Published online Oct 14, 2011. doi: 10.3748/wjg.v17.i38.4344
Revised: April 27, 2011
Accepted: May 4, 2011
Published online: October 14, 2011
Inflammatory bowel disease (IBD) is often associated with extraintestinal manifestations (EIMs) such as optic neuritis (ON), although this has been described in only a few adult patients so far, all of whom were affected with Crohn’s disease (CD). Furthermore, ON and demyelinating diseases have been demonstrated to be more frequent in IBD patients than in control populations. In our current case report, we describe a child with active CD who developed sudden blindness due to bilateral ON that was not related to any known cause, and that promptly responded to a high dose of steroids. Investigations and a clinical follow-up have so far ruled out the development of demyelinating diseases in this patient. To our knowledge, this is the first report of ON in a pediatric patient with CD. Possible explanations for this case include an episodic EIM of an active bowel disease, an associated autoimmune disorder such as a recurrent isolated ON, the first manifestation of multiple sclerosis, or another demyelinating disease that could appear in a later follow-up.
- Citation: Barabino AV, Gandullia P, Calvi A, Vignola S, Arrigo S, Marco RD. Sudden blindness in a child with Crohn’s disease. World J Gastroenterol 2011; 17(38): 4344-4346
- URL: https://www.wjgnet.com/1007-9327/full/v17/i38/4344.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i38.4344
Joint, skin, eye and biliary tract disorders are frequently associated with inflammatory bowel disease (IBD) as an extraintestinal manifestation (EIM), although nearly every organ may be involved in this disorder. Some EIMs are clearly related to intestinal disease activity, whereas others occur independently. Ophthalmologic complications are independent of the extent of bowel involvement, usually occurring during the early years of IBD. In rare cases, eye manifestations precede the IBD diagnosis and their course tends to parallel that of the underlying bowel disease. Several ophthalmologic manifestations from the anterior and the posterior segment have now been described[1]. Among the known posterior segment manifestations, optic neuritis (ON) may be present in up to 4% of adult IBD patients[2,3]. When ON is diagnosed, a thorough differential diagnosis has to be applied as it can be an isolated condition or a manifestation of neurologic or systemic disease. In particular, ON may be the sign of an autoimmune demyelinating disease.
A possible association between multiple sclerosis (MS) and IBD has been hypothesized for decades and an approximately 3-fold increased risk of MS in IBD patients has been suggested[4]. On the other hand anti-tumor necrosis factor (TNF)-α therapies may trigger the new onset of MS, ON and other demyelinating diseases in IBD patients. However, because of the small number of controlled clinical trials with anti-TNF-α medications conducted to date, it is not possible to state with certainty whether a causal association exists between these drugs and demyelinating disorders. Nevertheless, a recent study conducted in the era before anti-TNF therapies[4], has demonstrated that patients with Crohn’s disease (CD) and ulcerative colitis were 54% and 75% more likely, respectively, than community controls to have been diagnosed with MS, ON or other demyelinating conditions[5]. The results of this study have given credence to the emerging concept that patients with immune-mediated conditions are more likely than the general population to have another autoimmune disease. Thus, ON in IBD patients can signify an EIM of the underlying bowel disease or a demyelinating condition that seems more frequent in this population.
An 11-year-old boy presented with a recent history of severe and bloody diarrhea, abdominal pain and vomiting. The abdomen was meteoric and tender. His weight was 26 kg and height was 138 cm, which were, respectively, less than the 5th and the 10th-25th percentile for his age. Laboratory tests revealed hemoglobin 11 g/dL, platelets 507 000/m3, erythrocyte sedimentation rate 38 mm/h, C-reactive protein 9.5 mg/dL (normal < 0.45 mg/dL), and albumin 2.4 g/dL (normal > 3.5 g/dL). Thorough stool investigations ruled out infection or infestation. An abdominal ultrasonogram demonstrated thickened (9 mm) and hyperemic colonic walls. The patient was given iv albumin, metronidazole, ampicillin + sulbactam, and omeprazole without subsequent improvement. Pancolonoscopy with a terminal ileoscopy showed skip areas of deep ulcerations with a cobblestone pattern in the transverse and descending colon, and focal aphthous ulcers in the rectum. Esophagogastroduodenoscopy revealed patchy duodenal erosions and deep, wide ulcerations of the stomach. Owing to endoscopic findings that were consistent with severe CD fasting, a regimen of total parenteral nutrition (TPN) and iv methylprednisolone (20 mg bid) was started, and resulted in a slow clinical improvement. On histology, a chronic-active, patchy, erosive-ulcerative inflammation of the colon, stomach and duodenum, without evidence of granulomata, was seen. A barium meal and follow-through did not reveal small bowel lesions. On hospitalization day 20, at 14 d after the commencement of this treatment, steroids were tapered (5 mg/wk) and the antibiotics and TPN were discontinued.
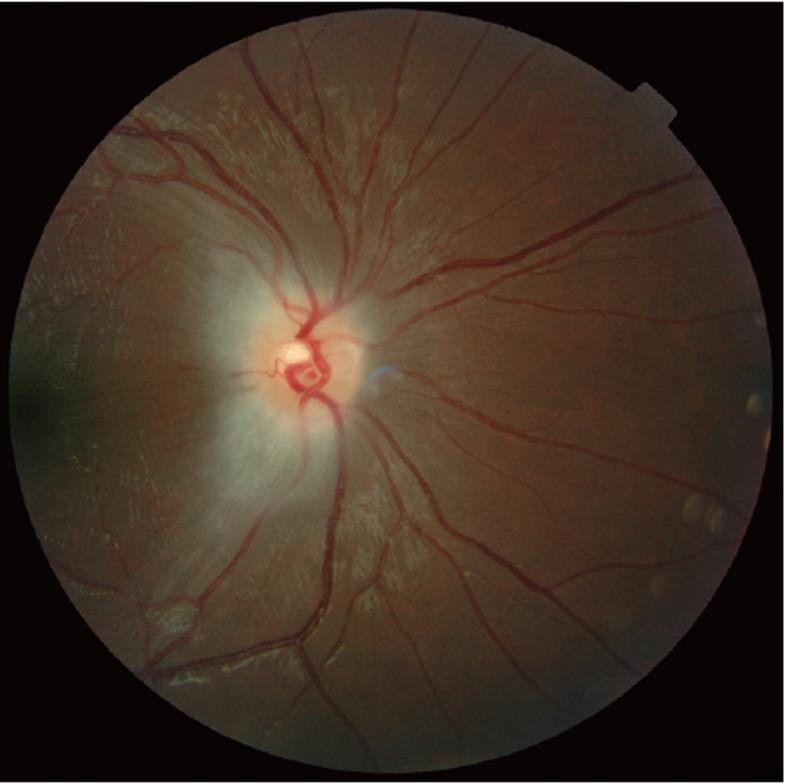
On hospitalization day 25, on which 35 mg/d of iv steroids was given, the patient suddenly complained of bilateral visual loss. Diffuse and severe bilateral papilledema was detected (Figure 1). Magnetic resonance imaging (MRI) of the head, with paramagnetic iv contrast, and cytological and chemical analysis of the cerebrospinal fluid (CSF) showed no abnormalities. A diagnosis of ON was made and three iv pulses of methylprednisolone (30 mg/kg on alternate days) were administered. At the end of this treatment course, visual acuity completely recovered and the optic disc appearance improved. Steroid treatment was prolonged orally. MRI of the spine, visual and brainstem auditory and somatosensory-evoked potentials, motor and sensory nerve conduction velocity, blood and CSF polymerase chain reaction analysis for viruses, CSF monoclonal band and the B12 blood level showed normal or negative results. On hospitalization day 40, the child was eventually discharged and was in clinical remission on prednisone (25 mg/d to be tapered to 5 mg weekly until discontinuation) and azathioprine (1 mg/kg per day). Eighteen days after the ON diagnosis, the optic nerve edema had resolved and optical coherence tomography revealed decreased thickness of the retinal nerve fiber layer (RNFL) in the temporal superior quadrant of both eyes. The child was then regularly followed-up and at 20 mo after diagnosis is still in clinical remission with normal growth.
IBDs are often associated with EIMs which occur in approximately one third of patients[6]. Little has been published, however, on their frequency in pediatric patients and most of the current data are from studies in adults[7,8]. The incidence of ocular manifestations ranges from 3.5% to 43% according to previous reports[1-3,9-11] and seems to occur more frequently in colonic CD cases. The most common complications of IBDs are episcleritis, scleritis, and uveitis occurring in up to 29%, 18% and 17% of patients, respectively. The reported incidence of posterior segment manifestations ranges between less than 1% to 30% depending upon the series[1,2,12]. ON as an ophthalmologic manifestation of IBD has been described in only a few adult patients so far[1,12,13], all affected with CD. The term ON is used to describe any inflammation, demyelinization, or degeneration of the optic nerve with attendant impairment of function[14]. The disease process for ON is usually acute, with a rapid and progressive loss of vision, and may be unilateral or bilateral. In childhood, ON may occur as an isolated condition or as a manifestation of a neurologic or systemic disease. ON may also be secondary to inflammatory disease, infections, toxic causes or a vitamin B12 deficiency and may signify a demyelinating disease of childhood such as MS, Devic disease or acute diffuse encephalomyelitis. Patients who experience an isolated episode of ON can develop other symptoms later on associated with a demyelinating disorder. High-dose iv methylprednisolone may help to speed the visual recovery in young adults[14].
We here present a case report of a child with severe acute gastrointestinal symptoms in which our investigations, in accordance with the Porto criteria[15], led to the diagnosis of diffuse CD. This disease was difficult to treat and required iv steroids, antibiotics and TPN. The patient subsequently developed a sudden loss of visual acuity consistent with a bilateral ON and not due to any known cause. This vision loss was promptly responsive to a high dose of steroids. Nevertheless after resolution, a residual segmental decrease of RNFL thickness was detected in both eyes. An extensive diagnostic work-up was required and investigations and clinical follow-up, that have not shown any recurrence, have ruled out demyelinating diseases thus far in this patient.
Reports of MS, demyelination (D), and ON associated with anti-TNF-α therapy have resulted in warnings in the instructions for prescribing of infliximab and adalimumab. However, the underlying relationship between IBD and these neurologic conditions has not been established. A previous retrospective cohort and retrospective cross-sectional study, performed in the era before TNF-α blockers were in clinical use, has reported that the incidence and prevalence of MS/D/ON is higher in patients with IBD compared with their matched controls. In particular, ON was recorded in 6 of 7988 CD patients (0.08%) and in 17 of 12 185 ulcerative colitis patients (0.14%) in this study, in comparison with 50 of 80 666 controls (0.06%)[4].
To our knowledge, our current report represents the first description of ON in a pediatric patient with CD. A correlation between ON and CD is possible in this case but, taking into account the current literature, a clear relationship cannot yet be argued. Our current case may represent an episodic EIM of the active bowel disease or an associated autoimmune disorder, such as recurrent isolated ON. It could also be a first manifestation of MS or other demyelinating diseases that are more frequent in IBD patients and could be clarified in a later follow-up of our current patient. We conclude from this case study that, although extremely rare, ON should be considered by pediatric gastroenterologists and ophthalmologists as a possible IBD complication. In patients with IBD presenting with ON, a thorough diagnostic work-up and strict long-term follow-up are recommended.
Peer reviewers: Walter Fries, MD, Department Medicina Interna and Terapia Medica, UOS Malattie Intestinali Croniche, Policlinico Messina, 98125 Messina, Italy; Andrew S Day, MB, ChB, MD, FRACP, AGAF, A/Professor, Paediatric Gastroenterology, Christchurch Hospital, and Associate Professor, Head of Department, Department of Paediatrics, University of Otago, Christchurch, PO Box 8140, Christchurch, New Zealand
S- Editor Tian L L- Editor Cant MR E- Editor Li JY
| 1. | Felekis T, Katsanos K, Kitsanou M, Trakos N, Theopistos V, Christodoulou D, Asproudis I, Tsianos EV. Spectrum and frequency of ophthalmologic manifestations in patients with inflammatory bowel disease: a prospective single-center study. Inflamm Bowel Dis. 2009;15:29-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 77] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Ghanchi FD, Rembacken BJ. Inflammatory bowel disease and the eye. Surv Ophthalmol. 2003;48:663-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Knox DL, Schachat AP, Mustonen E. Primary, secondary and coincidental ocular complications of Crohn's disease. Ophthalmology. 1984;91:163-173. [PubMed] |
| 4. | Gupta G, Gelfand JM, Lewis JD. Increased risk for demyelinating diseases in patients with inflammatory bowel disease. Gastroenterology. 2005;129:819-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 199] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 5. | Loftus EV. Inflammatory bowel disease extending its reach. Gastroenterology. 2005;129:1117-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Aloi M, Cucchiara S. Extradigestive manifestations of IBD in pediatrics. Eur Rev Med Pharmacol Sci. 2009;13 Suppl 1:23-32. [PubMed] |
| 7. | Rothfuss KS, Stange EF, Herrlinger KR. Extraintestinal manifestations and complications in inflammatory bowel diseases. World J Gastroenterol. 2006;12:4819-4831. [PubMed] |
| 8. | Salvarani C, Fries W. Clinical features and epidemiology of spondyloarthritides associated with inflammatory bowel disease. World J Gastroenterol. 2009;15:2449-2455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Mintz R, Feller ER, Bahr RL, Shah SA. Ocular manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2004;10:135-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 104] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Rankin GB, Watts HD, Melnyk CS, Kelley ML. National Cooperative Crohn's Disease Study: extraintestinal manifestations and perianal complications. Gastroenterology. 1979;77:914-920. [PubMed] |
| 11. | Greenstein AJ, Janowitz HD, Sachar DB. The extra-intestinal complications of Crohn's disease and ulcerative colitis: a study of 700 patients. Medicine (Baltimore). 1976;55:401-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 805] [Cited by in RCA: 693] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 12. | Ernst BB, Lowder CY, Meisler DM, Gutman FA. Posterior segment manifestations of inflammatory bowel disease. Ophthalmology. 1991;98:1272-1280. [PubMed] |
| 13. | Han SH, Lee OY, Yang SY, Jun DW, Lee HL, Jeon YC, Han DS, Sohn JH, Yoon BC, Choi HS. A case of optic neuritis associated with Crohn's disease. Korean J Gastroenterol. 2006;48:42-45. [PubMed] |
| 14. | Olitsky SE, Hug D, Gmith LP. Abnormalities of the optic nerve. Nelson Textbook of Pediatrics. Philadelphia: Saunders Elsevier 2007; 2067. |
| 15. | IBD Working Group of ESPGHAN. Inflammatory bowel disease in children and adolescents: recommendations for diagnosis--the Porto criteria. J Pediatr Gastroenterol Nutr. 2005;41:1-7. [PubMed] |