Published online Dec 7, 2013. doi: 10.3748/wjg.v19.i45.8449
Revised: October 18, 2013
Accepted: October 19, 2013
Published online: December 7, 2013
Processing time: 115 Days and 13.2 Hours
The occurrence of adult intussusception from small intestinal lymphoma is quite rare. We present an 82-year-old man with a two-month history of intermittent abdominal pain, nausea and fatigue. Clinical symptoms included moderate abdominal tenderness in the right lower abdomen. Computed tomography scan of the abdomen revealed a mass in the terminal ileum with the sign of “bowel within bowel” which was suspicious of ileo-ileum intussusception. The patient underwent laparoscopic segmental ileal resection. Pathologic evaluation revealed a diffuse large B cell non-Hodgkin’s lymphoma of the ileum. The postoperative course was uneventful.
Core tip: Intussusception is a common cause of bowel obstruction in pediatric patients. Primary diffuse large B cell non-Hodgkin’s lymphoma of the small intestine is rare. Intussusception due to primary diffuse large B cell non-Hodgkin’s lymphoma in the small intestine is even rarer in adults and is often difficult to diagnose. This article describes the diagnosis and management of this rare disease.
- Citation: Xu XQ, Hong T, Li BL, Liu W. Ileo-ileal intussusception caused by diffuse large B-cell lymphoma of the ileum. World J Gastroenterol 2013; 19(45): 8449-8452
- URL: https://www.wjgnet.com/1007-9327/full/v19/i45/8449.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i45.8449
Intussusception is most often seen in infants and children and only 5% of all cases occur in adults. It accounts for about 1% of all cases of adult bowel obstruction. Adult intussusception is rare and about 40% are related to malignant lesions[1]. In general, most lesions in the small intestine are benign. Malignant lesions account for up to 30% of all cases of intussusception in the small intestine. Intussusception occurring in the large bowel is more likely to be related to malignant lesions in 63%-68% of cases[2]. Primary malignant tumors of the small intestine are very rare, accounting for less than 2% of all gastrointestinal malignancies. Malignant lesions resulting in intussusception in the small intestine include primary adenocarcinoma, gastrointestinal stromal tumors (GISTs), lymphoma and carcinoid tumors[3].
The gastrointestinal tract is the most common site of primary extranodal non-Hodgkin’s lymphoma (NHL), accounting for 20%-40% of all extranodal disease[4]. The stomach (50%-60%) is the most frequently affected site, followed by the small bowel (20%-30%), whereas 85% of primary gastrointestinal lymphomas and 60%-80% of intestinal lymphomas are B-cell type followed by T-cell NHL and Hodgkin’s lymphoma[5]. The ileum is the most common site of small intestine lymphoma. Intussusception is very rarely seen in intestinal NHL and the most common type of lymphoma causing intussusception is diffuse B-cell NHL[5].
We herein describe a case of adult ileal intussusception caused by diffuse large B-cell lymphoma of the small bowel in an 82-year-old male patient.
An 82-year-old male was admitted with a two-month history of intermittent abdominal pain, nausea and fatigue. He also complained of marked weight loss (8 kg) during the last two months. He was diagnosed with incomplete intestinal obstruction and was supported with parenteral nutrition in the community hospital. His past medical history was hypertension for 20 years. Physical examination revealed moderate abdominal tenderness in the right lower abdomen.
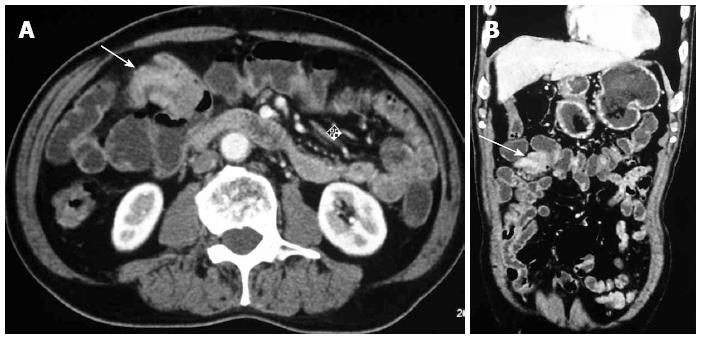
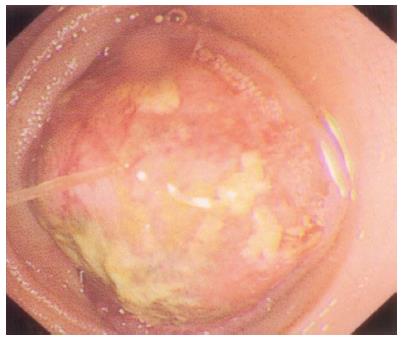
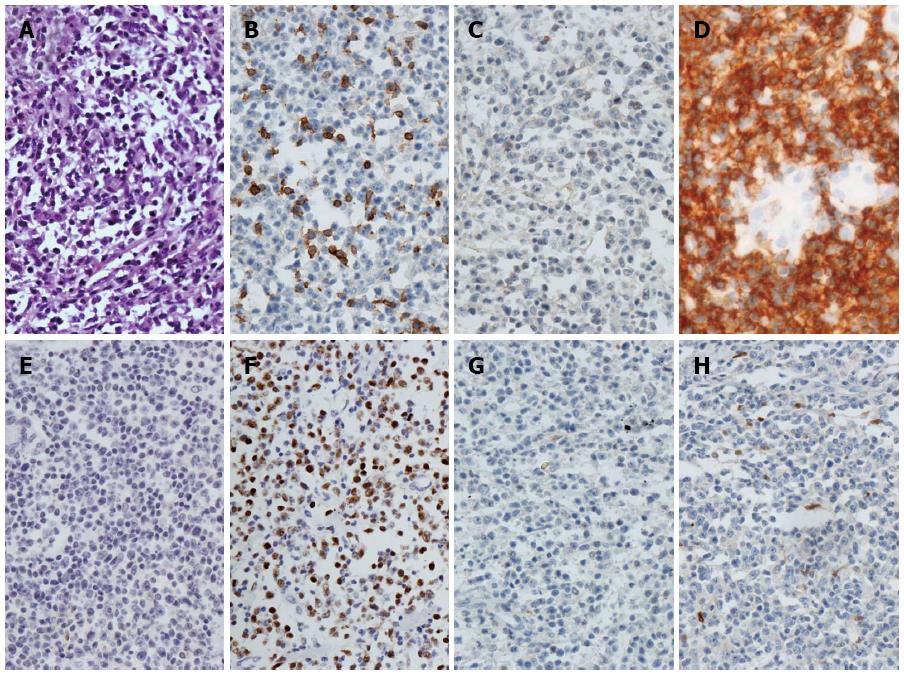
Blood tests revealed a white blood cell count of 4.1 × 109/L with 63% neutrophils and a hemoglobin level of 96 g/L with a hematocrit of 29%. His liver and kidney function test results and tumor marker (CEA, CA19-9, CA242 and CA724) levels were all normal. The fecal occult blood test was positive. Plain abdominal radiography was unremarkable. Contrast-enhanced computed tomography (CT) showed multiple lymphadenoma in the mesentery root of the small intestine and posterior peritoneum, a mass in the terminal ileum with the sign of “bowel within bowel” was suspicious of ileo-ileum intussusception (Figure 1). Positron emission tomography and computed tomography (PET-CT) showed high metabolism in the terminal ileum and multiple lymph nodes with high metabolism in the mesentery root of the small intestine, in which malignant lesions in the terminal ileum were considered (Figure 2). Therefore, balloon-assisted enteroscopy was performed. A mass, approximately 50 cm away from the ileocecal valve, almost filled the ileal cavity (Figure 3) and did not allow the enteroscope to pass. A biopsy was taken from this lesion and the pathology result showed a diffuse large B cell NHL of the ileum (Figure 4). Laparoscopic exploration was performed due to low hemoglobin, weight loss and the mass with suspected intussusception on CT. A tumor mass of 5.0 cm × 3.0 cm was revealed with ileo-ileum intussusception which was 40 cm distal to the ileum with multiple lymphadenoma in the mesentery root of the small intestine. A segmental ileal resection was performed laparoscopically. After opening the specimen, a mass of approximately 3 cm was found in the ileum wall almost filling the ileal cavity. The histopathological findings were suggestive of a diffuse large B cell NHL of the ileum (Figure 4), which was consistent with the preoperative pathological results of endoscopic biopsy. Tumor infiltration was detected in 2 of 16 lymph nodes. The postoperative course was uneventful. Bone marrow biopsies showed a normal marrow without infiltration. Cervical and chest PET-CT scans were unremarkable. Postoperative chemotherapy with cyclophosphamide, doxorubicin, vincristine, and prednisolone combined with the monoclonal antibody, rituximab, was administered. At the 6-mo follow up, there was no evidence of tumor activity.
Intussusception is rare in adults (< 5%), but it is the most common cause of intestinal obstruction in infants aged 6-18 mo[1]. The characteristic pediatric presentation triad of abdominal pain, palpable abdominal mass and bloody stool is rarely seen in adult cases. An abdominal mass is palpated in 12%-30% of cases, whereas 6%-25% of cases present with complications of the disease such as obstruction, hemorrhage, perforation, or intussusception[5]. Most patients present with subacute (24.4%) or chronic (51.2%) symptoms of abdominal pain, nausea, vomiting and constipation. The non-specific clinical presentation makes the preoperative diagnosis difficult[6]. CT scan is one of the most useful preoperative diagnostic modalities for intussusception as it can show the thickened segment of bowel with an eccentrically placed crescent-like fatty area (bowel within bowel )[5]. If the patient does not have a complete intestinal obstruction, colonoscopy is helpful for the clinical and pathological diagnosis of intussusception. PET-CT is useful for detecting the primary benign or malignant lesion sites and the distal regions which may be involved in lymphoma, although it is not often routinely used[7].
About 52%-55% of adult intussusceptions occur in the small intestine[8]. Sixty-three percent of adult small intestinal intussusception cases were associated with benign lesions, 23% cases were idiopathic, and 14% cases were associated with malignant lesions[9]. The incidence of primary lymphomas in the small intestine accounts for less than 2% of all gastrointestinal malignancies and 10%-20% of small intestine malignancies[1].
The management of small intestine intussusception caused by NHL is mandatory surgical intervention for adult intussusception due to the high incidence of underlying malignancy in intussusceptions and the inability to differentiate non-operatively benign from malignant causes in enteric intussusceptions[5]. For adult small intestinal intussusception caused by NHL, primary surgical resection of the localized intestinal lesions with NHL is the treatment modality of choice, especially in patients who have complications of intussusception.
In conclusion, we describe the diagnosis of adult ileal intussusception with detailed images of this specific case. Adult intussusception must be considered in the differential diagnosis of patients with abdominal pain and vomiting. The work-up must include X-ray, ultrasound and CT scan of the abdomen and PET-CT in special cases. Surgical intervention is required and warranted once the diagnosis of intussusception is made, due to the high risk of malignancy and bowel obstruction.
Ileo-ileal intussusception caused by diffuse large B-cell lymphoma of the ileum.
Adult intussusception must be considered in the differential diagnosis of patients with abdominal pain and vomiting.
Diagnostic imaging must include X-ray, ultrasound and computed tomography scan of the abdomen which can show the sign of “bowel within bowel”.
Surgical intervention is required and warranted once the diagnosis of intussusception is made, due to the high risk of malignancy and bowel obstruction.
This is an interesting case report, which shows a rare case of ileo-ileal intussusception caused by diffuse large B-cell lymphoma of the ileum.
P- Reviewers: Djordjevic I, Gupte GL, Lee HC, Namikawa T, von Delius S S- Editor: Wen LL L- Editor: Webster JR E- Editor: Liu XM
| 1. | Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 648] [Cited by in RCA: 666] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 2. | Akbulut S. Unusual cause of adult intussusception: diffuse large B-cell non-Hodgkin’s lymphoma: a case report and review. Eur Rev Med Pharmacol Sci. 2012;16:1938-1946. [PubMed] |
| 3. | Goh BK, Quah HM, Chow PK, Tan KY, Tay KH, Eu KW, Ooi LL, Wong WK. Predictive factors of malignancy in adults with intussusception. World J Surg. 2006;30:1300-1304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 65] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Li B, Shi YK, He XH, Zou SM, Zhou SY, Dong M, Yang JL, Liu P, Xue LY. Primary non-Hodgkin lymphomas in the small and large intestine: clinicopathological characteristics and management of 40 patients. Int J Hematol. 2008;87:375-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 68] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Yin L, Chen CQ, Peng CH, Chen GM, Zhou HJ, Han BS, Li HW. Primary small-bowel non-Hodgkin’s lymphoma: a study of clinical features, pathology, management and prognosis. J Int Med Res. 2007;35:406-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Wang N, Cui XY, Liu Y, Long J, Xu YH, Guo RX, Guo KJ. Adult intussusception: a retrospective review of 41 cases. World J Gastroenterol. 2009;15:3303-3308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 142] [Cited by in RCA: 152] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 7. | Iwaya Y, Takenaka K, Akamatsu T, Yamada Y, Haba S, Matsuda K, Nakazawa H, Muraki T, Kaneko Y, Ito T. Primary gastric diffuse large B-cell lymphoma with orbital involvement: diagnostic usefulness of 18F-fluorodeoxyglucose positron emission tomography. Intern Med. 2011;50:1953-1956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Schuind F, Van Gansbeke D, Ansay J. Intussusception in adults--report of 3 cases. Acta Chir Belg. 1985;85:55-60. [PubMed] |
| 9. | Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 382] [Article Influence: 13.6] [Reference Citation Analysis (0)] |