Published online Apr 28, 2012. doi: 10.3748/wjg.v18.i16.1996
Revised: January 4, 2012
Accepted: February 26, 2012
Published online: April 28, 2012
Regional portal hypertension is a rare cause of upper gastrointestinal bleeding. We reported an extremely rare case in which regional portal hypertension was associated with both the splenic arteriovenous fistula and chronic pancreatitis. In June 2010, our patient, a 41-year-old man, was admitted to a local hospital due to a sudden melena and dizziness without haematemesis and jaundice. The splenic arteriovenous fistula in this patient was successfully occluded through transcatheter arterial embolization. At the 12-mo follow-up, our patient was in good condition.
- Citation: Chen B, Tang CW, Zhang CL, Cao JW, Wei B, Li X. Melena-associated regional portal hypertension caused by splenic arteriovenous fistula. World J Gastroenterol 2012; 18(16): 1996-1998
- URL: https://www.wjgnet.com/1007-9327/full/v18/i16/1996.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i16.1996
Regional portal hypertension is a rare cause of upper gastrointestinal bleeding, with pancreatitis disease being the most frequently reported cause in the literature[1,2]. Splenic arteriovenous fistulas are also rare. Until now, there are approximately 126 reported cases of splenic arteriovenous fistula in the database of PubMed. Herein, we reported an extremely rare case in which regional portal hypertension was associated with both the splenic arteriovenous fistula and chronic pancreatitis.
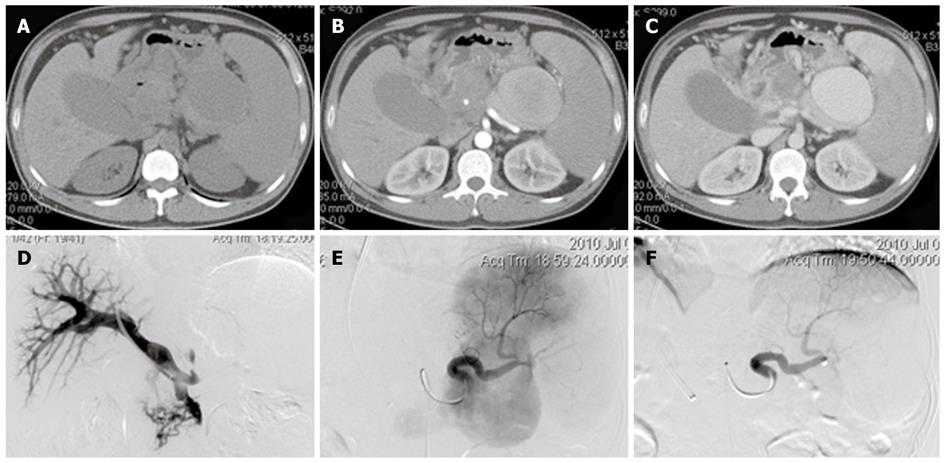
A 41-year-old man was admitted to a local hospital in June 2010 due to a sudden melena and dizziness without haematemesis and jaundice. He was managed conservatively, with fluid support and blood transfusion. No melena occurred again, and the symptom of dizziness was reduced. With the melena of unknown causes, he was referred to our institution for further diagnosis and treatment. On admission, his temperature was 36.7 °C, pulse was 85 times/min, respiration was 19 times/min, and blood pressure was 124/76 mmHg. Splenomegaly was found in physical examination. The liver was not palpable and no signs of jaundice were observed. The patient had a history of alcohol abuse, but no history of liver disease, trauma and surgery. Five years ago, the patient had an acute pancreatitis which recurred for five times. The details of laboratory tests were as follows: red blood cell 4.13 × 1012/L, hemoglobin 119 g/L, platelet 246 × 109/L, white blood cell 6.90 × 109/L, total bilirubin 13.3 μmol/L, albumin 42.9 g/L, creatinine (CREA) 572.9 μmol /L, glucose (GLU) 0 9.53 mmol/L, GLU120 21.75 mmol/L, prothrombin time 12.0 s, and alpfa-fetoprotein 1.36 ng/mL. Tests for HBsAg, HBeAg, anti-HBe, anti-HBc, anti-HCV and anti-HBs were all negative, except for anti-HBs. Gastroscopy revealed severe gastric varices and non-atrophic gastritis with bile reflux. Unenhanced computed tomography (CT) scanning of upper abdomen showed an oval cystic low-density lesion located in the area of splenic hilum, which was easily misdiagnosed as pancreatic pseudocyst on unenhanced CT (Figure 1A) and as pseudoaneurysm on contrast-enhanced scan. The lesion was significantly enhanced on the arterial phase of contrast-enhanced scan (Figure 1B). And on the portal phase of contrast-enhanced CT scan, this lesion was further enhanced and collateral vessels could be shown at the fundus of the stomach (Figure 1C). Additionally, thrombosis in the splenic vein was also found on the portal phase of contrast-enhanced CT scan. Biopsy of the liver was not performed. The current diagnosis was regional portal hypertension