainage in one patient, PTBD in one patient, and biliary lavage and balloon pull-through in one patient.
During the follow-up, four patients died due to non-stent related causes (renal failure in two cases 12 d and 210 d, respectively post stent insertion, esophageal variceal bleeding in one patient at 51 d post stent insertion, and ileus bleeding in one patient at 63 d post stent insertion). Two patients died of stent failure and cholangitis 90 d and 153 d after endoprosthesis, respectively. To our knowledge, eight patients with a successful stent insertion have been alive for more than 6 mo after stent implantation. The patient with the longest survival (over 18 mo) has been free from jaundice as of this publication.
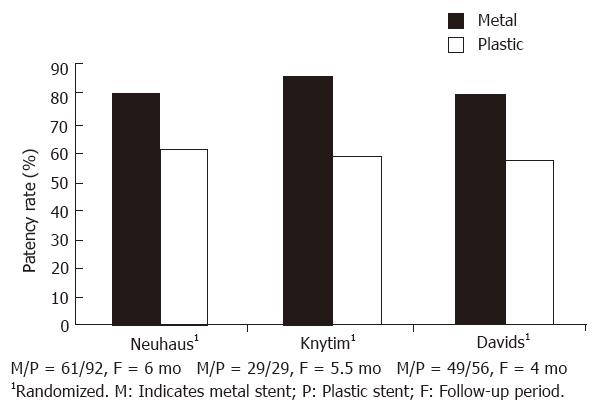
Expandable intraluminal stents were initially developed to prevent early reocclusion or delayed restenosis after percutaneous transluminal coronary angioplasty (PTCA). The first biliary expandable stent was inserted in an animal study in 1985[3]. The expandable diameters of the metal stents of up to 7-10 mm, the reduced surface area for bacterial attachment, and the capacity of being epithelialized by biliary mucosal cells are the major advantages in preventing bacterial colonization and biofilm formation. Figure 1 shows the results of current comparative or randomized studies by several specialists on wire mesh endoprostheses versus conventional plastic prostheses[4-6]. Hoepffner et al[2] reported a long term study on Wallstent therapy for 118 malignant choledochal stenosis patients, and found the survival rate at 6 mo, 12 mo, and 24 mo was 40%, 20% and 10% respectively, with the longest survival of 1295 d, which was similar to that after palliation bypass surgery in a previous report.
There were 44 (77.2%) patients with malignant biliary obstruction due to proximal bile duct stenosis in our study. It is attributable to the high incidence of hilar tumor (Klatskin’s tumor) and extraordinarily low resection rates of the cancer. According to the Bismuth classification[7], our patients were classified into type I (8 cases, 18.2%), type II (3 cases, 6.8%), type IIIa (5 cases, 11.4%), type IIIb (4 cases, 9.1%) and type IV (24 cases, 54.5%). The relationship between the typing and drainage sites is shown in Table 2. Generally, type I patients can get satisfactory drainage, followed by type II and type III. Type IV patients can only achieve poor drainage. We emphasize the importance of total revelation of intrahepatic duct, upon which it is possible to select a suitable site for drainage. Normally, the wider the range of the intrahepatic tree, the better the drainage. If the drained region can reach a little more than half a liver, it is still hopeful to eliminate jaundice completely. Sharp angles should be avoided when selecting a drainage site in order to get full expansion of the stent.
| Type | No. of patients | Drainage site | ||||
| H | L | R | RA | RP | ||
| I | 8 | 2 | 3 | 2 | 0 | 1 |
| II | 3 | 0 | 1 | 1 | 0 | 1 |
| IIIa | 5 | 0 | 2 | 0 | 1 | 2 |
| IIIb | 4 | 0 | 0 | 0 | 0 | 4 |
| IV | 24 | 0 | 6 | 2 | 4 | 12 |
| Total | 44 | 2 | 12 | 5 | 5 | 20 |
The length of the stent should also be determined carefully. In our group, there were four patients with late stent failure due to tumor overgrowth after a median interval of 127.5 d. Therefore, we recommend that the two ends of the stent preceding the tumor should not be shorter than 2 cm after full expansion in order to get long-term stenting.
We also attach importance to the use of transient nasobiliary drainage prior to the stenting. Because the metal stent is very expensive, we should be more prudent in choosing cases. Nasobiliary drainage is a simple and cheap way to know the quantity of the drain, and is very effective in controlling bile duct infection. It also gives the surgeon time to discuss if the patient has any opportunity to undergo a radical operation. In our group, 23 patients had undergone nasobiliary drainage, and three patients had undergone plastic stent drainage for a mean period of 15 d before metal endoprosthesis insertion. When the bile fluid was less than 300 mL per day and the cholestasis parameters decreased significantly, another endoscopic procedure for metal stent implantation can be performed.
Though expandable metal stents provide a longer median period of patency over conventional plastic prosthesis, they are not without problems. Tumor ingrowth through the metal mesh, or overgrowth at the ends of the stents may occur several weeks to several mo later, causing occlusion of bile flow (Table 3). Many stent occlusions can be successfully treated by implantation of a second metal stent or a conventional plastic one through the metal stent. Some endoscopists also reported the method of coagulation using a unipolar electrohydral probe or bipolar electrohydrothermal probe[2,8]. In recent studies, a “coating” stent or “electrolytic” stent may solve the above-mentioned disadvantages of metal stents[10,11].
| Huibregtse et al, 1992 (103 cases) | Hoepffner et al, 1994 (118 cases) | Our group, 1996 (57 cases) | |
| Early cholangitis | 2 | 5 | 2 |
| Late cholangitis | 18 (125 d)1 | 17 (148 d) | 9 (147 d) |
| Tumor ingrowth | 10 | 4 (150 d) | 4 (150 d) |
| Tumor overgrowth | 4 | 5 | 4 (128 d) |
| Sludge clogging | 5 (175 d) | N/A | 1 (210 d) |
The indications of metal stent implantation remain controversial. Though some doctors have tried to use metal stents to treat benign biliary stricture, most specialists are reluctant to use this unremovable stent in patients with benign disease because the recurrent ulceration caused by sharp filaments of the metal stent scan give rise to restricture proximal to the stent. The high cost of this treatment is also under discussion. Although several authors have argued that when the costs of retreatment due to plastic stent failure are included, the metal stents are cost-effective, considering the limited life span of these patients with terminal malignancies, the price of the metal stent is still a concern. “Is the expanse worth the expense?” is an interesting question raised by Cotton[12]. In our opinion, metal stent implantation is the treatment of choice for palliating jaundice in patients (1) with inoperable pancreatobiliary malignancies, (2) with adequate biliary tree to drainage, (3) without major organic exhausting, (4) who may survive for more than 3 mo, and (5) whose financial condition allows.
Reported at the International Workshop and Symposium on Therapeutic Endoscopy and Gastroenterology, Shenyang, 17th July, 1995
Original title:
S- Editor: Tao T L- Editor: Filipodia E- Editor: Li RF
| 1. | Sung JJ, Chung SC. Endoscopic stenting for palliation of malignant biliary obstruction. A review of progress in the last 15 years. Dig Dis Sci. 1995;40:1167-1173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Hoepffner N, Foerster EC, Högemann B, Domschke W. Long-term experience in Wallstent therapy for malignant choledochal stenosis. Endoscopy. 1994;26:597-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Carrasco CH, Wallace S, Charnsangavej C, Richli W, Wright KC, Fanning T, Gianturco C. Expandable biliary endoprosthesis: an experimental study. AJR Am J Roentgenol. 1985;145:1279-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 75] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Neuhaus H, Hagenmuller F, Classen M. Self expanding metal stents versus conventional plastic endoprostheses for malignant biliary obstruction. Gastrointest Endosc. 1991;37:253-260. |
| 5. | Knyrim K, Wagner HJ, Pausch J, Vakil N. A prospective, randomized, controlled trial of metal stents for malignant obstruction of the common bile duct. Endoscopy. 1993;25:207-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 382] [Cited by in RCA: 358] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 6. | Davids PH, Groen AK, Rauws EA, Tytgat GN, Huibregtse K. Randomised trial of self-expanding metal stents versus polyethylene stents for distal malignant biliary obstruction. Lancet. 1992;340:1488-1492. [PubMed] |
| 7. | Bismuth H, Castaing D, Traynor O. Resection or palliation: priority of surgery in the treatment of hilar cancer. World J Surg. 1988;12:39-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 237] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 8. | Dertinger S, Ell C, Fleig WE, Hochberger J, Kam M, Gurza L, et al. Long-term results using self-expanding metal stents for malignant biliary obstruction. Gastroenterology. 1992;102:310-311. |
| 9. | Huibregtse K, Carr-Locke DL, Cremer M, Domschke W, Fockens P, Foerster E, Hagenmüller F, Hatfield AR, Lefebvre JF, Liquory CL. Biliary stent occlusion--a problem solved with self-expanding metal stents? European Wallstent Study Group. Endoscopy. 1992;24:391-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 61] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Bosco JJ, Muggia RA, Howell DA, Jones M. Gianturco-Rosch metal Z-stent for endoscopic treatment of malignant extrahepatic biliary obstruction. Proceeding of World Congress of Gastroenterology. 1994;2512-2516. |
| 11. | Cwikiel W, Stridbeck H, Stenram U. Electrolytic stents to inhibit tumor growth. An experimental study in vitro and in rats. Acta Radiol. 1993;34:258-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Cotton PB. Metallic mesh stents--is the expanse worth the expense? Endoscopy. 1992;24:421-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |