Published online Nov 21, 2012. doi: 10.3748/wjg.v18.i43.6216
Revised: July 2, 2012
Accepted: July 9, 2012
Published online: November 21, 2012
Barrett’s esophagus is a condition resulting from chronic gastro-esophageal reflux disease with a documented risk of esophageal adenocarcinoma. Current strategies for improved survival in patients with Barrett's adenocarcinoma focus on detection of dysplasia. This can be obtained by screening programs in high-risk cohorts of patients and/or endoscopic biopsy surveillance of patients with known Barrett’s esophagus (BE). Several therapies have been developed in attempts to reverse BE and reduce cancer risk. Aggressive medical management of acid reflux, lifestyle modifications, antireflux surgery, and endoscopic treatments have been recommended for many patients with BE. Whether these interventions are cost-effective or reduce mortality from esophageal cancer remains controversial. Current treatment requires combinations of endoscopic mucosal resection techniques to eliminate visible lesions followed by ablation of residual metaplastic tissue. Esophagectomy is currently indicated in multifocal high-grade neoplasia or mucosal Barrett’s carcinoma which cannot be managed by endoscopic approach.
- Citation: Palma GDD. Management strategies of Barrett's esophagus. World J Gastroenterol 2012; 18(43): 6216-6225
- URL: https://www.wjgnet.com/1007-9327/full/v18/i43/6216.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i43.6216
Barrett’s esophagus (BE) is a condition resulting from chronic gastro-esophageal reflux disease (GERD). The clinical importance of the definition of BE is that it should identify a lesion documented to be at risk of esophageal adenocarcinoma.
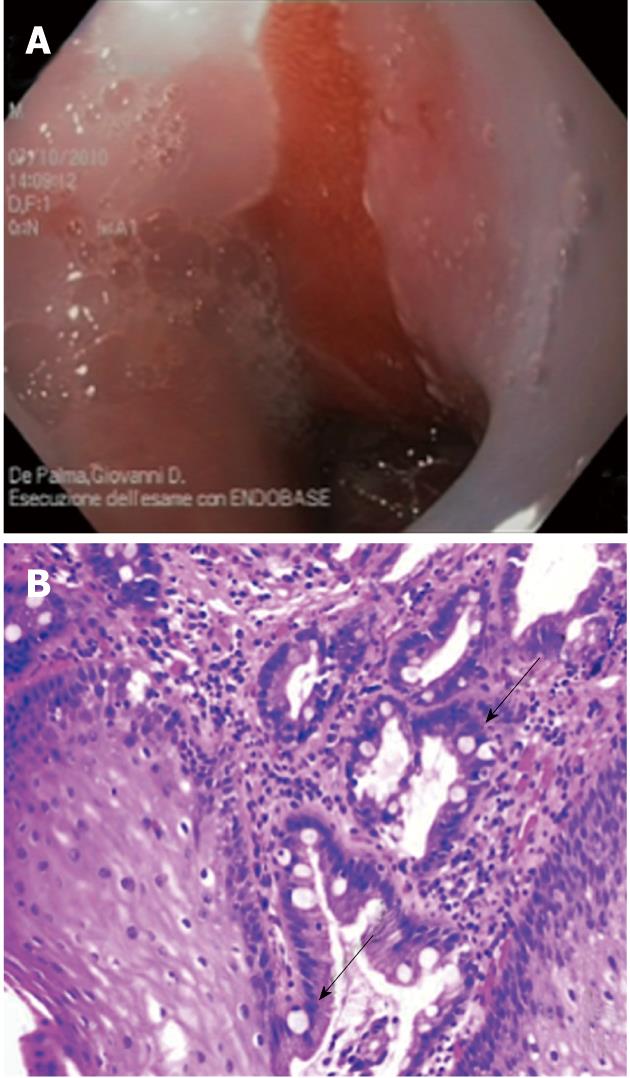
Presently, the diagnosis of BE is based on a combination of endoscopic and histologic criteria[1,2]. The diagnosis of BE is established when intestinal metaplasia (IM) is found in biopsy specimens obtained from salmon-colored mucosa in the distal esophagus proximal to the gastro-esophageal junction (Figure 1).
The diagnosis of BE requires systematic biopsy of the abnormal-appearing esophageal mucosa to document IM and to detect dysplasia[1]. The “Seattle” protocol with random four-quadrant biopsies taken at 1-2-cm intervals along the endoscopically visible BE is the current recommended procedure in guidelines for the detection of dysplasia in patients with established BE[3-6].
BE is currently graded with use of the Prague circumference and maximum criteria, which is a standardized, validated system based on the circumferential and maximal extent of the columnar-lined esophagus[7-9].
BE develops in in approximately 5% to 15% of patients with gastro-esophageal reflux undergoing endoscopic evaluation and in 1% to 2% of unselected population undergoing endoscopy[10-14]. Evidence from one case series suggests that at least 60% of patients with BE develop the disease as a result of chronic reflux; other condition of mucosal inflammation of the lower esophagus, such as mucosal damage by chemotherapy, non-steroidal anti-inflammatory drugs, and viral infections are associated with the development of BE in about 1% of cases respectively[15-19].
BE is associated with an increased risk of adenocarcinoma of the esophagus. Patients with BE are about 40 times more likely to have esophageal adenocarcinoma (EAC) than those without IM. The risk for an individual patient with BE has been estimated to range from 1 in 50 to 1 in 200 patient-years, or roughly 0.5% per year. Recent large cohort studies suggest the rate of progression is 0.1%-0.3% per year[20-23].
Barrett’s adenocarcinoma is considered a multistep process evolving from normal squamous mucosa to metaplasia to dysplasia to carcinoma. Why such a progression occurs, who is at risk, and what promotes these changes remain unclear. Clinical and demographic factors, such as, age, male gender, longer duration and increased frequency of GERD symptoms, length of BE segment are associated with modestly increased odds of progression to EAC in some studies[24-29]. Biomarkers[30-33] such as aneuploidy and p53 loss have been recently associated with increased risk of progression to high-grade dysplasia (HGD) and/or EAC[34-37].
At present, the strongest known predictor of cancer risk in the setting of BE is the degree of dysplasia. Subjects with no dysplasia have extremely low cancer rates for the five years following the index endoscopy. Conversely, subjects with HGD have rates reported as high as 10% per year[38-40].
It is of paramount importance that the correct diagnosis is established. In many instances, especially in the presence of severe inflammation, there is an inter-observer disagreement on the diagnosis and grading of dysplasia. All biopsies with suspected dysplasia should be reviewed by a second “expert” pathologist[41-43].
Several therapies have been developed in attempts to reverse BE and reduce cancer risk. Aggressive medical management of acid reflux, lifestyle modifications, antireflux surgery[44-49], and endoscopic treatments[50-52] have been recommended for many patients with BE. Whether these interventions are cost-effective or reduce mortality from esophageal cancer remains controversial.
Current strategies for improved survival in patients with Barrett’s adenocarcinoma focus on detection of dysplasia. This can be obtained by screening programs in high-risk cohorts of patients and/or endoscopic biopsy surveillance of patients with known BE.
There is inadequate evidence of benefit to recommend endoscopic screening for BE in the general population of patients with GERD who do not have risk factors[53-58]. Well-established risk factors for BE include age older than 50 years, male sex, white race, chronic GERD[1-5], hiatal hernia[59], elevated body mass index, and intra-abdominal distribution of body fat[60,61] . The risk factors can be used to determine the threshold for endoscopy in patients with GERD to screen for the presence of BE[2].
Endoscopic surveillance for patients with BE is recommended to identify curable neoplasia. Survey data indicate that although surveillance is widely practiced, there is marked variability in the technique and interval of surveillance because practice guidelines are not widely followed (Table 1)[62].
| ACG | ASGE | AGA | BSG | |
| No-dysplasia | Two esophageal examination with biopsy within 1 yr and follow up with endoscopy every 3 yr | Two consecutive esophageal examination with biopsy within 1 yr and follow up with endoscopy every 3 yr | Assess within 1 yr and if no dysplasia, defer for 5 yr or until cancer therapy is not possible of life expectancy is limited | Surveillance every 2 yr, if appropriate |
| Indefinite | - | Repeat biopsy after 8 wk of acid suppression, if evidence of acute inflammation due to gastro-esophageal acid reflux | - | Assess with extensive biopsies after course of proton pump inhibitors and return to routine surveillance, if no definite dysplasia at 6 mo |
| LGD | Treat based on highest grade of dysplasia seen on two esophageal examinations within 6 mo, with pathologist’s confirmation, and follow up with endoscopy every year until dysplasia is absent on two subsequent examinations | Follow up after 6 mo with concentrated biopsies in area of dysplasia; follow up every 12 mo if dysplasia persists | Assess in 1 yr and re-examine every year if dysplasia is confirmed by two pathologists (if there is disagreement about the presence of dysplasia then re-examine in 2 yr) | Extensive biopsy after intensive acid suppression for 8-12 wk; surveillance every 6 mo if dysplasia persist; surveillance intervals of 2-3 yr if regression occurs on two sequential examinations |
| HGD | Document any mucosal irregularities, repeat esophageal examination with biopsy within 3 mo, with pathologist’s confirmation, to eliminate the possibility of cancer; follow up with endoscopic mucosal resection in the case of any mucosal irregularity; then intensive endoscopic surveillance every 3 mo or an intervention, such as esophagectomy or ablation, in the case of flat mucosa | Diagnosis should be confirmed by a pathologist; surgical candidates can choose to have a surgery or endoscopic therapy; follow up patients who choose surveillance every 3 mo for 1 yr with several large biopsies every 1 cm along esophagus; after 1 yr without cancer detection, surveillance duration can be lengthened, provided dysplastic changes are absent on two subsequent examinations | Diagnosis should be confirmed by two pathologists; patients should be treated with surgical resection or endoscopic therapy; surveillance can be offered provided follow up with endoscopy is every 3 mo with a minimum of eight biopsies every 2 cm along esophagus | Esophagectomy recommended if changes persist after intensive acid suppression, if confirmed by two pathologists, and if patient considered fit for surgery; if unfit for surgery, use endoscopic ablation or mucosal resection |
Endoscopic imaging for the detection of dysplasia and early cancer: Endoscopy with multiple systematic biopsies (the “Seattle” protocol) is needed for the detection of dysplasia or adenocarcinoma for the surveillance of BE. This approach, requiring a large number of biopsies, is time consuming and has several limitations, including sampling error and inconsistent histological interpretation[2-6].
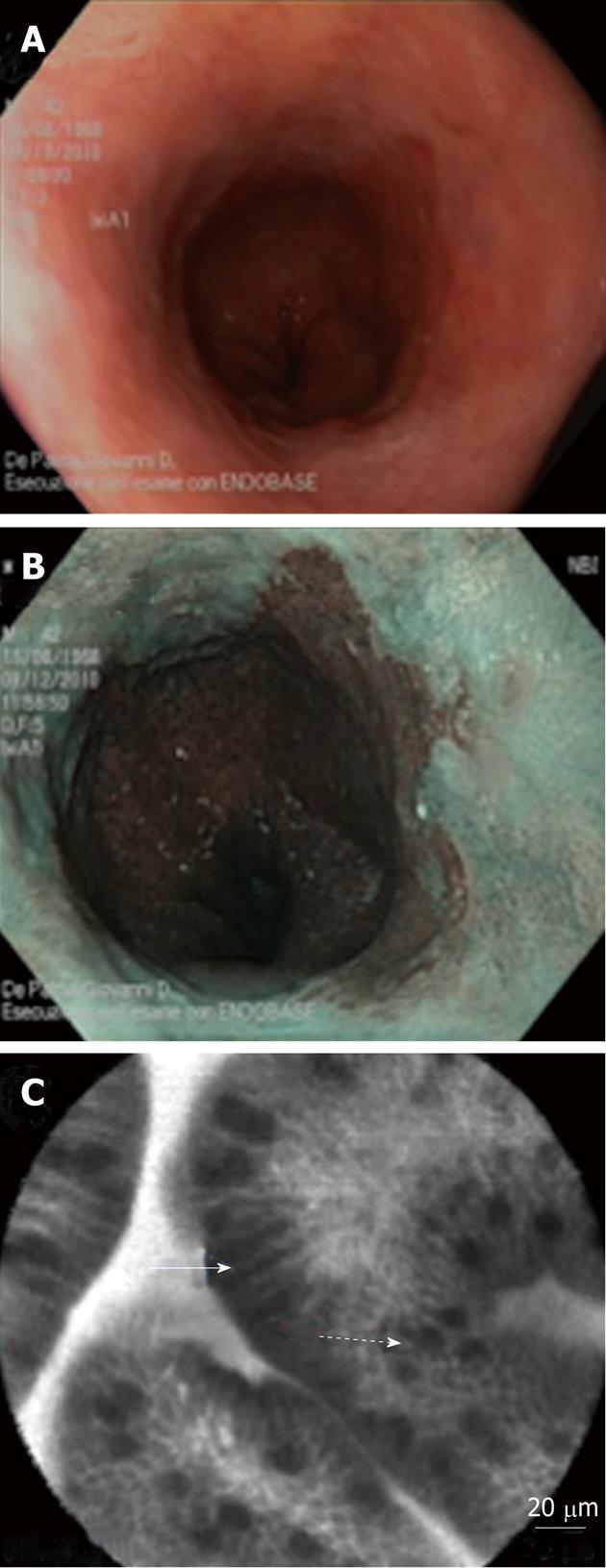
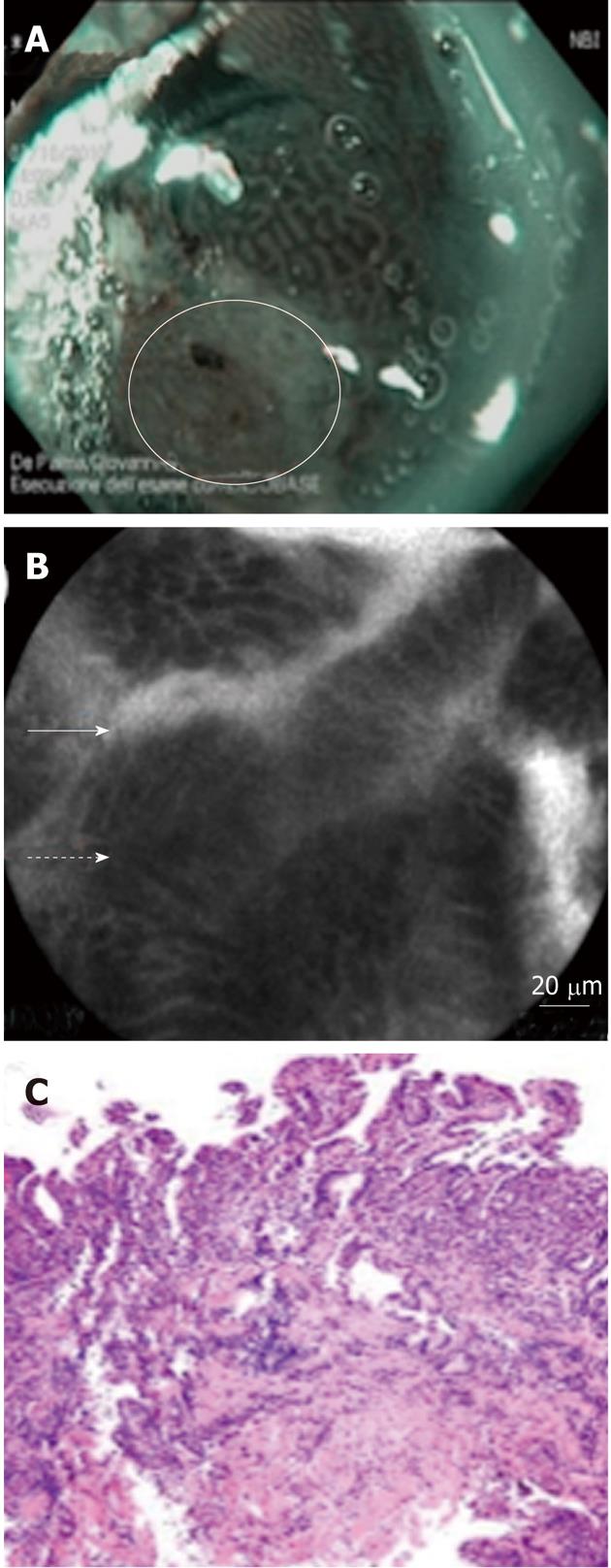
Several endoscopic imaging techniques to improve the accuracy of endoscopic diagnosis, have been developed and tested recently, with variable results[63-67]. Enhanced optical imaging techniques may improve the efficiency and accuracy of endoscopic surveillance[68-72]. Enhanced techniques can generally be categorized as broad-field (red-flag) techniques, such as high-definition/high-resolution white-light endoscopy (HD-WLE) and narrow-band imaging (NBI)[73-75], and focal techniques, such as confocal laser endomicroscopy (CLE)[76-80]. The broad-field techniques are good for providing an overview of the entire BE segment, and point out an area of interest, whereas focal techniques can provide greater detail of the area of interest (Figures 2 and 3)[81-85].
Recent reports demonstrated that, in BE patients undergoing surveillance endoscopy, CLE imaging with targeted biopsies significantly improved the yield of biopsies for dysplasia compared with standard endoscopy with random biopsies when CLE imaging is conducted on suspect areas evidenced with both HD-WLE and NBI. Similarly, CLE was useful as a tool to identify non-dysplastic BE, and hence potentially to reduce the number of biopsies needed[86-89].
Acid suppressive therapy, specifically proton pump inhibitors (PPIs), has been shown to improve symptoms and to heal and prevent relapse of erosive esophagitis in patients with BE[4,90,91]. Evidence to support use of PPIs, in patients with BE solely to reduce risk of progression to dysplasia or cancer is indirect and has not been proven in a long-term controlled trial[92-96]. Epidemiologic data suggest a lower risk of progression in PPI users. There is also some evidence to suggest that long-term therapy may induce regression of IM and promote the development of squamous islands[97-99].
There is epidemiologic and experimental evidence to suggest that chemoprevention using non-steroidal anti-inflammatory drugs, aspirin[100-104], and selective cyclooxygenase-2 inhibitors[105-107] may reduce the risk of cancer in BE patients. However, human trials to date has not proved that these treatments are associated with a lower risk for neoplastic progression[108].
The A phase III, randomised study of aspirin and esoprazole chemoprevention in Barrett’s metaplasia trial currently underway is seeking to determine the effects of high- and low-dose proton pump inhibitor therapy with and without low-dose aspirin as BE chemoprevention[109,110].
Endoscopic treatment is focused on destruction of the existing metaplastic-dysplastic tissue using different modalities that eliminate the mucosa. The theory behind endoscopic treatment is that the injury of the metaplastic-dysplastic BE combined with vigorous acid suppression or with antireflux surgery would lead to reversion of the BE to squamous epithelium and reduce the risk of progression to cancer[111-115].
Endoscopic treatment modalities include endoscopic resection techniques such as endoscopic mucosal resection and endoscopic submucosal dissection[114] and endoscopic ablation therapy[116,117], such as argon plasma coagulation (APC)[118,119], laser ablation, photodynamic therapy (PDT)[120], radiofrequency ablation (RFA)[121,122], and cryotherapy[123-127].
Current treatment requires combinations of mucosal resection techniques to eliminate visible lesions followed by ablation of residual metaplastic tissue. Endoscopic resection of focal lesions is currently the only method to accurately and reliably determine the depth of invasion of a superficial lesion since it is the only endoscopic technique that provides histology.
Several studies have reported on a variety of ablation methods and have demonstrated difficulty in achieving complete eradication of BE. Thermal ablative modalities, such as APC, and laser therapy suffer from several pitfalls including a not homogeneous ablation of the mucosa and inconsistent depth of tissue penetration causing that some glands can persist under the neo-squamous epithelium[128,129].
At present, after the areas of mucosal abnormality are removed, ablation of the residual Barrett’s mucosa is most commonly performed with PDT or RFA. Photodynamic therapy has been proved to be effective for dysplasia, with a success rate of > 90%. However, following this treatment, there is a high rate of complication and side effects, mainly characterized by strictures and photosensitivity[2,120,130-132]. Radiofrequency ablation is associated with fewer complications since it has a limited depth of injury, although stricture formation is approximately 6% in some prospective series[133-137]. After RFA, complete eradication of dysplasia was reported in > 90% of patients with LGD and > 80% of patients with HGD, 1 year after the initial treatment. After 3 years, complete eradication of dysplasia and complete eradication of IM was reported in 98% and 91% of patients, respectively. At 5 years follow up, complete eradication of IM was demonstrated in 92% of the patients[138-142].
Buried metaplasia is reported less frequently after RFA (< 1%) than after other different ablative endoscopic therapies, including PDT. However RFA is a relatively new procedure and, therefore, available studies on RFA describe only brief follow-up intervals[143,144].
Because of the esophagus remains after endoscopic therapy, surveillance endoscopy at regular intervals, is necessary, even after complete ablation of BE has been accomplished.
As development of BE is based on gastro-esophageal reflux, a potential concept would be to stop reflux by anti-reflux surgery and thereby interrupt the mechanisms of malignant degeneration. Patients who are appropriate surgical candidates may elect anti-reflux surgery[145-148]. Fundoplication effectively controls reflux symptoms in most patients[149,150]. Surgical control of reflux disease, however, has not been found to be associated with a decrease in the incidence of esophageal cancer[151-154].
Before the advent of endoscopic therapies, esophagectomy was the primary treatment option for patients with HGD.
Esophagectomy offers the most definite treatment in patients with BE with HGD (in particular in patients with multifocal HGD) since it eliminates all of the Barrett’s epithelium preventing the risk of progression. In patients with HGD, a benefit of esophagectomy includes the treatment of an occult carcinoma (surgical series summarizing the incidence of occult adenocarcinoma, in patients with the preoperative diagnosis of HGD in resected series show an incidence ranging from 0% to 73%)[155-159].
The standard surgical resection in most patients includes a total esophagectomy with a transhiatal or transthoracic approach, and reconstruction with gastric pull-up or tubularized gastric conduit and the anastomosis performed in the neck or the high chest. In some cases esophageal resection could be performed minimally invasively. Limited vagal-sparing surgery like esophageal stripping or Merendino’s operation is currently indicated in multifocal high-grade neoplasia or mucosal Barrett’s carcinoma which cannot be managed by endoscopic approach. Strong consideration should be given for the performance of surgery in a high-volume hospital, by a specialty-trained surgeon with a large-volume esophageal practice[160-162].
BE is a premalignant condition, with dysplasia usually preceding the development of adenocarcinoma. Patients with chronic reflux, especially white males, have the highest risk. Reducing reflux either medically or surgically may diminish the occurrence and/or progression of disease. Management of BE may vary from essentially a surveillance strategy to highly invasive esophagectomy.
Several therapies have been developed in attempts to reverse BE and reduce cancer risk, such as medical management of acid reflux, antireflux surgery, and endoscopic treatments. Whether these interventions are cost-effective or reduce mortality from esophageal cancer remains controversial. Endoscopic mucosal ablation techniques show promise as emerging therapeutic options. Current treatment requires combinations of endoscopic mucosal resection techniques to eliminate visible lesions followed by ablation of residual metaplastic tissue.
Esophagectomy is currently indicated in multifocal high-grade neoplasia or mucosal Barrett’s carcinoma which cannot be managed by endoscopic approach.
Peer reviewers: Dr. Julian Abrams, Department of Medicine, Columbia University Medical Center, 622 W 168th Street, PH 20-303, New York, NY 10032, United States; Dr. Lesley Ann Anderson, Department of Epidemiology and Public Health, Queen’s University Belfast, Mulhouse Building Grosvenor Road, Belfast BT12 6BJ, United Kingdom
S- Editor Gou SX L- Editor A E- Editor Xiong L
| 1. | Sampliner RE. Updated guidelines for the diagnosis, surveillance, and therapy of Barrett's esophagus. Am J Gastroenterol. 2002;97:1888-1895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 567] [Cited by in RCA: 504] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 2. | Spechler SJ, Sharma P, Souza RF, Inadomi JM, Shaheen NJ. American Gastroenterological Association medical position statement on the management of Barrett's esophagus. Gastroenterology. 2011;140:1084-1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 383] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 3. | Wang KK, Sampliner RE. Updated guidelines 2008 for the diagnosis, surveillance and therapy of Barrett's esophagus. Am J Gastroenterol. 2008;103:788-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 850] [Cited by in RCA: 786] [Article Influence: 46.2] [Reference Citation Analysis (1)] |
| 4. | Sharma P, McQuaid K, Dent J, Fennerty MB, Sampliner R, Spechler S, Cameron A, Corley D, Falk G, Goldblum J. A critical review of the diagnosis and management of Barrett's esophagus: the AGA Chicago Workshop. Gastroenterology. 2004;127:310-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 389] [Cited by in RCA: 351] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 5. | Hirota WK, Zuckerman MJ, Adler DG, Davila RE, Egan J, Leighton JA, Qureshi WA, Rajan E, Fanelli R, Wheeler-Harbaugh J. ASGE guideline: the role of endoscopy in the surveillance of premalignant conditions of the upper GI tract. Gastrointest Endosc. 2006;63:570-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 315] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 6. | Reid BJ, Blount PL, Feng Z, Levine DS. Optimizing endoscopic biopsy detection of early cancers in Barrett's high-grade dysplasia. Am J Gastroenterol. 2000;95:3089-3096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Anand O, Wani S, Sharma P. When and how to grade Barrett's columnar metaplasia: the Prague system. Best Pract Res Clin Gastroenterol. 2008;22:661-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Sharma P, Dent J, Armstrong D, Bergman JJ, Gossner L, Hoshihara Y, Jankowski JA, Junghard O, Lundell L, Tytgat GN. The development and validation of an endoscopic grading system for Barrett's esophagus: the Prague C & amp; M criteria. Gastroenterology. 2006;131:1392-1399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 731] [Cited by in RCA: 716] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 9. | Vahabzadeh B, Seetharam AB, Cook MB, Wani S, Rastogi A, Bansal A, Early DS, Sharma P. Validation of the Prague C & amp; M criteria for the endoscopic grading of Barrett's esophagus by gastroenterology trainees: a multicenter study. Gastrointest Endosc. 2012;75:236-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Falk GW. Barrett's esophagus. Gastroenterology. 2002;122:1569-1591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 252] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 11. | Csendes A, Smok G, Quiroz J, Burdiles P, Rojas J, Castro C, Henríquez A. Clinical, endoscopic, and functional studies in 408 patients with Barrett's esophagus, compared to 174 cases of intestinal metaplasia of the cardia. Am J Gastroenterol. 2002;97:554-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 49] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Lagergren J, Bergström R, Lindgren A, Nyrén O. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340:825-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2115] [Cited by in RCA: 2028] [Article Influence: 78.0] [Reference Citation Analysis (0)] |
| 13. | Solaymani-Dodaran M, Logan RF, West J, Card T, Coupland C. Risk of oesophageal cancer in Barrett's oesophagus and gastro-oesophageal reflux. Gut. 2004;53:1070-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 208] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 14. | Cameron AJ. Epidemiology of columnar-lined esophagus and adenocarcinoma. Gastroenterol Clin North Am. 1997;26:487-494. [PubMed] |
| 15. | Jankowski JA, Harrison RF, Perry I, Balkwill F, Tselepis C. Barrett's metaplasia. Lancet. 2000;356:2079-2085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 224] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 17. | Ronkainen J, Aro P, Storskrubb T, Johansson SE, Lind T, Bolling-Sternevald E, Vieth M, Stolte M, Talley NJ, Agréus L. Prevalence of Barrett's esophagus in the general population: an endoscopic study. Gastroenterology. 2005;129:1825-1831. [PubMed] |
| 18. | Qumseya BJ, Wolfsen CL, Wolfsen HC. Reflux disease and Barrett's esophagus. Endoscopy. 2011;43:962-965. [PubMed] |
| 19. | Tytgat GN. Recent developments in gastroesophageal reflux disease and Barrett's esophagus: ANNO 2012. J Dig Dis. 2012;13:291-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Hvid-Jensen F, Pedersen L, Drewes AM, Sørensen HT, Funch-Jensen P. Incidence of adenocarcinoma among patients with Barrett's esophagus. N Engl J Med. 2011;365:1375-1383. [PubMed] |
| 21. | Bhat S, Coleman HG, Yousef F, Johnston BT, McManus DT, Gavin AT, Murray LJ. Risk of malignant progression in Barrett's esophagus patients: results from a large population-based study. J Natl Cancer Inst. 2011;103:1049-1057. [PubMed] |
| 22. | Wani S. Population-based estimates of cancer and mortality in Barrett's esophagus: implications for the future. Clin Gastroenterol Hepatol. 2011;9:723-724. [PubMed] |
| 23. | Conteduca V, Sansonno D, Ingravallo G, Marangi S, Russi S, Lauletta G, Dammacco F. Barrett's esophagus and esophageal cancer: an overview. Int J Oncol. 2012;41:414-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 24. | Spechler SJ. The natural history of dysplasia and cancer in esophagitis and Barrett esophagus. J Clin Gastroenterol. 2003;36:S2-S5; discussion S26-S28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Wiseman EF, Ang YS. Risk factors for neoplastic progression in Barrett's esophagus. World J Gastroenterol. 2011;17:3672-3683. [PubMed] |
| 26. | Bobryshev YV, Killingsworth MC, Lord RV. Structural alterations of the mucosa stroma in the Barrett's esophagus metaplasia-dysplasia-adenocarcinoma sequence. J Gastroenterol Hepatol. 2012;27:1498-1504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Wani S, Falk GW, Post J, Yerian L, Hall M, Wang A, Gupta N, Gaddam S, Singh M, Singh V. Risk factors for progression of low-grade dysplasia in patients with Barrett's esophagus. Gastroenterology. 2011;141:1179-1186, 1186.e1. [PubMed] |
| 28. | Sikkema M, Looman CW, Steyerberg EW, Kerkhof M, Kastelein F, van Dekken H, van Vuuren AJ, Bode WA, van der Valk H, Ouwendijk RJ. Predictors for neoplastic progression in patients with Barrett's Esophagus: a prospective cohort study. Am J Gastroenterol. 2011;106:1231-1238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 29. | di Pietro M, O'Donovan M, Fitzgerald RC. Where is the truth when it comes to cancer risk in Barrett's esophagus? Gastroenterology. 2012;142:1245-1247. [PubMed] |
| 30. | Souza RF, Meltzer SJ. The molecular basis for carcinogenesis in metaplastic columnar-lined esophagus. Gastroenterol Clin North Am. 1997;26:583-597. [PubMed] |
| 31. | Souza RF. The molecular basis of carcinogenesis in Barrett's esophagus. J Gastrointest Surg. 2010;14:937-940. [PubMed] |
| 32. | Moyes LH, Going JJ. Still waiting for predictive biomarkers in Barrett's oesophagus. J Clin Pathol. 2011;64:742-750. [PubMed] |
| 33. | Chen H, Fang Y, Tevebaugh W, Orlando RC, Shaheen NJ, Chen X. Molecular mechanisms of Barrett's esophagus. Dig Dis Sci. 2011;56:3405-3420. [PubMed] |
| 34. | Coban S, Ormeci N, Savas B, Ekiz F, Ensari A, Kuzu I, Palabiykoglu M. Evaluation of Barrett's esophagus with CK7, CK20, p53, Ki67, and cyclooxygenase expressions using chromoendoscopical examination. Dis Esophagus. 2012;May 16 [Epub ahead of print]. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Rabinovitch PS, Longton G, Blount PL, Levine DS, Reid BJ. Predictors of progression in Barrett's esophagus III: baseline flow cytometric variables. Am J Gastroenterol. 2001;96:3071-3083. [PubMed] |
