Published online Dec 28, 2013. doi: 10.3748/wjg.v19.i48.9481
Revised: October 1, 2013
Accepted: December 13, 2013
Published online: December 28, 2013
Processing time: 152 Days and 21 Hours
There are many case reports on colon diverticula that cause irritable bowel syndrome, constipation, bleeding, diverticulitis, stricture due to multiple recurrences of diverticulitis, and perforation. However, few articles have examined neoplasms that arise from a diverticulum, such as adenoma and adenocarcinoma, and there have been no reports of granulation polyps that arise from a colon diverticulum after recurrent diverticulitis. We observed a rare granulation polyp that arose from a diverticulum as a result of repeated episodes of local diverticulitis. Narrow band imaging magnified colonoscopy was very useful to diagnose the polyp as a granulation polyp because of the absence of a pit pattern on the surface of the polyp. We successfully resected the polyp using endoscopic mucosal resection. We inverted the diverticulum, and the resected stalk of the polyp was used to close the diverticulum with an over-the-scope clip. If a granulomatous polyp could arise from a diverticulum, differential diagnosis between a colon neoplasm and a granulomatous polyp would not only be difficult but also necessary for suitable endoscopic treatment.
Core tip: The study observed a rare granulation polyp that arose from a diverticulum as a result of repeated episodes of local diverticulitis. The authors successfully resected the polyp using endoscopic mucosal resection. The diverticulum was inverted, and the resected stalk of the polyp was used to close the diverticulum with an over-the-scope clip.
- Citation: Mori H, Tsushimi T, Kobara H, Nishiyama N, Fujihara S, Matsunaga T, Ayagi M, Yachida T, Masaki T. Endoscopic management of a rare granulation polyp in a colonic diverticulum. World J Gastroenterol 2013; 19(48): 9481-9484
- URL: https://www.wjgnet.com/1007-9327/full/v19/i48/9481.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i48.9481
A colon diverticulum is caused by increased intra-colonic pressure or by a weakened colonic wall. Most colon diverticula consist of acquired pseudodiverticula and have been observed in the sigmoid colon of patients in Western countries and in the ascending colon of patients in Japan[1]. The most reliable method to identify colon diverticula is a barium enema; however, once a diverticulum begins to bleed, colonoscopy is a useful modality to treat the bleeding vessels[2,3]. Although the incidence of colonic diverticular bleeding is increasing, treatments have not yet been well established. The risk factors contributing to recurrent hemorrhage after initial improvement in colonic diverticular bleeding are past histories of hypertension or renal deficiency. Follow-up colonoscopy after the initial improvement in colonic diverticular bleeding is needed in patients with hypertension or renal deficiency[4]. In addition, local peritonitis due to diverticulitis, and perforation are serious complications[5]. Although 85% of patients with colonic diverticulitis will recover with non-surgical treatment, some patients may have complications such as abscesses, fistulas, obstruction and panperitonitis[6,7]. On the other hand, few articles have examined neoplasms that arise from the diverticulum, such as adenoma and adenocarcinoma[8].
