Published online Mar 21, 2013. doi: 10.3748/wjg.v19.i11.1805
Revised: December 17, 2012
Accepted: December 25, 2012
Published online: March 21, 2013
Processing time: 148 Days and 13.4 Hours
AIM: To investigate the impact of esophagogastroduodenoscopy with conscious sedation on the subsequent 24-h catheter-based pH monitoring.
METHODS: Fifty patients with extra-esophageal symptoms of gastroesophageal reflux disease undergoing ambulatory dual-probe 24-h pH monitoring were enrolled from March 2010 to August 2011. All of the data were collected prospectively and analyzed retrospectively. Thirty-six patients (72%, group A) underwent pH monitoring shortly after esophagogastroduodenoscopy (EGD) with conscious sedation, and 14 patients (28%, group B) underwent pH monitoring without conscious sedation. The 24-h pH data from two time periods were analyzed: the first 4 h (Period I) and the remaining time of the study (Period II).
RESULTS: The mean age of the patients was 49.6 ± 12.5 years; 20 patients (40%) were men. The baseline data, including age, sex, body mass index, reflux esophagitis, the Reflux Symptom Index, and the Reflux Findings Score, were comparable between the two groups. The percentage of total time with a pH < 4 and the frequency of acid reflux during Period I were not significantly different between the two groups, as measured using both pharyngeal (0.03% ± 0.10% vs 0.07% ± 0.16%, P = 0.32; and 0.07 ± 0.23 episodes/h vs 0.18 ± 0.47 episodes/h, P = 0.33, respectively) and esophageal probes (0.96% ± 1.89% vs 0.42% ± 0.81%, P = 0.59; and 0.74 ± 1.51 episodes/h vs 0.63 ± 0.97 episodes/h, P = 0.49, respectively). The percentage of total time with a pH < 4 and the frequency of acid reflux were also not significantly different between Periods I and II in group A patients, as measured using both pharyngeal (0.03% ± 0.10% vs 0.23% ± 0.85%, P = 0.21; and 0.07 ± 0.23 episodes/h vs 0.29 ± 0.98 episodes/h, P = 0.22, respectively) and esophageal probes (0.96% ± 1.89% vs 1.11% ± 2.57%, P = 0.55; and 0.74 ± 1.51 episodes/h vs 0.81 ± 1.76 episodes/h, P = 0.55, respectively).
CONCLUSION: EGD with conscious sedation does not interfere with the results of subsequent 24-h pH monitoring in patients with extra-esophageal symptoms of gastroesophageal reflux disease.
- Citation: Tsou YK, Lien JM, Chen CK, Lin CH, Chen HY, Lee MS. Esophagogastroduodenoscopy with conscious sedation does not interfere with catheter-based 24-h pH monitoring. World J Gastroenterol 2013; 19(11): 1805-1810
- URL: https://www.wjgnet.com/1007-9327/full/v19/i11/1805.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i11.1805
The manifestation of gastroesophageal reflux disease (GERD) can be either esophageal or extra-esophageal[1]. Extra-esophageal reflux, or laryngopharyngeal reflux (LPR), refers to the backflow of gastric contents into the larynx and pharynx[1,2]. Ambulatory dual-probe 24-h pH monitoring is currently considered the gold-standard diagnostic modality for the evaluation of patients with LPR[2-4]. This catheter-based pH measurement is performed with a pH sensor located within 2 cm above the proximal border of the upper esophageal sphincter (UES)[5]. Prior manometry-guided localization is required to determine UES positioning relative to the nostril. The two trans-nasal procedures are usually performed without intravenous sedation. Therefore, they are unpleasant and uncomfortable tests for patients[6,7].
Conscious sedation improves the quality of the test and increases the patient’s willingness to undergo a gastrointestinal examination[8]. Benzodiazepine administration and opiate-based sedation are the most common practices for conscious sedation[9]. Meperidine causes a reduction in the LES pressure in animal and human studies[10,11]. It may induce or exacerbate gastroesophageal reflux (GER), causing interference with pH studies[11]. However, capsule-based (Bravo) wireless pH measuring system is usually performed during or shortly after an esophagogastroduodenoscopy (EGD) with conscious sedation[12]. Therefore, it is unclear whether conscious sedation during EGD has an impact on the results of the subsequent esophageal pH test. To increase patient willingness to undergo 24-h pH monitoring, we attempted to perform a catheter-based pH study in a manner similar to the Bravo system in our patients. The aim of this study was to investigate whether EGD with conscious sedation interfered with subsequent catheter-based 24-h pH monitoring in patients with extra-esophageal symptoms of GERD.
From March 2010 to August 2011, 53 patients with LPR-like complaints underwent ambulatory 24-h pH monitoring at the Chang Gung Memorial Hospital. These complaints included globus (n = 27), sore throat (n = 13), chronic cough (n = 9), hoarseness (n = 3), and dysphagia (n = 1). Three patients were excluded from the analysis because of numerous artifacts (pH out of range) on their pH records (n = 2) and intolerance of the procedure (n = 1). All of the patients were instructed to discontinue any medications that affect gastric acid secretion and esophageal motility at least 7 d prior to the 24-h pH monitoring. This cohort study was incorporated into a prospective study (CMRPG390591) that was originally designed to evaluate the effects of different doses of proton pump inhibitors on the treatment of LPR. All of the data were collected prospectively and analyzed retrospectively. The study protocol was approved by the ethics committee at Chang Gung Memorial Hospital (IRB No: 99-3494C).
A total of 50 patients were enrolled in the current study. The mean patient age was 49.6 ± 12.5 years (range, 20-76 years). There were 20 (40%) men and 30 (60%) women. The mean body mass index (BMI) was 23.0 ± 3.2 kg/m2 (range, 18.1-30.0 kg/m2). Group A included 36 patients (72%) who underwent EGD with conscious sedation 30 min prior to pH monitoring. Group B included the remaining 14 patients (28%) who did not undergo EGD or conscious sedation on the same day.
All of the patients in group A underwent EGD with intravenous sedation using meperidine and midazolam on the same day prior to their 24-h pH monitoring study. The dosage of meperidine was 0.52 ± 0.10 mg/kg (range, 0.32-0.81 mg/kg), and the dosage of midazolam was 33.1 ± 7.1 g/kg (range, 16.1-53.6 g/kg). Hyoscine butylbromide was not given before or during the endoscopy in any of the participants.
All of the patients underwent esophageal manometry using a station pull-through technique to locate the UES in reference to the nostril. Subsequently, 24-h pH monitoring was performed using antimony electrodes and fitting recorders (Orion II, Medical Measurement Systems, The Netherlands). The pH catheter had two or four sensors that were 15 cm or 5 cm apart. The pH electrodes were calibrated before and after the test using reference buffer solutions with a pH of 4 or 7. The most proximal electrode (pharyngeal probe) was placed in the hypopharynx 2 cm above the manometry-defined proximal border of the UES. Each patient wore a data-logger with a sampling frequency of 1 Hz during the test period. Symptom occurrence, meal times and body positions (supine or upright) were written down in a diary and recorded in a data log. The patients were advised to eat their usual meals and engage in their usual activities on the day of the test. After a period of 24 h, they returned the data log, and the data were downloaded onto a computer using software provided by the manufacturer. The data from the diaries were extracted for interpretation.
A single pharyngeal event (pH < 4) preceded by a precipitous pH drop of the same magnitude in the esophageal probe was defined as a positive result for LPR. The most distal pH sensor in the esophagus (esophageal probe) was 15 cm away from the pharyngeal probe. Pathologic GER was defined as a percentage of total time with a pH < 4 greater than 4.2% as measured by the esophageal probe[13].
The elimination half-life of meperidine is 3.2-3.7 h, and the half-life of midazolam is approximately 3 h[14,15]. To analyze the effect of conscious sedation on 24-h pH monitoring, computer software provided by MMS was used to analyze the 24-h pH data of each patient during two periods: the first 4 h (Period I) and the remaining time of the study (Period II). Meal times and sleep h were excluded from the analysis. Thus, only data recorded when the patients assumed an upright position were used for the comparisons. The mean duration of each period was 3.5 ± 0.5 h for Period I and 10.1 ± 2.1 h for Period II.
An acid reflux event was defined as an episode of pH < 4 detected on the pharyngeal or esophageal probe. Long reflux was defined as a reflux event lasting more than 5 min. The variables used for the comparisons were percentage of total time with a pH < 4, frequency of acid reflux events (episodes/h), and presence of long reflux.
Continuous variables are expressed as the mean ± SD in the text and tables. The differences in the variables between patients in group A and B were compared using a t test for age and a Mann-Whitney U test for BMI, Reflux Symptom Index (RSI), Reflux Finding Score (RFS), percentage of total time with a pH < 4, and frequency of acid reflux. Either a χ2 or Fisher’s exact test (when χ2 test was inappropriate) was used to analyze differences in sex, presence of heartburn and regurgitation, erosive esophagitis, LPR, pathologic GER, and long reflux. The differences in the variables between Period I and Period II in group A patients were compared using a Wilcoxon Signed Rank test for the percentage of total time with a pH < 4, frequency of symptoms, and the presence of acid reflux. A McNemar’s test was used to analyze differences in the presence of long reflux. Statistical significance was defined as P < 0.05. The statistical analyses were performed using the SPSS version 17.0 for Windows.
The demographic, clinical, and endoscopic data from the patients in groups A and B were compared (Table 1). There were no significant differences between the two groups. Characteristic symptoms of GERD, heartburn and acid regurgitation were present in both groups (13/36 vs 7/14, P = 0.37). Six patients (16.7%) in group A and 2 (14.3%) in group B had erosive esophagitis (all were grade A, except one patient in group A who was grade B based on the Los Angeles classification) on the EGD (P = 1). The RSI is a validated patient-administered questionnaire for the diagnosis of LPR[16]. A total score greater than 13 is regarded as a positive result. The patients in group A scored 15.9 ± 7.5, and the patients in group B score 16.8 ± 9.2 (P = 0.62). The RFS is an 8-item scale listing common physical findings in LPR patients[17]. A total score of greater than 7 is regarded as a positive result. The RFS was 8.1 ± 3.7 in group A and 6.4 ± 2.4 in group B (P = 0.19). Twelve patients (33.3%) in group A and 5 (35.7%) in group B met the pH criteria for LPR (P = 0.87). There were three (8.3%) patients in group A and one (7.1%) in group B who had pathologic GER (P = 1.00).
| Variables | Group A(n = 36) | Group B(n = 14) | P value1 |
| Baseline data | |||
| Age (yr) | 49.5 ± 13.2 | 49.9 ± 11.0 | 0.91 |
| Sex (F) | 15 (41.7) | 5 (35.7) | 0.70 |
| Body mass index | 22.8 ± 3.2 | 23.3 ± 3.4 | 0.75 |
| Presence of heartburn or regurgitation | 13 (36.1) | 7 (50) | 0.37 |
| Erosive esophagitis on EGD | 6 (16.7) | 2 (14.3) | 1 |
| Reflux symptom index | 15.9 ± 7.5 | 16.8 ± 9.2 | 0.62 |
| Reflux findings score | 8.1 ± 3.7 | 6.4 ± 2.4 | 0.19 |
| Positive for LPR | 12 (33.3) | 5 (35.7) | 0.87 |
| Positive for pathologic GER | 3 (8.3) | 1 (7.1) | 1 |
| Data obtained during the first 4 h | |||
| Frequency of symptoms onset (episodes/h) | 0.04 ± 0.1 | 0.14 ± 0.22 | 0.08 |
| Pharyngeal probe | |||
| Total time of pH < 4 (%) | 0.03 ± 0.10 | 0.07 ± 0.16 | 0.32 |
| Mean frequency of reflux (episodes/h) | 0.07 ± 0.23 | 0.18 ± 0.47 | 0.33 |
| Patients with long reflux | 0 | 0 | 1 |
| Esophageal probe | |||
| Total time of pH < 4 (%) | 0.96 ± 1.89 | 0.42 ± 0.81 | 0.59 |
| Mean frequency of reflux (episodes/h) | 0.74 ± 1.51 | 0.63 ± 0.97 | 0.49 |
| Patients with long reflux | 1 (2.8) | 0 | 1 |
The pH data obtained from Period I were compared between the two groups (Table 1). Using the pharyngeal probe, the percentage of total time with a pH < 4 was 0.03% ± 0.10% (range, 0%-0.4%) in group A and 0.07% ± 0.16% (range, 0%-0.5%) in group B (P = 0.32). The frequency of acid reflux events was 0.07 ± 0.23 episodes/h (range, 0-1.1 episodes/h) in group A and 0.18 ± 0.47 episodes/h (range, 0-1.7 episodes/h) in group B (P = 0.33). None of the patients in either group had long reflux events. Using the esophageal probe, the mean percentage of total time with a pH < 4 was 0.96% ± 1.89% (range, 0%-7%) in group A and 0.42% ± 0.81% (range, 0%-2.9%) in group B (P = 0.59). The frequency of acid reflux events was 0.74 ± 1.51 episodes/h (range, 0-6.3 episodes/h) in group A and 0.63 ± 0.97 episodes/h (range, 0-3.1 episodes/h) in group B (P = 0.49). One patient in group A and no patients in group B had long reflux (P = 1).
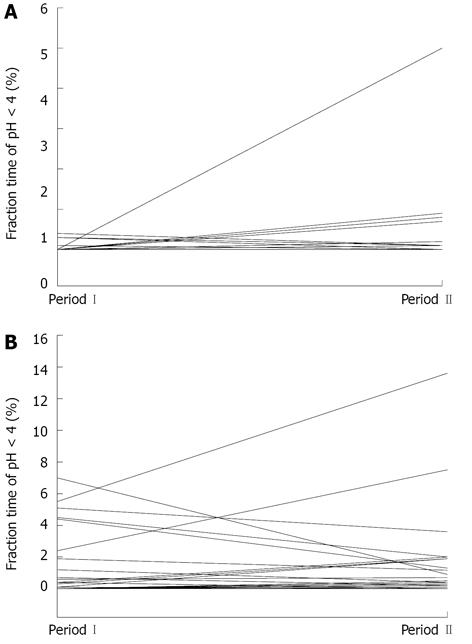
The pH data for Period I and Period II from the group A patients are shown in Table 2. The frequency of symptom occurrence was 0.04 ± 0.10 episodes/h (range, 0-0.3 episodes/h) during Period I and 0.03 ± 0.06 episodes/h (range, 0-0.3 episodes/h) during Period II (P = 0.29). Based on the pharyngeal probe measurements, the percentage of total time with a pH < 4 was 0.03% ± 0.10% (range, 0%-0.4%) in Period I and 0.23% ± 0.85% (range, 0%-5%) in Period II (P = 0.21, Figure 1A). The frequency of acid reflux was 0.07 ± 0.23 episodes/h (range, 0-1.1 episodes/h) in Period I and 0.29 ± 0.98 episodes/h (range, 0-5.7 episodes/h) in Period II (P = 0.22). None of the patients had a long reflux event. Based on the esophageal probe measurements, the percentage of total time with a pH < 4 was 0.96% ± 1.89% (range, 0%-7%) in Period I and 1.11% ± 2.57% (range, 0%-13.6%) in Period II (P = 0.55, Figure 1B). The frequency of acid reflux was 0.74 ± 1.51 episodes/h (range, 0-6.29 episodes/h) in Period I and 0.81 ± 1.76 episodes/h (range, 0-9.78 episodes/h) in Period II (P = 0.55). One patient had a long reflux event during Period I and five had a long reflux event during Period II (P = 0.22).
| Variables | Period I | Period II | P value1 |
| Frequency of symptom (episodes/h) | 0.04 ± 0.10 | 0.03 ± 0.06 | 0.29 |
| Pharyngeal probe | |||
| Total time of pH < 4 (%) | 0.03 ± 0.10 | 0.23 ± 0.85 | 0.21 |
| Mean frequency of reflux (episodes/h) | 0.07 ± 0.23 | 0.29 ± 0.98 | 0.22 |
| Patients with long reflux | 0 | 0 | 1 |
| Esophageal probe | |||
| Total time of pH < 4 (%) | 0.96 ± 1.89 | 1.11 ± 2.57 | 0.55 |
| Mean frequency of reflux (episodes/h) | 0.74 ± 1.51 | 0.81 ± 1.76 | 0.55 |
| Patients with long reflux | 1 (2.8%) | 5 (13.9%) | 0.22 |
EGD is usually performed without conscious sedation in Taiwan. Some of our patients reported that nasally passed procedures for esophageal manometry and 24-h pH monitoring were less tolerable than EGD without conscious sedation. Because moderate conscious sedation may be helpful to facilitate gastrointestinal procedures, we performed a catheter-based pH study in a manner similar to the Bravo system in our patients[8,12]. Our study results showed that EGD with conscious sedation does not have an immediate effect on subsequent catheter-based pH monitoring with regard to the relevant parameters assessed with pH monitoring techniques[6,18].
The Bravo capsule is usually placed during an EGD with conscious sedation[19-23]. The Bravo pH system allows for the measurement of esophageal acid exposure over a 48-h period. Therefore, many studies have investigated whether there is day-to-day discrepancy during Bravo pH monitoring[19-23]. The results are conflicting. Bechtold et al[19] and Bhat et al[20] reported more acid reflux events on day 1 than on day 2 using the Bravo system, suggesting that endoscopy and the associated sedatives may be responsible for the day-to-day discrepancy. Other studies showed that patients who underwent same-day EGD with intravenous sedation did not demonstrate any significant differences in reflux variables between day 1 and day 2 using Bravo pH monitoring[21-23].
Bhat et al[20] further analyzed their pH data by dividing the study period into the first 6 h and the remaining 18 h on both day 1 and day 2. They found an increase in esophageal acid exposure during the first 6 h after capsule insertion on day 1 compared to the corresponding period on day 2. There was no such difference during the remaining 18 h on day 1 and day 2. They concluded that EGD with conscious sedation interferes with subsequent capsule-based Bravo pH measurements. In this study, we divided the study period into the first 4 h and the remaining 20 h because the elimination half-life is nearly 4 h for meperidine and approximately 3 h for midazolam[14,15]. Our results showed no interference in patients who underwent EGD with sedation. Our data further revealed that three pH variables were not significantly different between the patients with and without prior sedation (using both the pharyngeal and laryngeal probes). Ayazi et al. observed a similar day-to-day discrepancy in patients receiving capsule-based Bravo pH monitoring without prior EGD and conscious sedation[24]. Their results argue for an iatrogenic effect of sedated EGD on the pH monitoring.
There are some limitations in the present study. First, the study cohort had extra-esophageal symptoms (LPR) but not esophageal symptoms (classical GERD). The mechanism of LPR may be different from that of classical GERD[2,25]. Therefore, whether the study results can be applied to pH monitoring in patients with characteristic symptoms of GERD needs further investigation. Second, the esophageal probe was placed at a variable distance above the proximal border of the LES of participants. The results of the pH parameters obtained from the esophageal probe may be suboptimal.
In conclusion, our results suggest that EGD with conscious sedation does not interfere with the results of subsequent catheter-based pH monitoring in patients with extra-esophageal manifestations of GERD. Catheter-based 24-h pH monitoring can be performed shortly after EGD with conscious sedation, especially for those patients who are intolerable to the procedures.
One of the limitations of catheter-based pH monitoring is discomfort. Whether it can be performed shortly after esophagogastroduodenoscopy (EGD) with conscious sedation like the performance of Bravo pH system is unknown. Authors aimed to investigate the impact of sedated EGD on the subsequent 24-h catheter-based pH monitoring.
In order to increase patients’ willingness to receive 24-h pH monitoring, authors have attempted to perform the catheter-based pH study in a similar way to Bravo system in our patients.
EGD with conscious sedation does not interfere with the results of the subsequent 24-h pH monitoring in patients with extraesophageal symptoms of gastroesophageal reflux disease.
Catheter-based 24-h pH monitoring can be performed shortly after sedated EGD especially for those patients who are intolerable to the procedures.
Laryngopharyngeal reflux is backflow of gastric content into larynx and pharynx which has been widely used by otolaryngologists, while extraesophageal reflux is commonly used by gastroenterologist.
The paper is well composed, documented. The results are interesting and suggest that EGD with conscious sedation does not interfere with the results of subsequent 24-h pH monitoring in patients with extra-esophageal symptoms of gastroesophageal reflux disease.
P- Reviewer Sivandzadeh GR S- Editor Gou SX L- Editor A E- Editor Zhang DN
| 1. | Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900-120; quiz 1943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2368] [Cited by in RCA: 2454] [Article Influence: 129.2] [Reference Citation Analysis (2)] |
| 2. | Rees CJ, Belafsky PC. Laryngopharyngeal reflux: Current concepts in pathophysiology, diagnosis, and treatment. Int J Speech Lang Pathol. 2008;10:245-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Koufman JA, Aviv JE, Casiano RR, Shaw GY. Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg. 2002;127:32-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 439] [Cited by in RCA: 416] [Article Influence: 18.1] [Reference Citation Analysis (36)] |
| 4. | Gupta R, Sataloff RT. Laryngopharyngeal reflux: current concepts and questions. Curr Opin Otolaryngol Head Neck Surg. 2009;17:143-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Merati AL, Lim HJ, Ulualp SO, Toohill RJ. Meta-analysis of upper probe measurements in normal subjects and patients with laryngopharyngeal reflux. Ann Otol Rhinol Laryngol. 2005;114:177-182. [PubMed] |
| 6. | Hirano I, Richter JE. ACG practice guidelines: esophageal reflux testing. Am J Gastroenterol. 2007;102:668-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 233] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 7. | Ward EM, Devault KR, Bouras EP, Stark ME, Wolfsen HC, Davis DM, Nedrow SI, Achem SR. Successful oesophageal pH monitoring with a catheter-free system. Aliment Pharmacol Ther. 2004;19:449-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 82] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Cohen LB, Ladas SD, Vargo JJ, Paspatis GA, Bjorkman DJ, Van der Linden P, Axon AT, Axon AE, Bamias G, Despott E. Sedation in digestive endoscopy: the Athens international position statements. Aliment Pharmacol Ther. 2010;32:425-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Hazeldine S, Fritschi L, Forbes G. Predicting patient tolerance of endoscopy with conscious sedation. Scand J Gastroenterol. 2010;45:1248-1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Rattan S, Goyal RK. Identification and localization of opioid receptors in the opossum lower esophageal sphincter. J Pharmacol Exp Ther. 1983;224:391-397. [PubMed] |
| 11. | Hall AW, Moossa AR, Clark J, Cooley GR, Skinner DB. The effects of premedication drugs on the lower oesophageal high pressure zone and reflux status of rhesus monkeys and man. Gut. 1975;16:347-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 85] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Pandolfino JE. Bravo capsule pH monitoring. Am J Gastroenterol. 2005;100:8-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Xiao YL, Lin JK, Cheung TK, Wong NY, Hung IF, Wong BC, Peng S, Wang AJ, Chen MH. Reflux profile of Chinese gastroesophageal reflux disease patients with combined multichannel intraluminal impedance-pH monitoring. J Gastroenterol Hepatol. 2009;24:1113-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Belafsky PC, Postma GN, Koufman JA. Validity and reliability of the reflux symptom index (RSI). J Voice. 2002;16:274-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 927] [Cited by in RCA: 994] [Article Influence: 43.2] [Reference Citation Analysis (0)] |
| 17. | Belafsky PC, Postma GN, Koufman JA. The validity and reliability of the reflux finding score (RFS). Laryngoscope. 2001;111:1313-1317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 702] [Cited by in RCA: 686] [Article Influence: 28.6] [Reference Citation Analysis (1)] |
| 18. | Lazarescu A, Sifrim D. Ambulatory monitoring of GERD: current technology. Gastroenterol Clin North Am. 2008;37:793-805, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Bechtold ML, Holly JS, Thaler K, Marshall JB. Bravo (wireless) ambulatory esophageal pH monitoring: how do day 1 and day 2 results compare? World J Gastroenterol. 2007;13:4091-4095. [PubMed] |
| 20. | Bhat YM, McGrath KM, Bielefeldt K. Wireless esophageal pH monitoring: new technique means new questions. J Clin Gastroenterol. 2006;40:116-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Korrapati V, Babich JP, Balani A, Grendell JH, Kongara KR. Does deep sedation impact the results of 48 hours catheterless pH testing? World J Gastroenterol. 2011;17:1304-1307. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Pandolfino JE, Richter JE, Ours T, Guardino JM, Chapman J, Kahrilas PJ. Ambulatory esophageal pH monitoring using a wireless system. Am J Gastroenterol. 2003;98:740-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 344] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 23. | Prakash C, Clouse RE. Value of extended recording time with wireless pH monitoring in evaluating gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2005;3:329-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 125] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 24. | Ayazi S, Hagen JA, Zehetner J, Banki F, Augustin F, Ayazi A, DeMeester SR, Oh DS, Sohn HJ, Lipham JC. Day-to-day discrepancy in Bravo pH monitoring is related to the degree of deterioration of the lower esophageal sphincter and severity of reflux disease. Surg Endosc. 2011;25:2219-2223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Koufman JA. Laryngopharyngeal reflux is different from classic gastroesophageal reflux disease. Ear Nose Throat J. 2002;81:7-9. [PubMed] |