| 36. | Reid BJ, Prevo LJ, Galipeau PC, Sanchez CA, Longton G, Levine DS, Blount PL, Rabinovitch PS. Predictors of progression in Barrett's esophagus II: baseline 17p (p53) loss of heterozygosity identifies a patient subset at increased risk for neoplastic progression. Am J Gastroenterol. 2001;96:2839-2848. [PubMed] |
| 37. | Babar M, Ryan AW, Anderson LA, Segurado R, Turner G, Murray LJ, Murphy SJ, Johnston BT, Comber H, Reynolds JV. Genes of the Interleukin-18 Pathway Are Associated With Susceptibility to Barrett's Esophagus and Esophageal Adenocarcinoma. Am J Gastroenterol. 2012;107:1331-1341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 38. | Weston AP, Sharma P, Topalovski M, Richards R, Cherian R, Dixon A. Long-term follow-up of Barrett's high-grade dysplasia. Am J Gastroenterol. 2000;95:1888-1893. [PubMed] |
| 39. | Miros M, Kerlin P, Walker N. Only patients with dysplasia progress to adenocarcinoma in Barrett's oesophagus. Gut. 1991;32:1441-1446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 185] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 40. | Desai TK, Krishnan K, Samala N, Singh J, Cluley J, Perla S, Howden CW. The incidence of oesophageal adenocarcinoma in non-dysplastic Barrett's oesophagus: a meta-analysis. Gut. 2012;61:970-976. [PubMed] |
| 41. | Yantiss RK. Diagnostic challenges in the pathologic evaluation of Barrett esophagus. Arch Pathol Lab Med. 2010;134:1589-1600. [PubMed] |
| 42. | Wani S, Mathur S, Sharma P. How to manage a Barrett's esophagus patient with low-grade dysplasia. Clin Gastroenterol Hepatol. 2009;7:27-32. [PubMed] |
| 43. | Montgomery E, Bronner MP, Goldblum JR, Greenson JK, Haber MM, Hart J, Lamps LW, Lauwers GY, Lazenby AJ, Lewin DN. Reproducibility of the diagnosis of dysplasia in Barrett esophagus: a reaffirmation. Hum Pathol. 2001;32:368-378. [PubMed] |
| 44. | Spechler SJ, Sharma P, Souza RF, Inadomi JM, Shaheen NJ. American Gastroenterological Association technical review on the management of Barrett's esophagus. Gastroenterology. 2011;140:e18-52; quiz e13. [PubMed] |
| 45. | Lekakos L, Karidis NP, Dimitroulis D, Tsigris C, Kouraklis G, Nikiteas N. Barrett's esophagus with high-grade dysplasia: focus on current treatment options. World J Gastroenterol. 2011;17:4174-4183. [PubMed] |
| 46. | Gordon V, Jankowski J. Chemoprevention in Barrett's oesophagus. Best Pract Res Clin Gastroenterol. 2011;25:569-579. [PubMed] |
| 47. | Konda VJ, Dalal K. Optimal management of Barrett's esophagus: pharmacologic, endoscopic, and surgical interventions. Ther Clin Risk Manag. 2011;7:447-458. [PubMed] |
| 48. | Bennett C, Vakil N, Bergman J, Harrison R, Odze R, Vieth M, Sanders S, Gay L, Pech O, Longcroft-Wheaton G. Consensus statements for management of Barrett's dysplasia and early-stage esophageal adenocarcinoma, based on a Delphi process. Gastroenterology. 2012;143:336-346. [PubMed] |
| 49. | Bhardwaj A, McGarrity TJ, Stairs DB, Mani H. Barrett's Esophagus: Emerging Knowledge and Management Strategies. Patholog Res Int. 2012;2012:814146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 50. | Chai NL, Linghu EQ. Which is the optimal treatment for Barrett's esophagus with high grade dysplasia--ablation or complete endoscopic removal? Endoscopy. 2012;44:218; author reply 219. [PubMed] |
| 51. | Konda VJ, Waxman I. Endotherapy for Barrett's esophagus. Am J Gastroenterol. 2012;107:827-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 52. | Fornari F, Wagner R. Update on endoscopic diagnosis, management and surveillance strategies of esophageal diseases. World J Gastrointest Endosc. 2012;4:117-122. [PubMed] |
| 53. | Kahrilas PJ. The problems with surveillance of Barrett's esophagus. N Engl J Med. 2011;365:1437-1438. [PubMed] |
| 54. | Crockett SD, Lipkus IM, Bright SD, Sampliner RE, Wang KK, Boolchand V, Lutzke LS, Shaheen NJ. Overutilization of endoscopic surveillance in nondysplastic Barrett's esophagus: a multicenter study. Gastrointest Endosc. 2012;75:23-31.e2. [PubMed] |
| 55. | Chang JY, Talley NJ, Locke GR, Katzka DA, Schleck CD, Zinsmeister AR, Dunagan KT, Wu TT, Wang KK, Prasad GA. Population screening for barrett esophagus: a prospective randomized pilot study. Mayo Clin Proc. 2011;86:1174-1180. [PubMed] |
| 56. | Dias Pereira A, Chaves P. Columnar-lined oesophagus without intestinal metaplasia: results from a cohort with a mean follow-up of 7 years. Aliment Pharmacol Ther. 2012;36:282-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 57. | Choi SE, Hur C. Screening and surveillance for Barrett's esophagus: current issues and future directions. Curr Opin Gastroenterol. 2012;28:377-381. [PubMed] |
| 58. | Kariyawasam VC, Bourke MJ, Hourigan LF, Lim G, Moss A, Williams SJ, Fanning SB, Chung AM, Byth K. Circumferential location predicts the risk of high-grade dysplasia and early adenocarcinoma in short-segment Barrett's esophagus. Gastrointest Endosc. 2012;75:938-944. [PubMed] |
| 59. | Andrici J, Tio M, Cox MR, Eslick GD. Hiatal Hernia and the Risk of Barrett's Esophagus: A Meta-Analysis. J Gastroenterol Hepatol. 2012;Jun 13 [Epub ahead of print]. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 60. | Akiyama T, Yoneda M, Maeda S, Nakajima A, Koyama S, Inamori M. Visceral obesity and the risk of Barrett's esophagus. Digestion. 2011;83:142-145. [PubMed] |
| 61. | Nelsen EM, Kirihara Y, Takahashi N, Shi Q, Lewis JT, Namasivayam V, Buttar NS, Dunagan KT, Prasad GA. Distribution of body fat and its influence on esophageal inflammation and dysplasia in patients with Barrett's esophagus. Clin Gastroenterol Hepatol. 2012;10:728-34; quiz e61-2. [PubMed] |
| 62. | Abrams JA, Kapel RC, Lindberg GM, Saboorian MH, Genta RM, Neugut AI, Lightdale CJ. Adherence to biopsy guidelines for Barrett's esophagus surveillance in the community setting in the United States. Clin Gastroenterol Hepatol. 2009;7:736-742; quiz 710. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 283] [Cited by in RCA: 260] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 63. | Shahid MW, Wallace MB. Endoscopic imaging for the detection of esophageal dysplasia and carcinoma. Gastrointest Endosc Clin N Am. 2010;20:11-24, v. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 64. | Kara MA, Peters FP, Rosmolen WD, Krishnadath KK, ten Kate FJ, Fockens P, Bergman JJ. High-resolution endoscopy plus chromoendoscopy or narrow-band imaging in Barrett's esophagus: a prospective randomized crossover study. Endoscopy. 2005;37:929-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 198] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 65. | Curvers WL, Singh R, Song LM, Wolfsen HC, Ragunath K, Wang K, Wallace MB, Fockens P, Bergman JJ. Endoscopic tri-modal imaging for detection of early neoplasia in Barrett's oesophagus: a multi-centre feasibility study using high-resolution endoscopy, autofluorescence imaging and narrow band imaging incorporated in one endoscopy system. Gut. 2008;57:167-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 191] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 66. | Sharma P, Bansal A, Mathur S, Wani S, Cherian R, McGregor D, Higbee A, Hall S, Weston A. The utility of a novel narrow band imaging endoscopy system in patients with Barrett's esophagus. Gastrointest Endosc. 2006;64:167-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 230] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 67. | Mannath J, Subramanian V, Hawkey CJ, Ragunath K. Narrow band imaging for characterization of high grade dysplasia and specialized intestinal metaplasia in Barrett's esophagus: a meta-analysis. Endoscopy. 2010;42:351-359. [PubMed] |
| 68. | Curvers WL, van Vilsteren FG, Baak LC, Böhmer C, Mallant-Hent RC, Naber AH, van Oijen A, Ponsioen CY, Scholten P, Schenk E. Endoscopic trimodal imaging versus standard video endoscopy for detection of early Barrett's neoplasia: a multicenter, randomized, crossover study in general practice. Gastrointest Endosc. 2011;73:195-203. [PubMed] |
| 69. | Wasielica-Berger J, Baniukiewicz A, Wroblewski E, Chwiesko A, Dabrowski A. Magnification endoscopy and chromoendoscopy in evaluation of specialized intestinal metaplasia in Barrett's Esophagus. Dig Dis Sci. 2011;56:1987-1995. [PubMed] |
| 70. | Singh R, Nordeen N, Shanmuganathan G, Thurairajah PH, Bhat YM. Role of narrow band imaging in Barrett's esophagus. Dig Endosc. 2011;23 Suppl 1:83-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 71. | Singh R, Mei SC, Sethi S. Advanced endoscopic imaging in Barrett's oesophagus: a review on current practice. World J Gastroenterol. 2011;17:4271-4276. [PubMed] |
| 72. | Sharma P, Hawes RH, Bansal A, Gupta N, Curvers W, Rastogi A, Singh M, Hall M, Mathur SC, Wani SB. Standard endoscopy with random biopsies versus narrow band imaging targeted biopsies in Barrett's oesophagus: a prospective, international, randomised controlled trial. Gut. 2012;Feb 7 [Epub ahead of print]. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 245] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 73. | Lee MH, Buterbaugh K, Richards-Kortum R, Anandasabapathy S. Advanced endoscopic imaging for Barrett's Esophagus: current options and future directions. Curr Gastroenterol Rep. 2012;14:216-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 74. | Singh M, Bansal A, Curvers WL, Kara MA, Wani SB, Alvarez Herrero L, Lynch CR, van Kouwen MC, Peters FT, Keighley JD. Observer agreement in the assessment of narrowband imaging system surface patterns in Barrett's esophagus: a multicenter study. Endoscopy. 2011;43:745-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 75. | Camus M, Coriat R, Leblanc S, Brezault C, Terris B, Pommaret E, Gaudric M, Chryssostalis A, Prat F, Chaussade S. Helpfulness of the combination of acetic acid and FICE in the detection of Barrett's epithelium and Barrett's associated neoplasias. World J Gastroenterol. 2012;18:1921-1925. [PubMed] |
| 76. | De Palma GD. Confocal laser endomicroscopy in the "in vivo" histological diagnosis of the gastrointestinal tract. World J Gastroenterol. 2009;15:5770-5775. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 82] [Cited by in RCA: 88] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 77. | Kiesslich R, Gossner L, Goetz M, Dahlmann A, Vieth M, Stolte M, Hoffman A, Jung M, Nafe B, Galle PR. In vivo histology of Barrett's esophagus and associated neoplasia by confocal laser endomicroscopy. Clin Gastroenterol Hepatol. 2006;4:979-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 362] [Cited by in RCA: 321] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 78. | Meining A, Saur D, Bajbouj M, Becker V, Peltier E, Höfler H, von Weyhern CH, Schmid RM, Prinz C. In vivo histopathology for detection of gastrointestinal neoplasia with a portable, confocal miniprobe: an examiner blinded analysis. Clin Gastroenterol Hepatol. 2007;5:1261-1267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 110] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 79. | Dunbar KB. Endomicroscopy in the evaluation of Barrett's esophagus. Curr Opin Gastroenterol. 2011;27:374-382. [PubMed] |
| 80. | Canto MI. Endomicroscopy of Barrett's Esophagus. Gastroenterol Clin North Am. 2010;39:759-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 81. | Pohl H, Rösch T, Vieth M, Koch M, Becker V, Anders M, Khalifa AC, Meining A. Miniprobe confocal laser microscopy for the detection of invisible neoplasia in patients with Barrett's oesophagus. Gut. 2008;57:1648-1653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 149] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 82. | Dunbar KB, Okolo P, Montgomery E, Canto MI. Confocal laser endomicroscopy in Barrett's esophagus and endoscopically inapparent Barrett's neoplasia: a prospective, randomized, double-blind, controlled, crossover trial. Gastrointest Endosc. 2009;70:645-654. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 171] [Cited by in RCA: 150] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 83. | Wallace MB, Sharma P, Lightdale C, Wolfsen H, Coron E, Buchner A, Bajbouj M, Bansal A, Rastogi A, Abrams J. Preliminary accuracy and interobserver agreement for the detection of intraepithelial neoplasia in Barrett's esophagus with probe-based confocal laser endomicroscopy. Gastrointest Endosc. 2010;72:19-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 119] [Cited by in RCA: 111] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 84. | Konda VJ, Chennat JS, Hart J, Waxman I. Confocal laser endomicroscopy: potential in the management of Barrett's esophagus. Dis Esophagus. 2010;23:E21-E31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 85. | Falk GW. Probe-based confocal endomicroscopy in Barrett's esophagus: the real deal or another tease? Gastrointest Endosc. 2011;74:473-476. [PubMed] |
| 86. | Bertani H, Pigò F, Dabizzi E, Frazzoni M, Mirante VG, Manno M, Manta R, Conigliaro R. Advances in Endoscopic Visualization of Barrett's Esophagus: The Role of Confocal Laser Endomicroscopy. Gastroenterol Res Pract. 2012;2012:493961. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 87. | Bajbouj M, Vieth M, Rösch T, Miehlke S, Becker V, Anders M, Pohl H, Madisch A, Schuster T, Schmid RM. Probe-based confocal laser endomicroscopy compared with standard four-quadrant biopsy for evaluation of neoplasia in Barrett's esophagus. Endoscopy. 2010;42:435-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 84] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 88. | Sharma P, Meining AR, Coron E, Lightdale CJ, Wolfsen HC, Bansal A, Bajbouj M, Galmiche JP, Abrams JA, Rastogi A. Real-time increased detection of neoplastic tissue in Barrett's esophagus with probe-based confocal laser endomicroscopy: final results of an international multicenter, prospective, randomized, controlled trial. Gastrointest Endosc. 2011;74:465-472. [PubMed] |
| 89. | Becker V, Vieth M, Bajbouj M, Schmid RM, Meining A. Confocal laser scanning fluorescence microscopy for in vivo determination of microvessel density in Barrett's esophagus. Endoscopy. 2008;40:888-891. [PubMed] |
| 90. | Klinkenberg-Knol EC, Nelis F, Dent J, Snel P, Mitchell B, Prichard P, Lloyd D, Havu N, Frame MH, Romàn J. Long-term omeprazole treatment in resistant gastroesophageal reflux disease: efficacy, safety, and influence on gastric mucosa. Gastroenterology. 2000;118:661-669. [PubMed] |
| 91. | Becher A, El-Serag H. Systematic review: the association between symptomatic response to proton pump inhibitors and health-related quality of life in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2011;34:618-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 91] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 92. | Peters FT, Ganesh S, Kuipers EJ, Sluiter WJ, Klinkenberg-Knol EC, Lamers CB, Kleibeuker JH. Endoscopic regression of Barrett's oesophagus during omeprazole treatment; a randomised double blind study. Gut. 1999;45:489-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 177] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 93. | Srinivasan R, Katz PO, Ramakrishnan A, Katzka DA, Vela MF, Castell DO. Maximal acid reflux control for Barrett's oesophagus: feasible and effective. Aliment Pharmacol Ther. 2001;15:519-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 53] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 94. | Wilkinson SP, Biddlestone L, Gore S, Shepherd NA. Regression of columnar-lined (Barrett's) oesophagus with omeprazole 40 mg daily: results of 5 years of continuous therapy. Aliment Pharmacol Ther. 1999;13:1205-1209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 55] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 95. | Abu-Sneineh A, Tam W, Schoeman M, Fraser R, Ruszkiewicz AR, Smith E, Drew PA, Dent J, Holloway RH. The effects of high-dose esomeprazole on gastric and oesophageal acid exposure and molecular markers in Barrett's oesophagus. Aliment Pharmacol Ther. 2010;32:1023-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 96. | Kastelein F, Spaander MC, Biermann K, Vucelic B, Kuipers EJ, Bruno MJ. Role of acid suppression in the development and progression of dysplasia in patients with Barrett's esophagus. Dig Dis. 2011;29:499-506. [PubMed] |
| 97. | El-Serag HB, Aguirre TV, Davis S, Kuebeler M, Bhattacharyya A, Sampliner RE. Proton pump inhibitors are associated with reduced incidence of dysplasia in Barrett's esophagus. Am J Gastroenterol. 2004;99:1877-1883. [PubMed] |
| 98. | Hillman LC, Chiragakis L, Shadbolt B, Kaye GL, Clarke AC. Effect of proton pump inhibitors on markers of risk for high-grade dysplasia and oesophageal cancer in Barrett's oesophagus. Aliment Pharmacol Ther. 2008;27:321-326. [PubMed] |
| 99. | Gore S, Healey CJ, Sutton R, Eyre-Brook IA, Gear MW, Shepherd NA, Wilkinson SP. Regression of columnar lined (Barrett's) oesophagus with continuous omeprazole therapy. Aliment Pharmacol Ther. 1993;7:623-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 99] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 100. | Corley DA, Kerlikowske K, Verma R, Buffler P. Protective association of aspirin/NSAIDs and esophageal cancer: a systematic review and meta-analysis. Gastroenterology. 2003;124:47-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 373] [Cited by in RCA: 379] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 101. | Nguyen DM, Richardson P, El-Serag HB. Medications (NSAIDs, statins, proton pump inhibitors) and the risk of esophageal adenocarcinoma in patients with Barrett's esophagus. Gastroenterology. 2010;138:2260-2266. [PubMed] |
| 102. | Thrift AP, Pandeya N, Smith KJ, Green AC, Webb PM, Whiteman DC. The use of nonsteroidal anti-inflammatory drugs and the risk of Barrett's oesophagus. Aliment Pharmacol Ther. 2011;34:1235-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 103. | Liao LM, Vaughan TL, Corley DA, Cook MB, Casson AG, Kamangar F, Abnet CC, Risch HA, Giffen C, Freedman ND. Nonsteroidal anti-inflammatory drug use reduces risk of adenocarcinomas of the esophagus and esophagogastric junction in a pooled analysis. Gastroenterology. 2012;142:442-452.e5; quiz e22-23. [PubMed] |
| 104. | Omer ZB, Ananthakrishnan AN, Nattinger KJ, Cole EB, Lin JJ, Kong CY, Hur C. Aspirin protects against Barrett's esophagus in a multivariate logistic regression analysis. Clin Gastroenterol Hepatol. 2012;10:722-727. [PubMed] |
| 105. | Buttar NS, Wang KK, Anderson MA, Dierkhising RA, Pacifico RJ, Krishnadath KK, Lutzke LS. The effect of selective cyclooxygenase-2 inhibition in Barrett's esophagus epithelium: an in vitro study. J Natl Cancer Inst. 2002;94:422-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 98] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 106. | Buttar NS, Wang KK, Leontovich O, Westcott JY, Pacifico RJ, Anderson MA, Krishnadath KK, Lutzke LS, Burgart LJ. Chemoprevention of esophageal adenocarcinoma by COX-2 inhibitors in an animal model of Barrett's esophagus. Gastroenterology. 2002;122:1101-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 262] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 107. | Heath EI, Canto MI, Piantadosi S, Montgomery E, Weinstein WM, Herman JG, Dannenberg AJ, Yang VW, Shar AO, Hawk E. Secondary chemoprevention of Barrett's esophagus with celecoxib: results of a randomized trial. J Natl Cancer Inst. 2007;99:545-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 133] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 108. | Winberg H, Lindblad M, Lagergren J, Dahlstrand H. Risk factors and chemoprevention in Barrett's esophagus--an update. Scand J Gastroenterol. 2012;47:397-406. [PubMed] |
| 109. | Jankowski J, Moayyedi P. Re: Cost-effectiveness of aspirin chemoprevention for Barrett's esophagus. J Natl Cancer Inst. 2004;96:885-87; author reply 887. [PubMed] |
| 110. | Jankowski J, Sharma P. Review article: approaches to Barrett's oesophagus treatment-the role of proton pump inhibitors and other interventions. Aliment Pharmacol Ther. 2004;19 Suppl 1:54-59. [PubMed] |
| 111. | Tantau M, Mosteanu O, Pop T, Tantau A, Mester G. Endoscopic therapy of Barrett's esophagus and esophageal adenocarcinoma. J Gastrointestin Liver Dis. 2010;19:213-217. [PubMed] |
| 112. | Dunki-Jacobs EM, Martin RC. Endoscopic therapy for Barrett's esophagus: a review of its emerging role in optimal diagnosis and endoluminal therapy. Ann Surg Oncol. 2012;19:1575-1582. [PubMed] |
| 113. | Leggett CL, Prasad GA. High-grade dysplasia and intramucosal adenocarcinoma in Barrett's esophagus: the role of endoscopic eradication therapy. Curr Opin Gastroenterol. 2012;28:354-361. [PubMed] |
| 114. | Ortiz-Fernández-Sordo J, Parra-Blanco A, García-Varona A, Rodríguez-Peláez M, Madrigal-Hoyos E, Waxman I, Rodrigo L. Endoscopic resection techniques and ablative therapies for Barrett's neoplasia. World J Gastrointest Endosc. 2011;3:171-182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 115. | Halsey KD, Greenwald BD. Cryotherapy in the management of esophageal dysplasia and malignancy. Gastrointest Endosc Clin N Am. 2010;20:75-87, vi-vii. [PubMed] |
| 116. | Garman KS, Shaheen NJ. Ablative therapies for Barrett's esophagus. Curr Gastroenterol Rep. 2011;13:226-239. [PubMed] |
| 117. | Muguruma N, Okamoto K, Kimura T, Kishi K, Okahisa T, Okamura S, Takayama T. Endoscopic ablation therapy for gastrointestinal superficial neoplasia. Dig Endosc. 2012;24:139-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 118. | Ackroyd R, Tam W, Schoeman M, Devitt PG, Watson DI. Prospective randomized controlled trial of argon plasma coagulation ablation vs. endoscopic surveillance of patients with Barrett's esophagus after antireflux surgery. Gastrointest Endosc. 2004;59:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 52] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 119. | Byrne JP, Armstrong GR, Attwood SE. Restoration of the normal squamous lining in Barrett's esophagus by argon beam plasma coagulation. Am J Gastroenterol. 1998;93:1810-1815. [PubMed] |
| 120. | Wang KK, Kim JY. Photodynamic therapy in Barrett's esophagus. Gastrointest Endosc Clin N Am. 2003;13:483-489, vii. [PubMed] |
| 121. | Bulsiewicz WJ, Shaheen NJ. The role of radiofrequency ablation in the management of Barrett's esophagus. Gastrointest Endosc Clin N Am. 2011;21:95-109. [PubMed] |
| 122. | Terheggen G, Schumacher B, Neuhaus H. [Radiofrequency ablation using the HALO system in the treatment of Barrett's oesophagus]. Z Gastroenterol. 2012;50:601-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 123. | Greenwald BD, Dumot JA. Cryotherapy for Barrett's esophagus and esophageal cancer. Curr Opin Gastroenterol. 2011;27:363-367. [PubMed] |
| 124. | Xue HB, Tan HH, Liu WZ, Chen XY, Feng N, Gao YJ, Song Y, Zhao YJ, Ge ZZ. A pilot study of endoscopic spray cryotherapy by pressurized carbon dioxide gas for Barrett's esophagus. Endoscopy. 2011;43:379-385. [PubMed] |
| 125. | Chen AM, Pasricha PJ. Cryotherapy for Barrett's esophagus: Who, how, and why? Gastrointest Endosc Clin N Am. 2011;21:111-118. [PubMed] |
| 126. | Shaheen NJ, Greenwald BD, Peery AF, Dumot JA, Nishioka NS, Wolfsen HC, Burdick JS, Abrams JA, Wang KK, Mallat D. Safety and efficacy of endoscopic spray cryotherapy for Barrett's esophagus with high-grade dysplasia. Gastrointest Endosc. 2010;71:680-685. [PubMed] |
| 127. | Dumot JA, Vargo JJ, Falk GW, Frey L, Lopez R, Rice TW. An open-label, prospective trial of cryospray ablation for Barrett's esophagus high-grade dysplasia and early esophageal cancer in high-risk patients. Gastrointest Endosc. 2009;70:635-644. [PubMed] |
| 128. | Van Laethem JL, Peny MO, Salmon I, Cremer M, Devière J. Intramucosal adenocarcinoma arising under squamous re-epithelialisation of Barrett's oesophagus. Gut. 2000;46:574-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 170] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 129. | Shand A, Dallal H, Palmer K, Ghosh S, MacIntyre M. Adenocarcinoma arising in columnar lined oesophagus following treatment with argon plasma coagulation. Gut. 2001;48:580-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 130. | Overholt BF, Wang KK, Burdick JS, Lightdale CJ, Kimmey M, Nava HR, Sivak MV, Nishioka N, Barr H, Marcon N. Five-year efficacy and safety of photodynamic therapy with Photofrin in Barrett's high-grade dysplasia. Gastrointest Endosc. 2007;66:460-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 229] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 131. | Ban S, Mino M, Nishioka NS, Puricelli W, Zukerberg LR, Shimizu M, Lauwers GY. Histopathologic aspects of photodynamic therapy for dysplasia and early adenocarcinoma arising in Barrett's esophagus. Am J Surg Pathol. 