We describe a rare case of a granulomatous polyp which arose from a colon diverticulum.
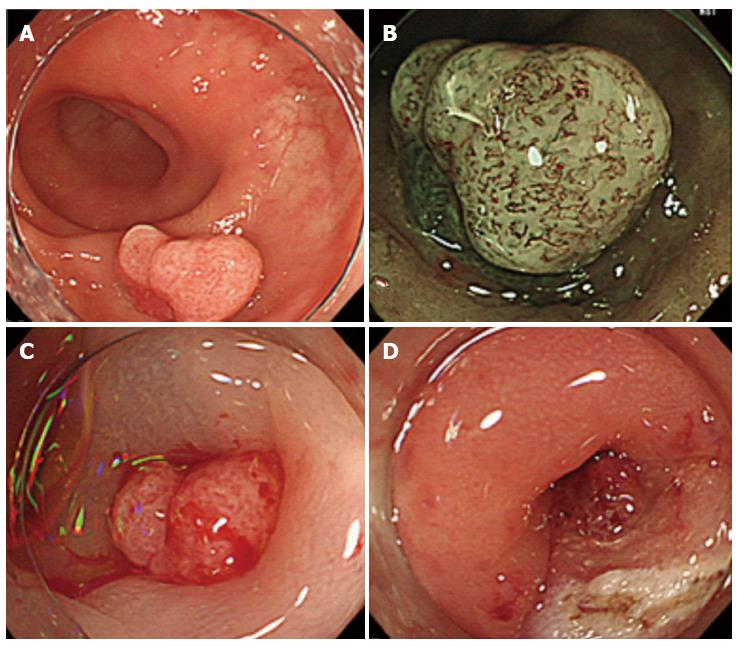
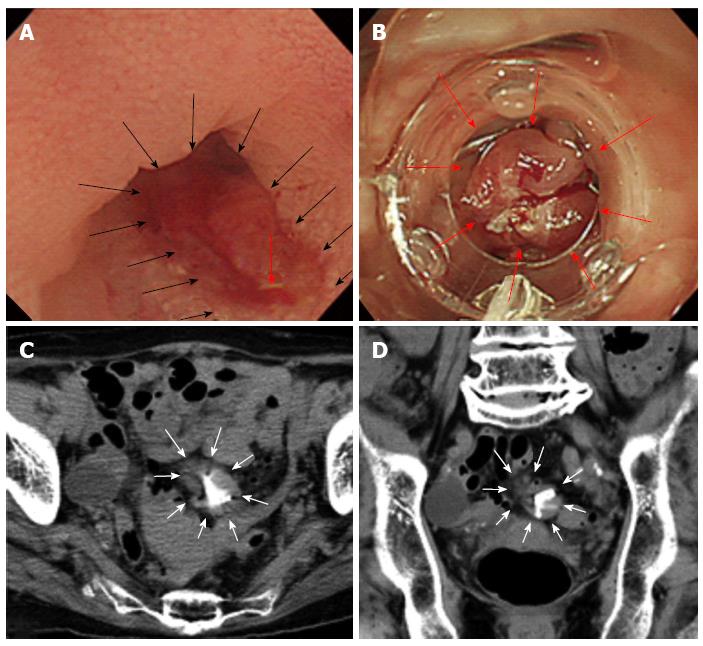
A 62-year-old woman who suffered from repeated left lower abdominal pain and high fever (38 °C) underwent a colonoscopy and was diagnosed with a sigmoid colon polyp that was approximately 25 mm in diameter (Figure 1A). Twice during the previous year, she had suffered from abdominal pain and a high fever, and her blood laboratory data were as follows: a white blood cell count of 12000/μL and a C-reactive protein level of 5.59 mg/mL. After undergoing colonoscopy, her symptoms disappeared. Additionally, narrow band imaging (NBI) magnified colonoscopy was performed to diagnose the polyp in greater detail. Several irregular microvessels were found on the surface of the polyp. However, the pit pattern which is usually observed in neoplasms, such as adenoma and adenocarcinoma, was absent from the surface of the polyp (Figure 1B). The surface was smooth, and we were unable to determine whether the polyp was a neoplasm or an inflammatory polyp. To confirm the qualitative histological diagnosis, we performed endoscopic mucosal resection (EMR) of the polyp. We obtained written informed consent from the patient to perform the EMR procedure for treatment of the polyp. During EMR, a local saline injection was administered, which slightly elevated the polyp (Figure 1C), and allowed resection of the polyp. After removing the polyp, we identified the diverticulum using the resected stalk of the polyp (Figure 1D). A closer view of the resected surface revealed that the cavity of the diverticulum was irregular, and exposed vessels were observed (Figure 2A). The resection of the polyp indicated that it arose from the diverticulum (Figure 2A). To prevent post-EMR bleeding and delayed perforation, we inverted the diverticulum and sutured the inverted diverticulum, including the resected stalk of the polyp, with an over-the-scope clip (OTSC) (Figure 2B). After the EMR procedure, computed tomography was performed to examine the soft tissue density around the OTSC and the increased fat density around the resected site (Figure 2C and D).
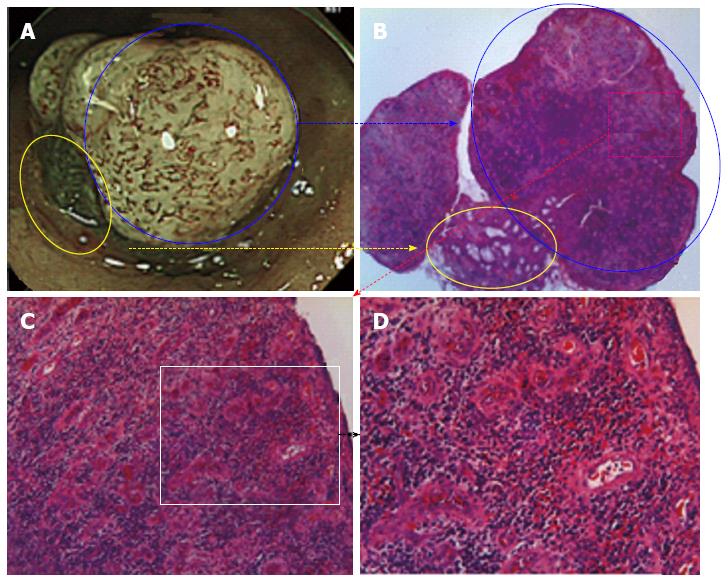
According to the clinical course of the patient, which included high fever and repeated left lower abdominal pain, we suspected that post-inflammation granulation tissue arose from the bottom of the diverticulum after repeated episodes of diverticulitis. Seven days after the procedure, the histology of the polyp revealed that it was composed only of granulation tissue with no neoplasm (Figure 3). The patient was discharged from our hospital without any complications.
We report the unique case of a granulomatous polyp that arose from a single diverticulum after repeated episodes of local diverticulitis. A colonic diverticulum causes some serious complications such as bleeding, stricture due to multiple recurrences of diverticulitis, and perforation[5-7]. Several case reports have also described neoplasms that arose from a single diverticulum, which was successfully treated with EMR and completely closed with the assistance of laparoscopy[8]. However, there have been no previous reports of granulomatous polyps that arose from a single diverticulum after repeated episodes of local diverticulitis, which was treated with EMR and closed with an OTSC. When polyps are diagnosed as neoplastic, magnifying chromoendoscopy and NBI magnifying image-enhanced endoscopy can be used to detect the pit pattern. A granulomatous polyp should be diagnosed when no pit pattern is observed because a pit pattern reveals the surface characteristics of a neoplasm[9]. The resection of a polyp arising from a diverticulum is associated with a risk of perforation or bleeding. A full-thickness resection using a pre-full thickness suture with an OTSC was reported to be the safest method to resect the full-thickness wall of the colon[10]. Similarly, after inverting the diverticulum and the polyp into the colon, a full-thickness suture using an OTSC and a full-thickness resection may be safely performed. In this case, we should have initially inverted the diverticulum and the polyp and safely resected the full-thickness of the colon wall after diagnosing the granulomatous polyp that arose from a diverticulum. When many granulomatous polyps arise from many diverticula and the neighboring granuloma fuses, a stricture of the colon may develop; therefore, a differential diagnosis between colon cancer and a granulomatous stricture would be difficult[11].
We would like to thank Professor Yasuyuki Suzuki for technical and editorial assistance.
P- Reviewers: Maltz C, Siriwardana HPP S- Editor: Qi Y L- Editor: Cant MR E- Editor: Wu HL
| 1. | Maconi G, Barbara G, Bosetti C, Cuomo R, Annibale B. Treatment of diverticular disease of the colon and prevention of acute diverticulitis: a systematic review. Dis Colon Rectum. 2011;54:1326-1338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Yoshida M, Kawabata K, Kutsumi H, Fujita T, Soga T, Nishimura K, Kawanami C, Kinoshita Y, Chiba T, Fujimoto S. Polypoid prolapsing mucosal folds associated with diverticular disease in the sigmoid colon: usefulness of colonoscopy and endoscopic ultrasonography for the diagnosis. Gastrointest Endosc. 1996;44:489-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Ishii N, Setoyama T, Deshpande GA, Omata F, Matsuda M, Suzuki S, Uemura M, Iizuka Y, Fukuda K, Suzuki K. Endoscopic band ligation for colonic diverticular hemorrhage. Gastrointest Endosc. 2012;75:382-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 91] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 4. | Setoyama T, Ishii N, Fujita Y. Enodoscopic band ligation (EBL) is superior to endoscopic clipping for the treatment of colonic diverticular hemorrhage. Surg Endosc. 2011;25:3574-3578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 60] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Paoluzi OA, Tosti C, Andrei F, Stroppa I, Pallone F. Look out before polypectomy in patients with diverticular disease--a case of a large, inverted diverticulum of the colon resembling a pedunculated polyp. Can J Gastroenterol. 2010;24:61-63. [PubMed] |
| 6. | D’Ovidio V, Di Camillo M, Pimpo MT, Meo D, Vernia P, Caprilli R. An unusual complicated polypectomy and inverted colonic diverticula. Colorectal Dis. 2010;12:491-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Hirata T, Kawakami Y, Kinjo N, Arakaki S, Arakaki T, Hokama A, Kinjo F, Fujita J. Association between colonic polyps and diverticular disease. World J Gastroenterol. 2008;14:2411-2413. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Fu KI, Hamahata Y, Tsujinaka Y. Early colon cancer within a diverticulum treated by magnifying chromoendoscopy and laparoscopy. World J Gastroenterol. 2010;16:1545-1547. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (4)] |
| 9. | Tanaka S, Sano Y. Aim to unify the narrow band imaging (NBI) magnifying classification for colorectal tumors: current status in Japan from a summary of the consensus symposium in the 79th Annual Meeting of the Japan Gastroenterological Endoscopy Society. Dig Endosc. 2011;23 Suppl 1:131-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 96] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 10. | Schurr MO, Baur F, Ho CN, Anhoeck G, Kratt T, Gottwald T. Endoluminal full-thickness resection of GI lesions: a new device and technique. Minim Invasive Ther Allied Technol. 2011;20:189-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Nishiyama N, Mori H, Kobara H, Rafiq K, Fujihara S, Kobayashi M, Masaki T. Difficulty in differentiating two cases of sigmoid stenosis by diverticulitis from cancer. World J Gastroenterol. 2012;18:3623-3626. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |