Published online Oct 21, 2013. doi: 10.3748/wjg.v19.i39.6689
Revised: August 10, 2013
Accepted: September 13, 2013
Published online: October 21, 2013
Processing time: 117 Days and 3.7 Hours
Benign multicystic peritoneal mesothelioma (BMPM) is a rare cystic mesothelial lesion that occurs predominantly in reproductive aged women. A 56-year-old Caucasian male was admitted to our surgical department with a chief complaint of a painful mass in his right lower abdomen for almost 2 years. The physical examination revealed a palpable painful mass. Computed tomography demonstrated an irregular, cystic tumor in his right lower abdomen. There was no obvious capsule or internal septations. No enhancement after intravenous administration of contrast was noted. An exploratory laparotomy was performed, and a multicystic tumor and adherent to the caecum was noted. The walls of the cysts were thin and smooth, filled with clear fluid, and very friable. An en bloc resection of the tumor, including appendix and caecum, was performed. Histological examination revealed multiple cysts lined with flattened simple epithelial cells, and the capsule walls of the cysts were composed of fibrous tissue. Immunohistochemical analysis documented positive expression of mesothelial cells and calretinin. The final diagnosis was BMPM. The patient was well at 6-mo follow-up. BMPM is exceedingly rare lesion. A complete resection of the tumor is required. The diagnosis of BMPM is based on pathological analysis.
Core tip: Benign multicystic peritoneal mesothelioma (BMPM) is a rare cystic mesothelial lesion that occurs predominantly in reproductive aged women. The preoperative diagnosis of BMPM is difficult, and final diagnosis requires histological evaluation of a surgical specimen. In immunohistochemical analysis, positive expression of mesothelial cells and calretinin is always noted. The best treatment strategy for BMPM is en bloc removal, which can avoid recurrence. The recurrent rate after complete resection is about 50%; the recurrent tumor should be completely removed and follow-up including physical examination and imaging studies is required for all cases.
- Citation: Wang TB, Dai WG, Liu DW, Shi HP, Dong WG. Diagnosis and treatment of benign multicystic peritoneal mesothelioma. World J Gastroenterol 2013; 19(39): 6689-6692
- URL: https://www.wjgnet.com/1007-9327/full/v19/i39/6689.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i39.6689
Benign multicystic peritoneal mesothelioma (BMPM) is uncommon lesion usually occurring in women of reproductive age. Because of its rarity, preoperative diagnosis is difficult and its origin and pathogenesis are uncertain[1-3]. Here, we present a case of BMPM in a 56-year-old Caucasian male with a painful mass in right lower abdomen for 2 years. The preoperative diagnosis was angiolymphoma. An en bloc removal was performed. The final diagnosis was BMPM according to the findings of histological and immunohistochemical examinations. We hope that this information assists surgeons in recognizing the diagnosis and treatment of BMPM.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A 56-year-old Caucasian male was admitted to our surgical department with a chief complaint of a painful mass in his right lower abdomen for almost 2 years. His medical history was negative, and he smoked 20 cigarettes per day and stated mild alcohol consumption for 30 years. His vital signs were normal, and physical examination revealed a palpable painful mass in his right lower abdomen. Laboratory investigations, urine analysis, chest and abdominal radiographs did not reveal any abnormalities.
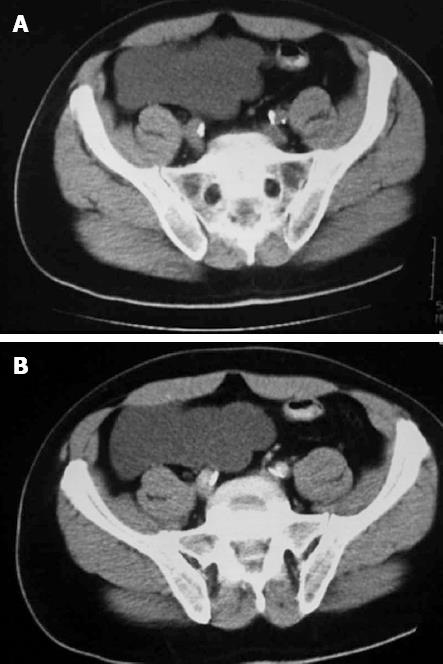
Computed tomography (CT) demonstrated a 13 cm × 12.9 cm × 6.1 cm irregular, cystic tumor in his right lower abdomen. There was no obvious capsule or internal septations. The Hounsfield value was 8, which demonstrated its cystic nature. No enhancement after intravenous administration of contrast was noted (Figure 1). Angiolymphoma was considered preoperatively.
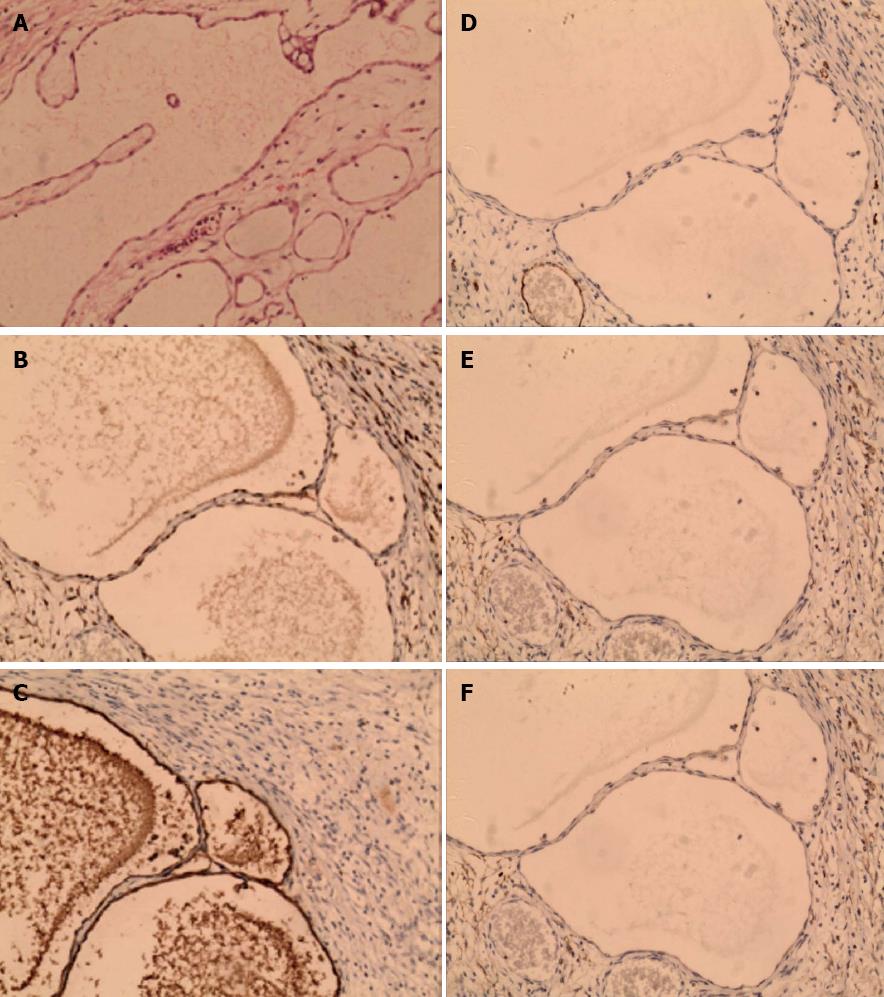
An exploratory laparotomy was performed under general anesthesia, and a multicystic tumor occupying the right abdomen and adherent to the caecum was noted. The walls of the cysts were thin and smooth, filled with clear fluid, and very friable (Figure 2). The multicystic mass, appendix, and caecum were removed. Histological examination revealed multiple cysts lined with flattened simple epithelial cells, and the capsule walls of the cysts were composed of fibrous tissue (Figure 3A). Immunohistochemical analysis documented positive expression of mesothelial cells (MC, Figure 3B) and calretinin (CR, Figure 3C), while expressions of D2-40, CD31, and CD34 were negative (Figure 3D-F). The final diagnosis was BMPM. The patient was discharged in good condition on postoperative day 10, and was free of symptoms at 6-mo follow-up.
Mesotheliomas always arise from pleural, pericardial, and peritoneal lining cells. BMPM is a rare lesion, and until 2009 only about 146 cases were documented in literature[2]. The characteristic behavior of BMPM is benign; however, rare cases of malignant transformation have been noted[4].
The pathogenesis of BMPM is still unclear; however, as the majority of cases occur reproductive aged females, it is believe that female sex hormones play a role in its pathogenesis[5,6]. Kurisu et al[7] reported finding small foci of endometriosis in BMPM cystic walls, and in a second case the lesion was adjacent to endometriotic cysts in the pelvic space. These histologic findings suggest that endometriosis contributes to the origin of BMPM. A history of right oophorectomy and left ovarian cystectomy for an ovarian tumor in a 23-year-old Japanese female with BMPM suggests that previous abdominal surgery is a risk factor for BMPM[8]. Husain et al[9] reported two cases of BMPM in females with concurrent colonic adenocarcinoma arising in the ileocecal region.
The most common presenting symptoms are chronic or intermittent abdominal or pelvic pain, tenderness, or distension with an abdominal or pelvic mass. The mean diameter of BMPM has been reported to be 13 cm at the time of diagnosis. On physical examination, the mass always presents as a fixed tumor with slight tenderness. Multiseptated anechoic cysts are always demonstrated by ultrasonography; however, CT is necessary to provide information about the location and extent of the mass and evidence of low-attenuation and non-calcified septa in the cysts[4]. Kemp et al[5] reported a case of BMPM in a middle-aged female that was diagnosed by fine needle core biopsy. An association between BMPM and increased serum CA19-9 concentration has been described, and a minimally invasive laparoscopic approach enabled not only histologic diagnosis but also surgical treatment[6].
Because BMPM is an extremely rare lesion, preoperative diagnosis is challenging. Definitive diagnosis relies on histological examination, which demonstrates multiple cysts with thin walls lined with single-layered or cuboidal mesothelia and filled with serous fluid. In immunohistochemical analysis, positive expression of MC and CR, which are markers for mesothelial cells, is always noted. The differential diagnosis primarily includes lymphangioma and malignant peritoneal mesothelioma (MPM). Lymphangioma can be identified if cysts present with predominantly chylous fluid, lymphoid aggregates, smooth muscle, and CD2-40 positive expression on immunohistochemical analysis. MPM always presents a history of exposure to asbestos, abdominal pain, distension, ascites, and weight loss. A plain chest radiograph may show signs of asbestos. An abdominal CT examination may show the presence of ascitic fluid and peritoneal thickening. At laparotomy, widespread nodular thickening of the visceral peritoneum with a striking, diffusely uniform, erythematous appearance can be confirmed to be MPM[10].
The best treatment strategy for BMPM is en bloc removal, which can avoid recurrence. The correlation between rupture of cystic lesion of BMPM and recurrence tumor is uncertain. Because of its benign nature, adjuvant chemotherapy and/or radiotherapy are not indicated for patients with BMPM. Other treatments such as hormonal therapy, sclerotherapy, and thermotherapy have not been proven to provided uncertain therapeutic effects. Although the prognosis is excellent, the recurrent rate after complete resection is about 50%; thus, the goal should not be a cure, but symptomatic relief through individualization of treatment. For the rare cases in which malignant transformation occurs, the recurrent tumor should be completely removed and follow-up including physical examination and imaging studies is required for all cases[11-13].
BMPM is a rare tumor, which is not associated with specific complaints, objective signs, or unique appearance on imaging studies. Preoperative diagnosis is very difficult, and the final diagnosis always requires pathological analysis. En bloc removal of BMPM is the ideal treatment strategy, and malignant transformation is rare. Further studies are needed to better understand its etiology and pathogenesis.
P- Reviewers Hotta T, Beidoux V S- Editor Zhai HH L- Editor A E- Editor Zhang DN
| 1. | Dzieniecka M, Kałużyński A. Benign multicystic peritoneal mesothelioma (BMPM) - case report and review of the literature. Pol J Pathol. 2011;62:122-124. [PubMed] |
| 2. | Koo PJ, Wills JS. Case 146: Benign multicystic mesothelioma. Radiology. 2009;251:944-946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Asghar S, Qureshi N, Awan A. Benign mesothelioma of peritoneum presenting as a pelvic mass. J Coll Physicians Surg Pak. 2008;18:723-725. [PubMed] |
| 4. | Pitta X, Andreadis E, Ekonomou A, Papachristodoulou A, Tziouvaras C, Papapaulou L, Sapidis N, Chrisidis T. Benign multicystic peritoneal mesothelioma: a case report. J Med Case Rep. 2010;4:385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Kemp AM, Nayar R, De Frias D, Lin X. Cytomorphologic characteristics of fine needle core biopsy of multicystic peritoneal mesothelioma: a case report and review of the literature. Diagn Cytopathol. 2010;38:192-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 6. | Pinto V, Rossi AC, Fiore MG, D’Addario V, Cicinelli E. Laparoscopic diagnosis and treatment of pelvic benign multicystic mesothelioma associated with high CA19.9 serum concentration. J Minim Invasive Gynecol. 2010;17:252-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Kurisu Y, Tsuji M, Shibayama Y, Yamada T, Ohmichi M. Multicystic mesothelioma caused by endometriosis: 2 case reports and review of the literature. Int J Gynecol Pathol. 2011;30:163-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Takemoto S, Kawano R, Honda K, Nakazono A, Shimamatsu K. Benign multicystic peritoneal mesothelioma mimicking recurrence of an ovarian borderline tumor: a case report. J Med Case Rep. 2012;6:126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Husain A, Ozdemirli M. Benign multicystic mesothelioma with concurrent colonic adenocarcinoma: a report of two cases. Surg Today. 2012;42:978-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Naraynsingh V, Ramdass MJ, Lum CL. Malignant peritoneal mesothelioma presenting as recurrent adhesion obstruction in general surgery: a case report. J Med Case Rep. 2011;5:420. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Vallerie AM, Lerner JP, Wright JD, Baxi LV. Peritoneal inclusion cysts: a review. Obstet Gynecol Surv. 2009;64:321-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Safioleas MC, Constantinos K, Michael S, Konstantinos G, Constantinos S, Alkiviadis K. Benign multicystic peritoneal mesothelioma: a case report and review of the literature. World J Gastroenterol. 2006;12:5739-5742. [PubMed] |
| 13. | Cavallaro A, Berretta M, Lo Menzo E, Cavallaro V, Zanghì A, Di Vita M, Cappellani A. Cystic peritoneal mesothelioma: report of a case. Surg Today. 2011;41:141-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |