Published online Dec 28, 2012. doi: 10.3748/wjg.v18.i48.7314
Revised: November 25, 2011
Accepted: December 2, 2012
Published online: December 28, 2012
AIM: To investigate the feasibility and the effectiveness of ileoileostomy in the region adjacent to the ileocecal valve, which can retain the ileocecal valve in infants.
METHODS: This is a retrospective review of 48 patients who underwent ileoileostomy in the region adjacent to the ileocecal valve (group 1) and 34 patients who underwent ileocecal resections and ileotransversanastomosis (group 2). Patients were monitored for the time to flatus, resumption of eating, length of hospital stay after surgery, serum total bile acid, vitamin B12 and postoperative complications.
RESULTS: The time to flatus, time until resumption of eating and post-operative length of hospital stay showed no statistically significant differences between the two groups. Serum total bile acid and vitamin B12 were not significantly different between the two groups at post-operative day 1 and day 3, but were significantly decreased at 1 wk after operation in group 2. None of the patients died or suffered from stomal leak in these two groups. However, the incidence of diarrhea, intestinal infection, disturbance of acid-base balance and water-electrolytes in group 1 was lower than in group 2.
CONCLUSION: Ileoileostomy in the region adjacent to the ileocecal valve is safe and results in fewer complications than ileotransversanastomosis in infants.
- Citation: Jiang WW, Xu XQ, Geng QM, Zhang J, Chen H, Lv XF, Lu CG, Tang WB. Enteroenteroanastomosis near adjacent ileocecal valve in infants. World J Gastroenterol 2012; 18(48): 7314-7318
- URL: https://www.wjgnet.com/1007-9327/full/v18/i48/7314.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i48.7314
Ileocecal valve plays a very important role in the regulation of intestinal transit. It acts as a barrier to delay passage for small bowel contents and hence increases absorption. It also prevents reflux from the caecum into the ileum[1,2].
Anatomically, the terminal ileum has poor vascularization. The arterial supply of the terminal ileum in the region adjacent to the ileocecal valve comes from a single arch from the ileocolic artery. Therefore, conventional wisdom is, for a lesion involving the region of the ileum that is about 10-15 cm away from the ileocecal valve, a right hemicolectomy should be selected[3]. However, it was established in adults that the danger of incompetence of the anastomosis sutures near the blind gut was not greater than that in ileotransversanastomosis[4]. Moreover, long-term results in adult patients after resection of the small intestine with the enteroenteroanastomosis near the blind gut were better than in patients with resection of the ileocecal valve, regarding passage of the intestinal contents[4].
A previous study reported that an intact ileocecal valve was essential for better nutritive conditions in the newborn undergoing extensive small intestinal resection[5]. In non-tumoral lesions, preservation of the ileocaecal valve to retain its important function should be considered. The terminal ileum has a high incidence of intussusception, transmesenteric hernia, intestinal atresia and necrotizing enterocolitis. Our aim was to determine the feasibility of ileoileostomy in the region adjacent to the ileocecal valve and compare the rate of complications of ileoileostomy in the region adjacent to the ileocecal valve and ileocolostomy after ileocecal resections in infants.
This is a retrospective review of 48 patients who underwent ileoileostomy in the region adjacent to the ileocecal valve (group 1) and 34 patients who underwent ileocecal resections and ileocolostomy (group 2) in the Department of Pediatric Surgery, Nanjing Children’s Hospital, affiliated to Nanjing Medical University, between January 1, 2003 and May 3, 2011. In this study, all patients were without extensive ileal resection. We and our patients have established a long-term friendly relationship. The study was approved by the Ethics Committee of Nanjing Children’s Hospital, affiliated to Nanjing Medical University. Informed consent was obtained from all the guardians of the subjects.
