Published online Sep 21, 2013. doi: 10.3748/wjg.v19.i35.5940
Revised: April 24, 2013
Accepted: May 17, 2013
Published online: September 21, 2013
Processing time: 250 Days and 14.3 Hours
We report the case of a 17-year-old male admitted to our academic hospital with massive rectal bleeding. Since childhood he had reported recurrent gastrointestinal bleeding and had two exploratory laparotomies 5 and 2 years previously. An emergency abdominal computed tomography scan, gastroscopy and colonoscopy, performed after hemodynamic stabilization, were considered normal. High-dose intravenous proton pump inhibitor (PPI) therapy was initiated and bleeding stopped spontaneously. Two other massive rectal bleeds occurred 8 h after each cessation of PPI which led to a hemostatic laparotomy after negative gastroscopy and small bowel capsule endoscopy. This showed long tubular duplication of the right colon, with fresh blood in the duplicated colon. Obscure lower gastrointestinal bleeding is a difficult medical situation and potentially life-threatening. The presence of ulcerated ectopic gastric mucosa in the colonic duplication explains the partial efficacy of PPI therapy. Obscure gastrointestinal bleeding responding to empiric anti-acid therapy should probably evoke the diagnosis of bleeding ectopic gastric mucosa such as Meckel’s diverticulum or gastrointestinal duplication, and gastroenterologists should be aware of this potential medical situation.
Core tip: Obscure lower gastrointestinal bleeding is a difficult medical situation and potentially life threatening. The collaboration between endoscopists and radiologists usually allow location of the source of bleeding, but some rare situations, such as gastrointestinal malformations, need surgical intervention to diagnose and concomitantly treat an obscure bleeding source. In terms of medical therapy, only proton pump inhibitor therapy has efficacy in peptic ulcer disease. Obscure gastrointestinal bleeding responding to empiric antacid therapy should suggest the diagnosis of bleeding ectopic gastric mucosa such as Meckel’s diverticulum or gastrointestinal duplication, and gastroenterologists should be aware of this potential medical situation.
- Citation: Jacques J, Projetti F, Legros R, Valgueblasse V, Sarabi M, Carrier P, Fredon F, Bouvier S, Loustaud-Ratti V, Sautereau D. Obscure bleeding colonic duplication responds to proton pump inhibitor therapy. World J Gastroenterol 2013; 19(35): 5940-5942
- URL: https://www.wjgnet.com/1007-9327/full/v19/i35/5940.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i35.5940
Obscure lower gastrointestinal bleeding is a difficult medical situation which is potentially life-threatening. No medical therapy is currently available to manage these patients until endoscopic, radiologic or surgical therapy is performed after the identification of the bleeding lesion. Proton pump inhibitor (PPI) therapy is not recommended for bleeding lesions downstream of the angle of Treitz. We describe here the partial efficacy of PPI therapy in massive obscure gastrointestinal bleeding due to a bleeding ulcer in the ectopic gastric mucosa of an undiagnosed colonic duplication.
A 17-year-old male was admitted to the emergency room of our academic hospital with massive rectal bleeding. He had reported recurrent gastrointestinal bleeding since childhood, which led to multiple hospitalizations. At 5 and 2 years before this admission he underwent exploratory laparotomies because of suspicion of a Meckel diverticulum. On admission, blood pressure was lowered to 80/55 mmHg, with a reflex tachycardia of 120 beats/min. The hemoglobin level was 5.7 g/dL. Initial resuscitation required significant volume replacement, and the transfusion of 3 blood units and 3 fresh bags of frozen plasma. High-dose intravenous PPI therapy at the dosage used in peptic ulcer bleeding (8 mg/h) was initiated.
An emergency abdominal computed tomography (CT) scan, performed after hemodynamic stabilization, was considered normal. A gastroscopy and an ileocolonoscopy, with a water-jet device after preparation by an enema, were normal. Bleeding stopped spontaneously, and after a 24-h clinical and biological stabilization, we decided to stop the PPI therapy because of the absence of gastroduodenal ulcer disease.
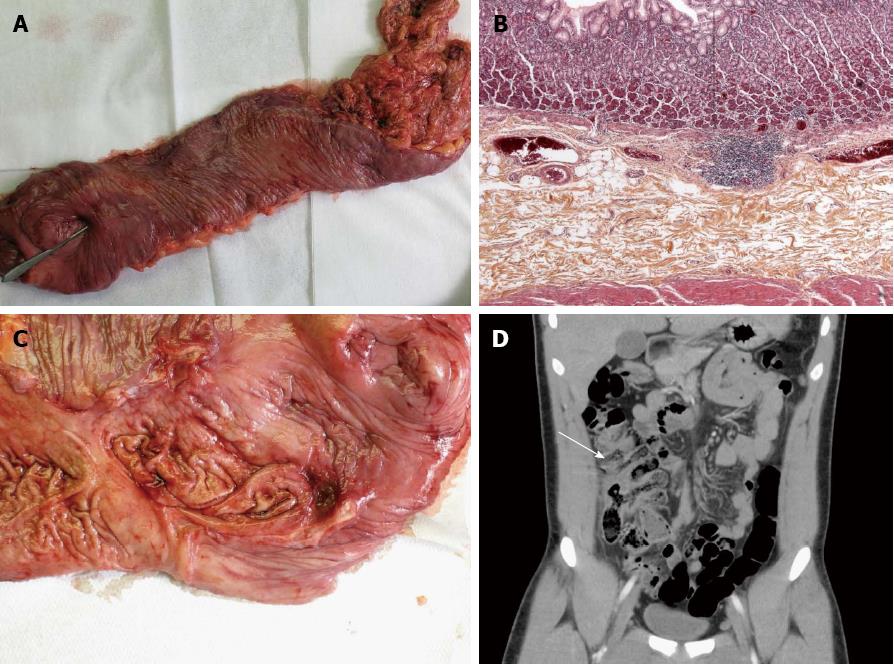
Unfortunately, a further massive rectal bleed consisting of red fresh blood with melena, and hemodynamic instability occurred 8 h later. High dose intravenous PPI therapy was reintroduced and gastroscopy conducted by a French national expert in endoscopy was once again considered normal. Small bowel capsule endoscopy was then performed and his initial interpretation eliminated a bleeding lesion upstream of the angle of Treitz. PPI therapy was once again stopped and 8 h later a third massive rectal bleed occurred which led to selective mesenteric arteriography. This showed suspicious hypervascularization of the right colon. Hemostatic laparotomy was performed because of the patient’s unstable condition and lack of a diagnosis. This showed long tubular duplication of the right colon, which was connected to the cecum at one end (Figure 1A), with fresh blood in the duplicated colon. Although anastomosis was not visible during the endoscopy, the capsule was seen inside the duplicated colon. Hemostatic right hemicolectomy with ileocolonic anastomosis was performed. Pathological analysis (Figure 1B) showed intestinal duplication, with intimate attachment to the mesentery, a smooth muscle coat and an ectopic gastric mucosal lining. A large ulcer with stigma of recent hemorrhage (Figure 1C) was present near the anastomosis. Retrospective analysis of the CT scan by a senior gastrointestinal radiologist using coronal reconstruction agreed with our diagnosis as difficult and rare, but possible (Figure 1D, arrow). Two years after the surgery, the patient had no further gastrointestinal bleeding.
Duplications of the gastrointestinal tract are rare congenital anomalies that can occur anywhere along its length[1,2], and are characterized by attachment to at least one part of the tract, a layer of smooth muscle and epithelial lining resembling some part of the tract[3]. Colonic duplication is a rare abnormality, accounting for 4%-18% of all gastrointestinal duplications, and is usually located in the cecum. Tubular types are found in only 18% of cases and are most often encountered in the small and large bowel. Gastric mucosa is frequently observed in the wall of the duplications, irrespective of their site of origin in the alimentary tract[3]. Clinically, they can become a problem at any age, but the majority are discovered during the neonatal period or infancy[4,5]. They can manifest as abdominal masses[6], bowel obstruction and gastrointestinal hemorrhage[7]. A diagnosis of intestinal duplication can be difficult and is usually performed intraoperatively.
This case highlights the diagnostic and therapeutic evaluation during massive gastrointestinal bleeding of unknown origin. First, despite all diagnostic tools available nowadays in a tertiary center, obscure gastrointestinal bleeding can sometimes be a diagnostic and therapeutic challenge. The growing efficacy of endoscopic devices (gastroscopy, colonoscopy with washing-pump, small bowel capsule endoscopy and enteroscopy) and radiologic procedures (high resolution CT scan, arteriography) tend to make the surgical procedure therapeutic only. This case highlights the unusual but still existing role of surgery in the diagnosis and treatment of massive gastrointestinal bleeds of unknown etiology[8] in challenging cases. Whereas such a role is common in cases of obscure bleeding during childhood, the usefulness of surgical exploration must not be ignored in adults. Gastrointestinal congenital malformations such as colonic duplication are a rare cause of obscure gastrointestinal bleeding. Coronal and sagittal reconstruction of CT scans can be very useful and must always be made in cases where there is an absence of diagnosis.
In terms of medical therapy, PPI therapy represents the treatment of choice in non-portal hypertensive gastrointestinal bleeding of the upper gastrointestinal tract[9]. No drugs are approved nowadays for the management of lower gastrointestinal hemorrhage[8]. In this case, the discrepancy in the efficacy of PPI therapy and no sign of a gastroduodenal ulcer is explained by the pathology result. High dose PPI therapy probably acted on the bleeding ulcer existing in the ectopic gastric mucosa in the duplicated right colon. Rare cases have already been reported on the hemostatic efficacy of anti-acid therapy (H2-receptor antagonist or PPI) in bleeding Meckel’s diverticula whose histological analysis reveals ectopic gastric mucosa in more than half of the cases[10]. Obscure gastrointestinal bleeding responding to empiric anti-acid therapy should probably suggest the diagnosis of bleeding ectopic gastric mucosa such as Meckel’s diverticulum or gastrointestinal duplication.
P- Reviewers Guslandi M, Klinge U, Liu QD S- Editor Huang XZ L- Editor Cant MR E- Editor Ma S
| 1. | Dahshan A. Bleeding Meckel diverticulum responds to intravenous pantoprazole. South Med J. 2007;100:334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 62] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Holcomb GW, Gheissari A, O’Neill JA, Shorter NA, Bishop HC. Surgical management of alimentary tract duplications. Ann Surg. 1989;209:167-174. [PubMed] |
| 3. | Macpherson RI. Gastrointestinal tract duplications: clinical, pathologic, etiologic, and radiologic considerations. Radiographics. 1993;13:1063-1080. [PubMed] |
| 4. | Iyer CP, Mahour GH. Duplications of the alimentary tract in infants and children. J Pediatr Surg. 1995;30:1267-1270. [PubMed] |
| 5. | Hernandez Troya AC, Gebara S, Bloom DA, Chan W. Occult colonic duplication. Clin Pediatr (Phila). 2011;50:550-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Carneiro FP, de Nazareth Sobreira M, de Azevedo AE, Alves AP, Campos KM. Colonic duplication in an adult mimicking a tumor of pancreas. World J Gastroenterol. 2008;14:966-968. [PubMed] |
| 7. | Fotiadis C, Genetzakis M, Papandreou I, Misiakos EP, Agapitos E, Zografos GC. Colonic duplication in adults: report of two cases presenting with rectal bleeding. World J Gastroenterol. 2005;11:5072-5074. [PubMed] |
| 8. | Barnert J, Messmann H. Diagnosis and management of lower gastrointestinal bleeding. Nat Rev Gastroenterol Hepatol. 2009;6:637-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 9. | Holster IL, Kuipers EJ. Management of acute nonvariceal upper gastrointestinal bleeding: current policies and future perspectives. World J Gastroenterol. 2012;18:1202-1207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 66] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (1)] |