2004;28:1466-1473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 44] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 132. | Pech O, Gossner L, May A, Rabenstein T, Vieth M, Stolte M, Berres M, Ell C. Long-term results of photodynamic therapy with 5-aminolevulinic acid for superficial Barrett's cancer and high-grade intraepithelial neoplasia. Gastrointest Endosc. 2005;62:24-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 118] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 133. | Sharma VK, Wang KK, Overholt BF, Lightdale CJ, Fennerty MB, Dean PJ, Pleskow DK, Chuttani R, Reymunde A, Santiago N. Balloon-based, circumferential, endoscopic radiofrequency ablation of Barrett's esophagus: 1-year follow-up of 100 patients. Gastrointest Endosc. 2007;65:185-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 201] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 134. | Lyday WD, Corbett FS, Kuperman DA, Kalvaria I, Mavrelis PG, Shughoury AB, Pruitt RE. Radiofrequency ablation of Barrett's esophagus: outcomes of 429 patients from a multicenter community practice registry. Endoscopy. 2010;42:272-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 100] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 135. | Fleischer DE, Overholt BF, Sharma VK, Reymunde A, Kimmey MB, Chuttani R, Chang KJ, Muthasamy R, Lightdale CJ, Santiago N. Endoscopic radiofrequency ablation for Barrett's esophagus: 5-year outcomes from a prospective multicenter trial. Endoscopy. 2010;42:781-789. [PubMed] |
| 136. | dos Santos RS, Bizekis C, Ebright M, DeSimone M, Daly BD, Fernando HC. Radiofrequency ablation for Barrett's esophagus and low-grade dysplasia in combination with an antireflux procedure: a new paradigm. J Thorac Cardiovasc Surg. 2010;139:713-716. [PubMed] |
| 137. | Shaheen NJ, Overholt BF, Sampliner RE, Wolfsen HC, Wang KK, Fleischer DE, Sharma VK, Eisen GM, Fennerty MB, Hunter JG. Durability of radiofrequency ablation in Barrett's esophagus with dysplasia. Gastroenterology. 2011;141:460-468. [PubMed] |
| 138. | Shaheen NJ, Sharma P, Overholt BF, Wolfsen HC, Sampliner RE, Wang KK, Galanko JA, Bronner MP, Goldblum JR, Bennett AE. Radiofrequency ablation in Barrett's esophagus with dysplasia. N Engl J Med. 2009;360:2277-2288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1146] [Cited by in RCA: 973] [Article Influence: 60.8] [Reference Citation Analysis (0)] |
| 139. | Pouw RE, Gondrie JJ, Sondermeijer CM, ten Kate FJ, van Gulik TM, Krishnadath KK, Fockens P, Weusten BL, Bergman JJ. Eradication of Barrett esophagus with early neoplasia by radiofrequency ablation, with or without endoscopic resection. J Gastrointest Surg. 2008;12:1627-1636; discussion 1636-1637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 82] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 140. | Ganz RA, Overholt BF, Sharma VK, Fleischer DE, Shaheen NJ, Lightdale CJ, Freeman SR, Pruitt RE, Urayama SM, Gress F. Circumferential ablation of Barrett's esophagus that contains high-grade dysplasia: a U.S. Multicenter Registry. Gastrointest Endosc. 2008;68:35-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 174] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 141. | Carriquiry L. Better knowledge of a disease that should be eradicated. World J Surg. 2012;36:1036. [PubMed] |
| 142. | Vaccaro BJ, Gonzalez S, Poneros JM, Stevens PD, Capiak KM, Lightdale CJ, Abrams JA. Detection of intestinal metaplasia after successful eradication of Barrett's Esophagus with radiofrequency ablation. Dig Dis Sci. 2011;56:1996-2000. [PubMed] |
| 143. | Yachimski P, Falk GW. Subsquamous intestinal metaplasia: implications for endoscopic management of Barrett's esophagus. Clin Gastroenterol Hepatol. 2012;10:220-224. [PubMed] |
| 144. | Gray NA, Odze RD, Spechler SJ. Buried metaplasia after endoscopic ablation of Barrett's esophagus: a systematic review. Am J Gastroenterol. 2011;106:1899-908; quiz 1909. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 151] [Cited by in RCA: 131] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 145. | Bammer T, Hinder RA, Klaus A, Trastek VF, Achem SR. Rationale for surgical therapy of Barrett esophagus. Mayo Clin Proc. 2001;76:335-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 146. | Ye W, Chow WH, Lagergren J, Yin L, Nyrén O. Risk of adenocarcinomas of the esophagus and gastric cardia in patients with gastroesophageal reflux diseases and after antireflux surgery. Gastroenterology. 2001;121:1286-1293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 174] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 147. | Gutschow CA, Schröder W, Prenzel K, Bollschweiler E, Romagnoli R, Collard JM, Hölscher AH. Impact of antireflux surgery on Barrett's esophagus. Langenbecks Arch Surg. 2002;387:138-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 148. | Corey KE, Schmitz SM, Shaheen NJ. Does a surgical antireflux procedure decrease the incidence of esophageal adenocarcinoma in Barrett's esophagus? A meta-analysis. Am J Gastroenterol. 2003;98:2390-2394. [PubMed] |
| 149. | Parrilla P, Martínez de Haro LF, Ortiz A, Munitiz V, Molina J, Bermejo J, Canteras M. Long-term results of a randomized prospective study comparing medical and surgical treatment of Barrett's esophagus. Ann Surg. 2003;237:291-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 150. | Miholic J, Hafez J, Lenglinger J, Wrba F, Wischin C, Schütz K, Hudec M. Hiatal hernia, Barrett's esophagus, and long-term symptom control after laparoscopic fundoplication for gastroesophageal reflux. Surg Endosc. 2012;26:3225-3231. [PubMed] |
| 151. | Parrilla P, Martínez de Haro LF, Ortiz A, Munitiz V, Molina J, Bermejo J, Canteras M. Long-term results of a randomized prospective study comparing medical and surgical treatment of Barrett's esophagus. Ann Surg. 2003;237:291-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 152. | Kelty CJ, Falk GL. Anti-reflux surgery does not remove cancer risk in Barrett's esophagus. Surg Endosc. 2011;25:3948; author reply 3949-3950. [PubMed] |
| 153. | Simonka Z, Paszt A, Abrahám S, Pieler J, Tajti J, Tiszlavicz L, Németh I, Izbéki F, Rosztóczy A, Wittmann T. The effects of laparoscopic Nissen fundoplication on Barrett's esophagus: long-term results. Scand J Gastroenterol. 2012;47:13-21. [PubMed] |
| 154. | Kauttu T, Räsänen J, Krogerus L, Sihvo E, Puolakkainen P, Salo JA. Long-term results of ablation with antireflux surgery for Barrett's esophagus: a clinical and molecular biologic study. Surg Endosc. 2012;26:1892-1897. [PubMed] |
| 155. | Buttar NS, Wang KK, Sebo TJ, Riehle DM, Krishnadath KK, Lutzke LS, Anderson MA, Petterson TM, Burgart LJ. Extent of high-grade dysplasia in Barrett's esophagus correlates with risk of adenocarcinoma. Gastroenterology. 2001;120:1630-1639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 266] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 156. | DeMeester SR, DeMeester TR. Columnar mucosa and intestinal metaplasia of the esophagus: fifty years of controversy. Ann Surg. 2000;231:303-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 188] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 157. | DeMeester SR. Adenocarcinoma of the esophagus and cardia: a review of the disease and its treatment. Ann Surg Oncol. 2006;13:12-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 154] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 158. | Pennathur A, Landreneau RJ, Luketich JD. Surgical aspects of the patient with high-grade dysplasia. Semin Thorac Cardiovasc Surg. 2005;17:326-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 159. | DeMeester SR. Evaluation and treatment of superficial esophageal cancer. J Gastrointest Surg. 2010;14 Suppl 1:S94-S100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 160. | Oelschlager BK, Pellegrini CA. Laparoscopic treatment of Barrett's esophagus*. Dis Mon. 2004;50:580-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 161. | Luna RA, Gilbert E, Hunter JG. High-grade dysplasia and intramucosal adenocarcinoma in Barrett's esophagus: the role of esophagectomy in the era of endoscopic eradication therapy. Curr Opin Gastroenterol. 2012;28:362-369. [PubMed] |
| 162. | Hölscher AH, Vallböhmer D, Gutschow C, Bollschweiler E. Reflux esophagitis, high-grade neoplasia, and early Barrett's carcinoma-what is the place of the Merendino procedure? Langenbecks Arch Surg. 2009;394:417-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |