Published online Jul 28, 2011. doi: 10.3748/wjg.v17.i28.3366
Revised: December 27, 2010
Accepted: January 3, 2011
Published online: July 28, 2011
In endoscopic placement of multiple plastic biliary stents (PBSs), we sometimes experience proximal dislocation of the first PBS at the time of subsequent PBS insertion. We describe the case of a 79-year-old male with obstructive jaundice caused by cholangiocarcinoma who needed to receive multiple PBS placements for management of cholangitis. Although proximal dislocation of the first PBS was observed, we prevented the dislocation via our technique of using guidewire inserted from the distal end of the first PBS to the side hole as the anchor-wire. We could complete this technique only by inserting guidewire through the side hole of the first PBS during the process of releasing the first PBS and pulling out the guidewire and the inner sheath. It did not matter whether the anchor-wire went towards the third portion of the duodenum or the duodenal bulb. Here we introduce this “anchor-wire technique”, which is useful for the prevention of PBS proximal dislocation in placing multiple PBSs.
- Citation: Hamada T, Nakai Y, Matsubara S, Isayama H, Narita A, Watanabe K, Koike Y, Matsukawa S, Kawase T, Koike K. Anchor-wire technique for multiple plastic biliary stents to prevent stent dislocation. World J Gastroenterol 2011; 17(28): 3366-3368
- URL: https://www.wjgnet.com/1007-9327/full/v17/i28/3366.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i28.3366
Endoscopic placement of plastic biliary stents (PBSs) has become a widely accepted procedure for biliary obstruction. The utility of multiple PBSs was reported for the management of hilar biliary obstruction or the dilation of benign biliary stricture[1-3]. However, endoscopic placement of multiple PBSs is difficult and prolongs procedure time. One of the problems in endoscopic placement of multiple PBSs is proximal dislocation of the first PBS at the time of subsequent PBS insertions. A proximally dislocated PBS above the papilla may be very difficult to remove[4-6]. Here we report a technique to resolve this problem using an “anchor-wire”.
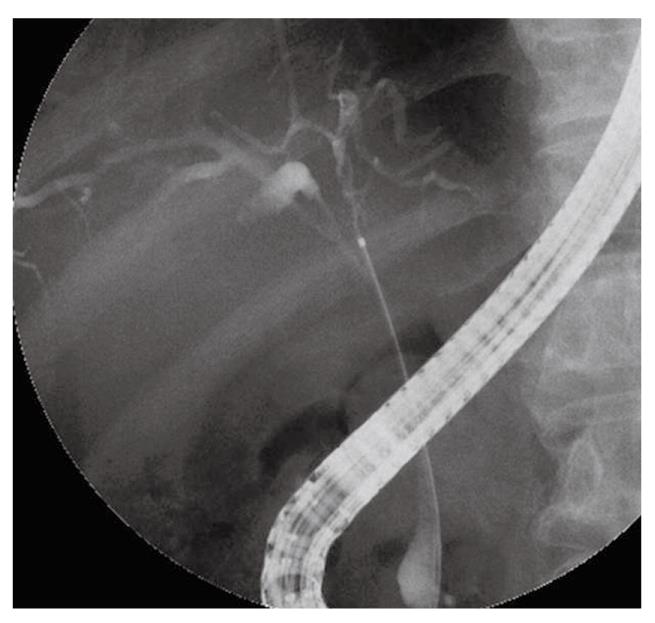
A 79-year-old male was admitted with acute obstructive suppurative cholangitis (AOSC). The first endoscopic retrograde cholangiography (ERC) showed severe biliary stenosis with type III hilar biliary stricture according to Bismuth’s classification (Figure 1)[7]. We placed three 5 Fr PBSs endoscopically, one each in the left hepatic duct (LHD), the anterior branch of the right hepatic duct (a-RHD) and the posterior branch of the right hepatic duct (p-RHD). The diagnosis of cholangiocarcinoma was pathologically confirmed. Radiation therapy was started after obstructive jaundice was resolved.
Two months later, he was admitted with AOSC and the two PBSs were distally dislocated and disappeared. ERC was performed to insert 3 larger diameter (7 Fr) PBSs. However, we failed to lead a guidewire to the LHD, because of the more severe stenosis, which was probably caused by radiation therapy. We decided to insert two 7 Fr PBSs (Flexima™, Boston Scientific, Natick, Mass) to the a-RHD and p-RHD. First, we inserted a 0.035 inch guidewire (RevoWave™, Piolax Medical Devices, Kanagawa, Japan) into the p-RHD using a bendable cannula (SwingTip™, Olympus, Tokyo, Japan) and inserted a PBS (7 Fr, 15 cm) to the p-RHD across the papilla. When we tried to insert another PBS (7 Fr, 15 cm) to the a-RHD, interference of the two PBSs caused proximal dislocation of the first PBS.
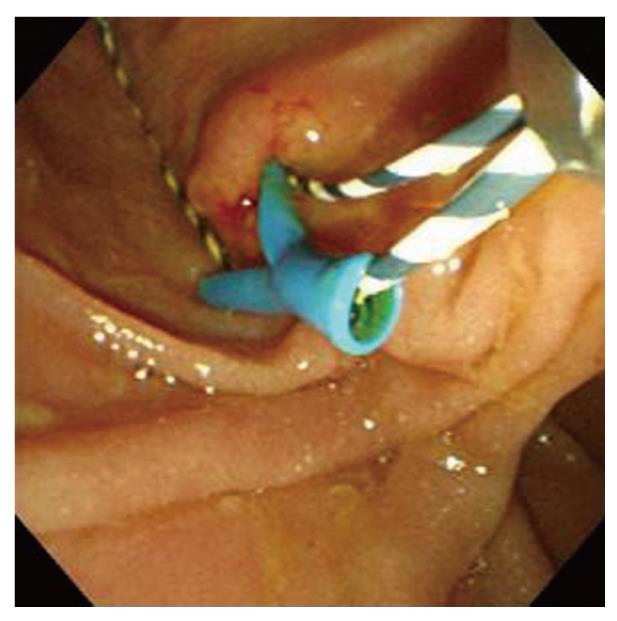
To prevent proximal dislocation of the first PBS into the bile duct, we inserted the stiff guidewire (RevoWave™) from the distal end of the first PBS through the distal side hole, leading it towards the third portion of the duodenum and made it work as an “anchor-wire” (Figure 2). When we subsequently inserted the second PBS, the anchor-wire successfully prevented proximal dislocation of the first PBS inclined to migrate into the bile duct, by pulling it down.
At the time of subsequent stent exchange, the anchor-wire to the duodenal bulb could also work as the anchor (Figure 3). This time, we could complete this technique only by inserting the guidewire through the side hole in the process of releasing the first stent and pulling out the guidewire and the inner sheath.
We reported a technique named for “the anchor-wire technique”, useful for preventing proximal dislocation of PBS in endoscopic placement of multiple PBSs.
Flexima™ is one of the most widely used PBSs, with a flap and a side hole on each end for preventing migration. However, we sometimes experience proximal dislocation of the first PBS at the time of subsequent PBS insertion when inserting multiple PBSs[3]. Proximal dislocation leads to stent dysfunction and PBSs dislocated above the papilla requires a particular technique for endoscopic removal[4-6]. Parlak et al[8] reported a technique for the prevention of this complication. They cannulated the distal side hole of the first PBS using a cannula and inserted a guidewire through the distal side of the PBS to the duodenum before they inserting the second PBS using the guidewire as the anchor. However, we experienced difficulty in realizing this technique for PBSs with side flaps, and distal migration of the first PBS could occur conversely, resulting from traction force of the anchor-wire at the time of the second PBS insertion. Furthermore, repeated insertion of a guidewire with a cannula was necessary, leading to a prolonged procedure time. Our technique can be completed with ease and certainty because we can insert the guidewire through the side hole of the first PBS in the process of releasing the first stent and pulling out the guidewire and the inner sheath.
In conclusion, this anchor-wire technique can prevent proximal dislocation in multiple PBSs insertion.
Peer reviewer: Dr. Thiruvengadam Muniraj, MBBS, MD, PhD, MRCP(UK), University of Pittsburgh Medical Center, 100 Chatham Park Drive, Apt 511, Pittsburgh, PA 15220, United States
S- Editor Sun H L- Editor Rutherford A E- Editor Zheng XM
| 1. | Chang WH, Kortan P, Haber GB. Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc. 1998;47:354-362. |
| 2. | Draganov P, Hoffman B, Marsh W, Cotton P, Cunningham J. Long-term outcome in patients with benign biliary strictures treated endoscopically with multiple stents. Gastrointest Endosc. 2002;55:680-686. |
| 3. | Costamagna G, Pandolfi M, Mutignani M, Spada C, Perri V. Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest Endosc. 2001;54:162-168. |
| 4. | Chaurasia OP, Rauws EA, Fockens P, Huibregtse K. Endoscopic techniques for retrieval of proximally migrated biliary stents: the Amsterdam experience. Gastrointest Endosc. 1999;50:780-785. |
| 5. | Katsinelos P, Kountouras J, Paroutoglou G, Chatzimavroudis G, Paikos D, Zavos C, Karakousis K, Gelas G, Tzilves D. Migration of plastic biliary stents and endoscopic retrieval: an experience of three referral centers. Surg Laparosc Endosc Percutan Tech. 2009;19:217-221. |
| 6. | Okabe Y, Tsuruta O, Kaji R, Ishida Y, Yasumoto M, Mitsuyama K, Suga H, Toyonaga A, Sata M. Endoscopic retrieval of migrated plastic stent into bile duct or pancreatic pseudocyst. Dig Endosc. 2009;21:1-7. |
| 7. | Bismuth H, Castaing D, Traynor O. Resection or palliation: priority of surgery in the treatment of hilar cancer. World J Surg. 1988;12:39-47. |