The patients were categorized into two groups. Group 1 included 48 patients (26 males and 22 females aged 1 d to 10.6 mo; median age 4.8 mo) who underwent ileoileostomy in the region adjacent to the ileocecal valve. Causes of surgery included intussusception (7), transmesenteric hernia (11), intestinal atresia (5), necrotizing enterocolitis (17), mesenteric cyst (5) and duplication of intestine (3). Group 2 included 34 patients (20 males and 14 females aged 1 d to 9.1 mo; median age 4.2 mo) who underwent ileocecal resections and ileocolostomy. Causes of surgery included intussusception (7), transmesenteric hernia (10), intestinal atresia (4), necrotizing enterocolitis (9), mesenteric cyst (2) and duplication of intestine (2) (Table 1).
| Group 1 | Group 2 | |
| Patients | 48 (26 males and 22 females) | 34 (20 males and 14 females) |
| Age | 1 d to 10.6 mo | 1 d to 9.1 mo |
| (median age 4.8 mo) | (median age 4.2 mo) | |
| Primary diseases | Intussusception (7) | Intussusception (7) |
| Transmesenteric hernia (11) | Transmesenteric hernia (10) | |
| Intestinal atresia (5) | Intestinal atresia (4) | |
| Necrotizing enterocolitis (17) | Necrotizing enterocolitis (9) | |
| Mesenteric cyst (5) | Mesenteric cyst (2) | |
| Duplication of intestine (3) | Duplication of intestine (2) |
No patient died during this study. The patients with underlying pathology associated with chronic diarrhea such as short bowel syndrome were excluded. Patients were monitored in the time to flatus, resumption of eating and length of hospital stay after surgery, serum total bile acid, vitamin B12 and post-operative complications.
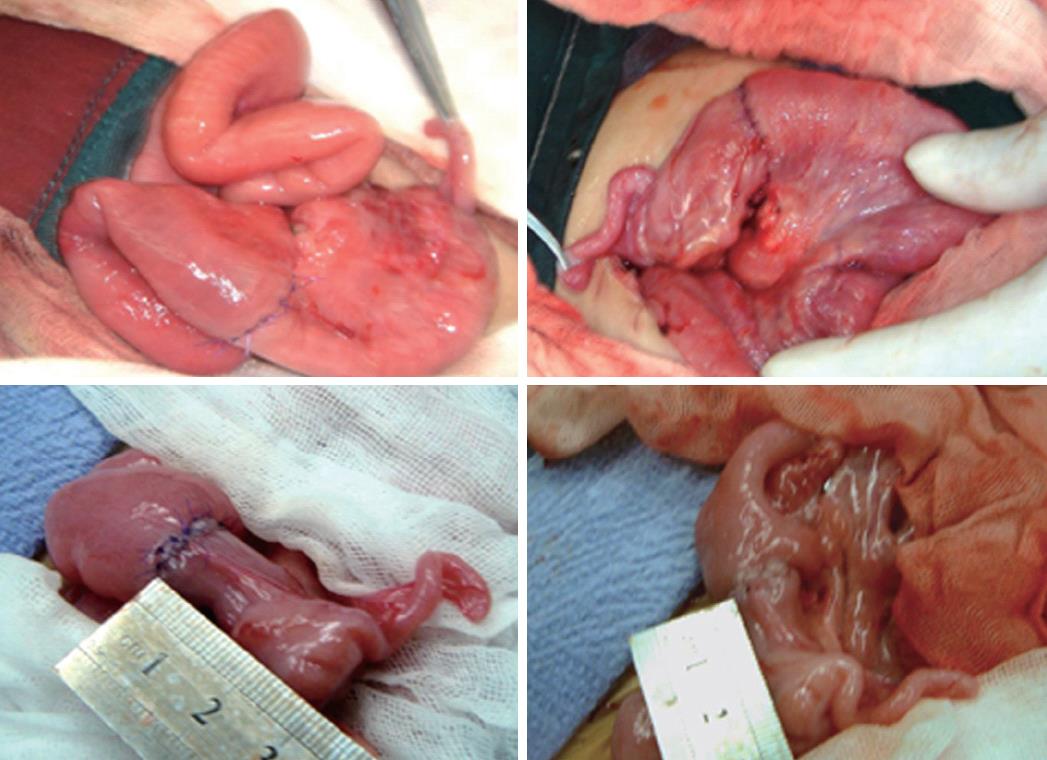
In brief, for group 1, the mesentery close to the bowel wall was dissociated and the ileocolic artery trunk was reserved. After resection of the lesions of the terminal ileum, pulsatile bleeding was visible in the two ends of the bowel. An ileoileostomy was then performed with 5-0 PDS (2-5 cm away from the ileocecal valve at a median distance of 3.5 cm) with no embed. The arteria ileocolica was reserved. No intestinal decompression was added (Figure 1).
In group 2, after resection of the terminal ileum, ileocecal junction and the ascending colon and part of the colon transversum, an ileocolostomy was performed with 5-0 PDS.
The lesion resulting in the bowel resection was purple or gray, the mesenteric vascular pulse and bowel peristalsis disappeared, and the intestinal wall was inelastic. The resected bowel was approximately 10-30 cm.
Statistical analysis was carried out using SPSS software, version 14.0 (SPSS Inc., Chicago, IL, United States). A Pearson Chi-square test was used to compare the complications found in the two groups. The time of flatus, resumption of eating and length of hospital stay after operation were expressed as mean ± SD. Parameters were analyzed by Student’s t test. For the above parameters, P < 0.05 was considered statistically significant.
The time to flatus, resumption of eating, and length of hospital stay after surgery showed no statistically significant differences between the two groups (Table 2).
| Time to flatus after surgery (d) | Time of resumption of eating after surgery (d) | Length of hospital stay after surgery (d) | |
| Group 1 | 2 ± 0.9 | 6 ± 0.4 | 8 ± 3.1 |
| Group 2 | 2 ± 0.7 | 5 ± 0.8 | 8 ± 2.5 |
After surgery, we advised nurses and parents to pay attention to the first flatus (anal exhaust) or defecation of the children, and recorded the time as well.
Resumption of eating was guided and determined by little liquid in gastrointestinal decompression, no yellow or green liquid in gastrointestinal decompression, no flatulence, and successful defecation.
Serum total bile acid and vitamin B12 (Table 3) showed no significant differences between the two groups at post-operative day 1 and day 3, but were significantly decreased at 1 wk after operation in group 2.
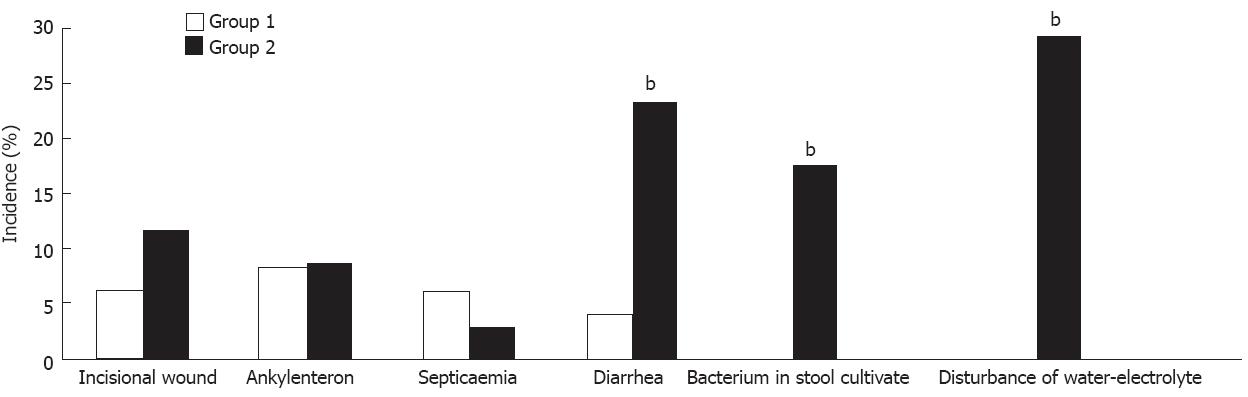
None of the patients died or suffered from stomal leak in these two groups. However, the incidence of diarrhea, bacterium in stool cultivante, and disturbance of water-electrolytes in group 1 was lower than in group 2 (Figure 2).
The present study showed that ileoileostomy in the region adjacent to the ileocecal valve was safe and was associated with fewer complications.
Previous studies have demonstrated that resection of the ileocaecal valve has several adverse effects. The ileocecal segment has been considered to possess a weak sphincteric action and functions in the flow of chyme and gut motility[1]. The ileocaecal valve prevents the reflux of chime, and thus prevents bacterial overgrowth from colonic bacterial flora in the small intestine. In the absence of an ileocecal valve, the colonic bacteria can reflux into the small intestine, resulting in infections of the small intestine and inflammation of the ileal mucosa[6-11]. Moreover, in the absence of the ileocecal valve, transit time was decreased and there was reduced exposure to the absorptive surface. Without adequate detention time in the small intestine, accelerated chime transport may lead to diarrhea, steatorrhea, malnutrition, dehydration, hypoalbuminemia and loss of minerals[12]. Dorney et al[5] found that the small bowel length required for survival was more than twofold when the ileocaecal valve was resected.
In animals and humans, bile salts and vitamin B12 have been shown to be major reclamation products from the ileum[13-16]. Further studies showed that the ileal absorption of bile salts is mediated by an apical sodium-dependent bile acid transporter located in the terminal ileum[17]. Previous studies have shown that patients with an ileal resection or disease of the distal ileum excreted bile salts in the feces significantly faster than healthy control subjects[18]. Moreover, patients who underwent massive ileal resections, especially ileocecal resections, showed malabsorption of bile acids[19,20]. Moreover, the anemia that occurred after ileocecal resection may have been due to deficiency in vitamin B12. As a result, reserving the ileal valve and terminal ileum might produce improved results.
Fernando et al[21] found that in most of the specimens from human cadavers analyzed in their study, the arterial supply of the ileocecal junction was from the ileocolic artery, superior mesenteric artery, and terminal ileal branches of the superior mesenteric artery. In their study, anastomosis in the ileocecal junction with small windows was observed in 38 (70%) cases, more than the cases for large windows. Moreover, Serova[4] demonstrated that the danger of incompetence of the anastomosis sutures in the region adjacent to the ileocecal valve was not higher than that in ileotransversanastomosis, and the immediate and long-term results in the enteroenteroanastomosis group were much better than in the group that had exclusion of the ileocecal segment. In our study, we demonstrated that after dissociating the mesentery close to the bowel wall and removing the part of the vascular network adjacent to the ileocecal junction, enteroenteroanastomosis near the blind gut was safe and no anastomotic leakage occurred.
Though there is a possibility of increasing the enteric cavity pressure of the ileocecal junction, we found that ileoileostomy only 2-5 cm away from the ileocecal valve is safe and effective in infants. This allowed a fluid diet to go through the ileal valve more easily than a solid diet. We also found that ileoileostomy in the region adjacent to the ileocecal valve was accompanied by fewer complications. As a result, the surgical method can be used clinically. Moreover, regarding the importance of the ileocecal valve, ileoileostomy in the region adjacent to the ileocecal valve might be helpful when a massive small bowel resection is necessary.
Ileocecal valve plays a very important role in the regulation of intestinal transit. It acts as a barrier to delay passage for small bowel contents and hence increases absorption. It also prevents reflux from the caecum into the ileum. In non-tumoral lesions, preservation of the ileocaecal valve to retain its important function should be considered.
The terminal ileum has poor vascularization. The arterial supply of the terminal ileum in the region adjacent to the ileocecal valve comes from a single arch from the ileocolic artery. This study focuses on the feasibility of ileoileostomy in the region adjacent to the ileocecal valve and the complications of ileoileostomy in the region adjacent to the ileocecal valve.
Though there is a possibility of increasing the enteric cavity pressure of the ileocecal junction, the authors found that ileoileostomy only 2-5 cm away from the ileocecal valve is safe and effective in infants. This allowed a fluid diet to go through the ileal valve more easily than a solid diet. The authors also found that ileoileostomy in the region adjacent to the ileocecal valve was accompanied by fewer complications.
Enteroenteroanastomosis near the adjacent ileocecal valve can be used clinically. Moreover, regarding the importance of the ileocecal valve, ileoileostomy in the region adjacent to the ileocecal valve might be helpful when a massive small bowel resection is necessary.
The presented paper is of some scientific interest and well-written.
Peer reviewer: Dr. Stefan Wirth, Professor, Children’s Hospital, Heusnerstt. 40, 42349 Wuppertal, Germany
S- Editor Cheng JX L- Editor Ma JY E- Editor Li JY
| 1. | Malbert CH. The ileocolonic sphincter. Neurogastroenterol Motil. 2005;17 Suppl 1:41-49. [PubMed] |
| 2. | Shafik AA, Ahmed IA, Shafik A, Wahdan M, Asaad S, El Neizamy E. Ileocecal junction: anatomic, histologic, radiologic and endoscopic studies with special reference to its antireflux mechanism. Surg Radiol Anat. 2011;33:249-256. [PubMed] |
| 3. | Zhong SZ. Clinical Anatomy. Beijing: People's Medical Publishing House 1998; 366-367. |
| 4. | Serova LS. Possibilities of forming enteroenteroanastomosis near the cecum. Vestn Khir Im I I Grek. 1988;140:52-55. [PubMed] |
| 5. | Dorney SF, Ament ME, Berquist WE, Vargas JH, Hassall E. Improved survival in very short small bowel of infancy with use of long-term parenteral nutrition. J Pediatr. 1985;107:521-525. [PubMed] |
| 6. | Ecker KW, Pistorius G, Harbauer G, Feifel G. Bacterial clearance of the terminal ileum in relation to the ileocolic connection. Zentralbl Chir. 1995;120:336-342. [PubMed] |
| 7. | Richardson JD, Griffen WO. Ileocecal valve substitutes as bacteriologic barriers. Am J Surg. 1972;123:149-153. [PubMed] |
| 8. | Folaranmi S, Rakoczy G, Bruce J, Humphrey G, Bowen J, Morabito A, Kapur P, Morecroft J, Craigie R, Cserni T. Ileocaecal valve: how important is it? Pediatr Surg Int. 2011;27:613-615. [PubMed] |
| 9. | Singleton AO, Kurrus FD, Donegan DW. The increasing of absorption following massive resections of bowel by means of antiperistaltic bowel segments as measured by radioiodine fat absorption studies. Ann Surg. 1961;154:130-132. [PubMed] |
| 10. | Stahlgren LH, Umana G, Roy R, Donnelly J. A study of intestinal absorption in dogs following massive small intestinal resection and insertion of an antiperistaltic segment. Ann Surg. 1962;156:483-492. [PubMed] |
| 11. | Richardson JD, Griffen WO. Importance of the ileocecal valve in intestinal absorption. Texas Rep Biol Med. 1970;28:408-409. |
| 12. | Quigley EM, Thompson JS. Effects of artificial ileocolonic sphincter on motility in intestinal remnant following subtotal small intestinal resection in the dog. Dig Dis Sci. 1994;39:1222-1229. [PubMed] |
| 13. | Song SM, Bae KW, Yoon HS, Im HJ, Seo JJ. A case of anemia caused by combined vitamin B12 and iron deficiency manifesting as short stature and delayed puberty. Korean J Pediatr. 2010;53:661-665. [PubMed] |
| 14. | Medeiros AC, Filho IA, Medeiros VB, Pinheiro LA, Freire FH, Azevedo IM, Brandão-Neto J. Comparing reconstruction with ileocecal graft to jejunal interposition pouch after total gastrectomy in rats. J Invest Surg. 2007;20:41-48. [PubMed] |
| 15. | Iwanaka T, Hashizume K, Kawarasaki H, Tanaka K, Kanamori Y, Utsuki T, Obana K, Uno K, Sugiyama M, Tsuchida Y. Ileocecal resection in neonates and infants: a follow-up study. J Pediatr Surg. 1993;28:110-112. [PubMed] |
| 16. | Westergaard H. Bile Acid malabsorption. Curr Treat Options Gastroenterol. 2007;10:28-33. [PubMed] |
| 17. | Meihoff WE, Kern F. Bile salt malabsorption in regional ileitis, ileal resection and mannitol-induced diarrhea. J Clin Invest. 1968;47:261-267. [PubMed] |
| 18. | Hofmann AF, Grundy SM. Abnormal bile salt metabolism in a patient with extensive lower intestinal resection. Clin Res. 1965;13:254. |
| 19. | Hofmann AF. Bile acid malabsorption caused by ileal resection. Arch Intern Med. 1972;130:597-605. [PubMed] |
| 20. | Aldini R, Roda A, Festi D, Sama C, Mazzella G, Bazzoli F, Morselli AM, Roda E, Barbara L. Bile acid malabsorption and bile acid diarrhea in intestinal resection. Dig Dis Sci. 1982;27:495-502. [PubMed] |