considered to be related to chronic pancreatitis. Under local anesthesia, a percutaneous transjugular approach was used to estimate the portal venous pressure; the portal pressure was normal and an increased pressure of splenic vein was 23.5 mmHg (Figure 1D). Through a percutaneous femoral approach, splenic artery angiography showed, on the arterial phase, a smaller splenic artery, splenic vein aneurysmal expansion, and esophageal and gastric varices, suggesting the formation of splenic arteriovenous fistula (Figure 1E). With splenic artery being extremely tortuous, it was difficult for conventional catheter to track the orifice of the fistula through target vessels, therefore embolization of the fistula was performed using a micro-catheter. Postoperative angiography revealed that splenic arteriovenous fistula had been totally occluded (Figure 1F).
Regional portal hypertension, also known as sinistral or left-sided portal hypertension, is a rare cause of upper gastrointestinal bleeding, with pancreatitis disease being the most frequently reported cause in the literature[1,2]. Splenic arteriovenous fistula is a rare but potentially curable cause of portal hypertension. The fistula may be congenital or acquired. It is thought that they arise from rupture of a splenic artery aneurysm or after abdominal trauma, surgery or pancreatitis[3]. To our best knowledge, splenic arteriovenous fistulas related to pancreatitis have been rarely reported and its pathogenesis remains unclear[4]. In this case, the fistula arose from pancreatitis, and regional portal hypertension was caused by splenic arteriovenous fistula and splenic vein thrombosis, with the former playing a major role. As for regional portal hypertension, the key point is to make the correct diagnosis as soon as possible, because it is curable. It should be considered in the presence of gastrointestinal bleeding with normal liver function tests and splenomegaly. Surgical excision of splenic arteriovenous fistula is technically difficult, and is sometimes unsuccessful because of the remote location of the lesion, presence of numerous portal collaterals, and adhesion. Interventional radiologic technique, such as transcatheter arterial embolization, has been demonstrated to be a safe and effective alternative to surgery[5]. The splenic arteriovenous fistula in our patient was successfully occluded through transcatheter arterial embolization. At the 12-mo follow-up, this patient was found in good condition.
Peer reviewer: Dr. Andrea De Gottardi, Hepatology-Inselspital, Freiburg Strasse, Berne 3010, Switzerland
S- Editor Gou SX L- Editor Ma JY E- Editor Zhang DN
| 1. | Köklü S, Coban S, Yüksel O, Arhan M. Left-sided portal hypertension. Dig Dis Sci. 2007;52:1141-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 132] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 2. | Sakorafas GH, Sarr MG, Farley DR, Farnell MB. The significance of sinistral portal hypertension complicating chronic pancreatitis. Am J Surg. 2000;179:129-133. [PubMed] |
| 3. | Vanhoenacker FM, Op de Beeck B, De Schepper AM, Salgado R, Snoeckx A, Parizel PM. Vascular disease of the spleen. Semin Ultrasound CT MR. 2007;28:35-51. [PubMed] |
| 4. | Raat H, Stockx L, De Meester X, Van Steenbergen W, Marchal G. Percutaneous embolization of a splenic arteriovenous fistula related to acute necrotizing pancreatitis. Eur Radiol. 1999;9:753. [PubMed] |
| 5. | Hung CF, Tseng JH, Lui KW, Wan YL, Tsai CC, Shem CH, Wu CS. Intractable oesophageal variceal bleeding caused by splenic arteriovenous fistula: treatment by transcatheter arterial embolization. Postgrad Med J. 1999;75:355-357. [PubMed] |