Published online Feb 28, 2010. doi: 10.3748/wjg.v16.i8.1031
Revised: November 26, 2009
Accepted: December 3, 2009
Published online: February 28, 2010
We report a unique case of communicating gastric duplication associated with pancreas divisum, diagnosed with a multidisciplinary approach, including X-rays, computed tomography, magnetic resonance imaging, esophagogastroduodenoscopy, ultrasound endoscopy and histology. We believe that this approach constitutes a fuller diagnostic evaluation, resulting in better and safer surgery.
- Citation: Di Pisa M, Curcio G, Marrone G, Milazzo M, Spada M, Traina M. Gastric duplication associated with pancreas divisum diagnosed by a multidisciplinary approach before surgery. World J Gastroenterol 2010; 16(8): 1031-1033
- URL: https://www.wjgnet.com/1007-9327/full/v16/i8/1031.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i8.1031
Gastric duplications are uncommon congenital anomalies[1], which are rarely found in adults, are more common in females, and are typically diagnosed in children. They constitute 2%-7% of gastrointestinal duplications[2]. The clinical presentation is usually nonspecific, though gastric duplications can be associated with severe clinical presentations[2]. Traditionally, the majority of these duplications are cystic, non-communicating and located along the greater curvature or posterior wall; there are very few cases in the literature of gastric duplication completely communicating with the gastric lumen[3].
We present a rare case of a communicating type gastric duplication associated with pancreas divisum in a young woman, diagnosed with a multidisciplinary approach, including computed tomography (CT), magnetic resonance imaging (MRI), endoscopy, histology and ultrasound endoscopy.
A 48-year-old healthy female presented with epigastric pain, nausea and bloating. She was admitted to our hospital for further investigation.
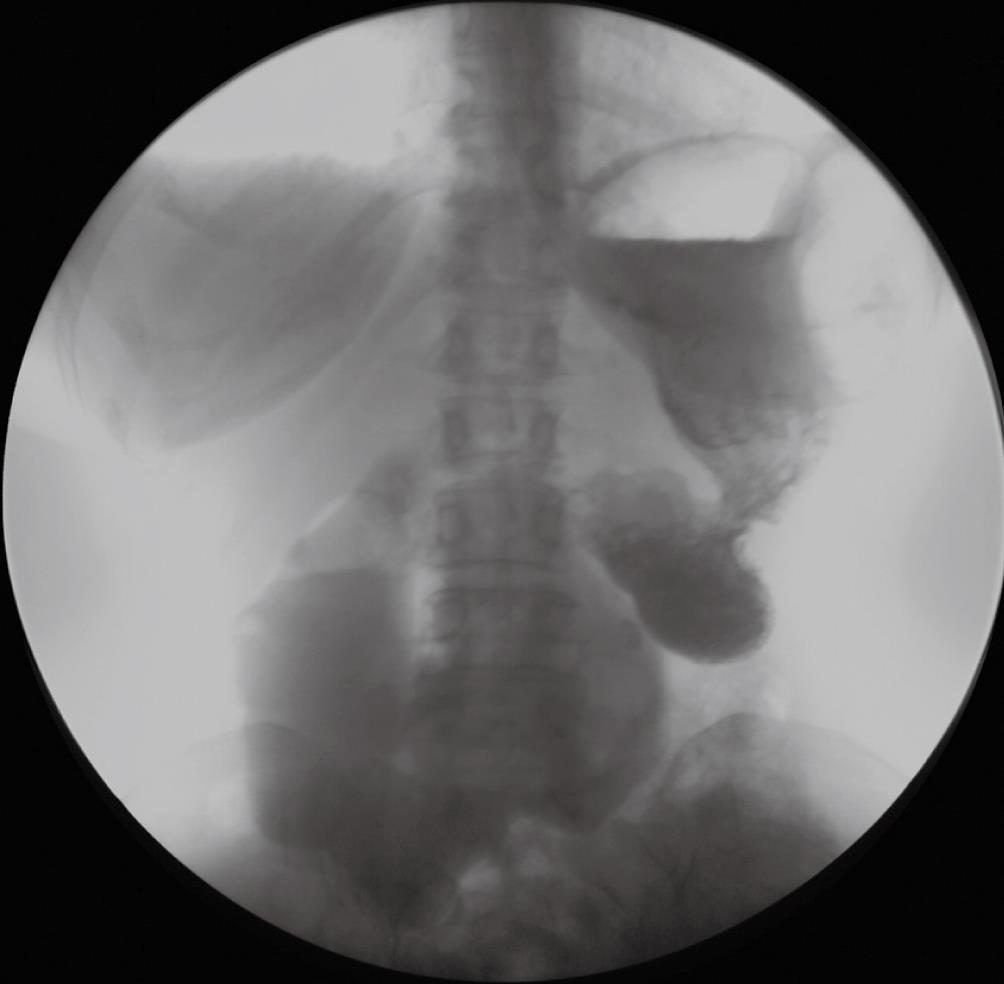
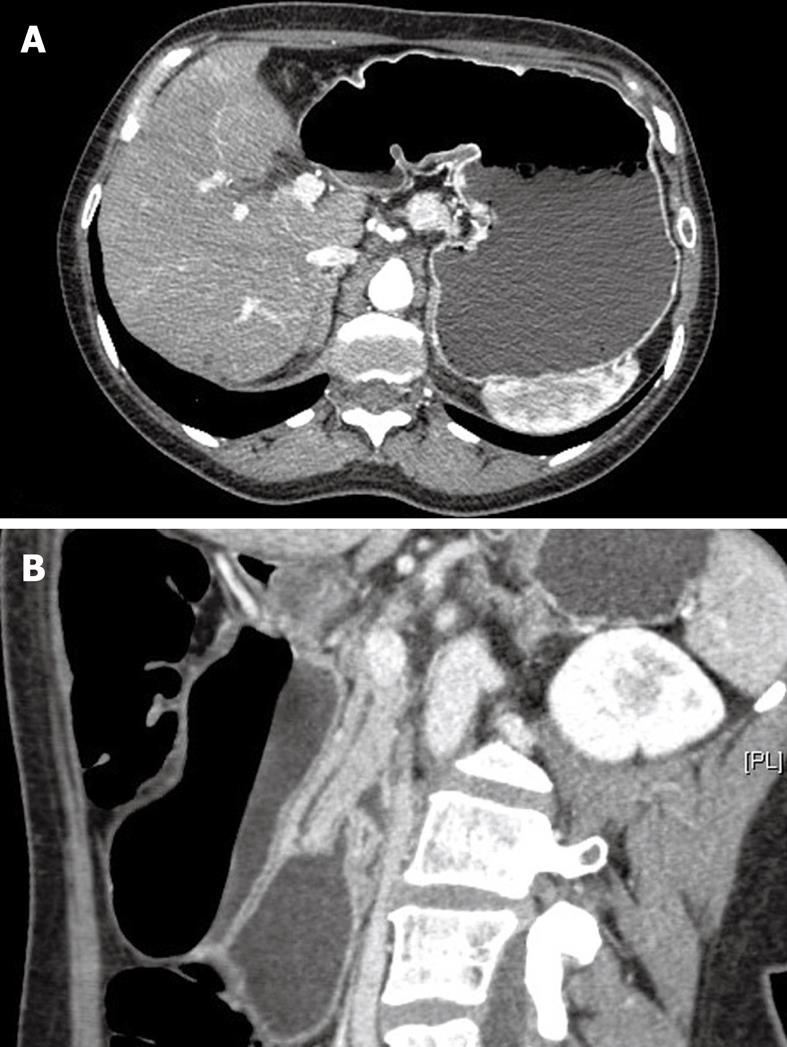
Her medical history was unremarkable. Physical examination and laboratory data were normal. First, an upper gastrointestinal barium contrast study was done, which showed a double compartment stomach, with the accessory stomach starting at the esophagogastric junction and continuing along the entire greater curvature to the pylorus, where it joined the lumen of the primary stomach. Both gastric lumens were filled with barium, providing evidence of free communication of the duplication with the gastric cavity (Figure 1). The patency of the gastric duplication and primary stomach was confirmed by CT with gastrografin (Figure 2). Also, in order to rule out possible biliary and pancreatic complications, with which gastric duplications can be associated, and in view of potential surgery, MRI was performed. It showed an incomplete pancreas divisum, with no common bilio-pancreatic duct (Figure 3). To confirm the gastric nature of the wall of the double stomach, a gastroscopy with ultrasound examination was performed.
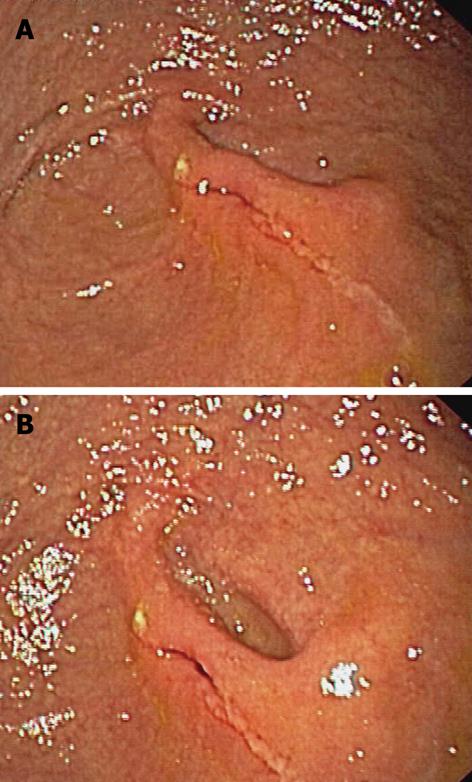
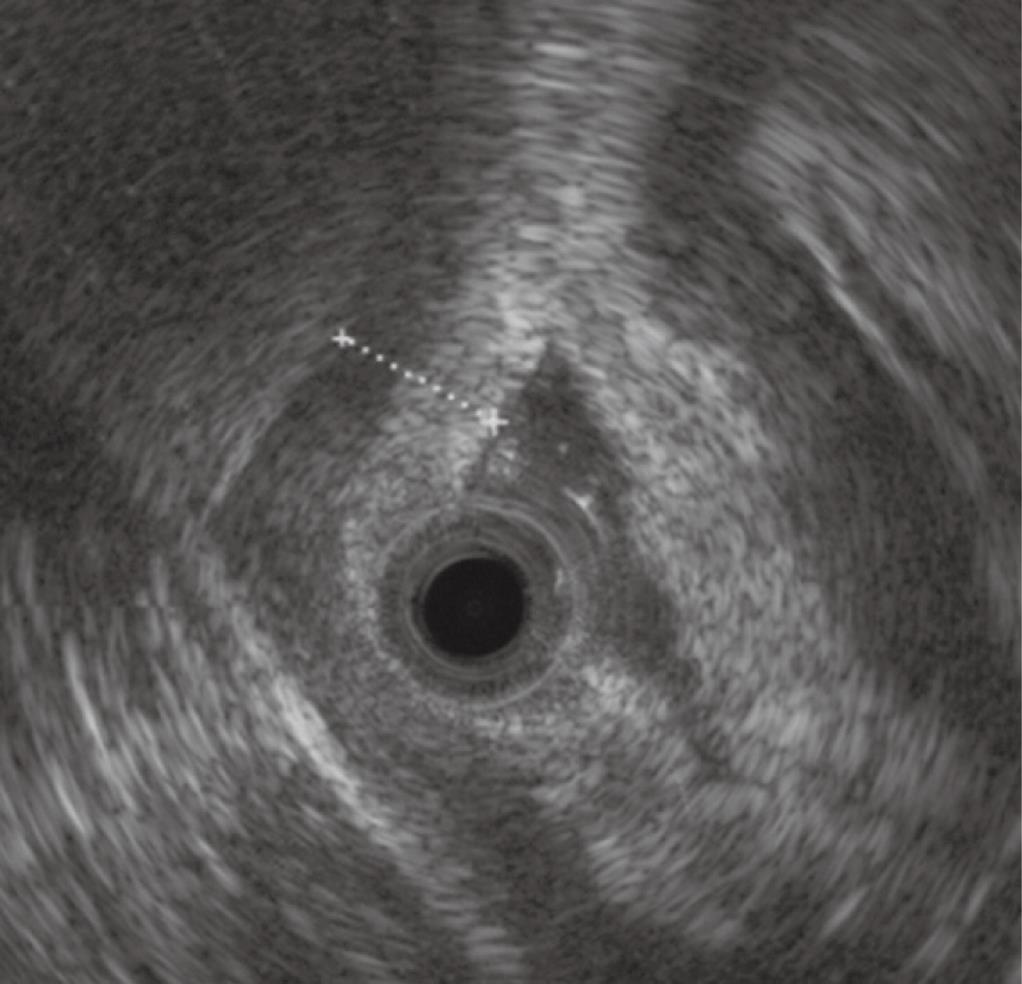
Under deep sedation, the patient was monitored continuously with electrocardiography, pulse oximetry and automatic recording of blood pressure and pulse. After introducing the scope into the esophagus, just behind the esophagogastric junction, a large cavity covered with normal mucosa was seen continuing into another cavity through a similar pylorus orifice. Beyond it, a new cavity, continuing into the duodenum, was observed (Figure 4). During the same endoscopic examination, a 20 MHz miniprobe was inserted into the operative channel of the endoscope and it revealed, on the first cavity, the pathognomonic multilayered appearance of the wall suggestive of a digestive origin, including an echogenic inner mucosal layer and a hypoechoic muscular layer (Figure 5). Finally, multiple biopsies were taken to confirm the gastric origin of the first cavity, and the histology pattern showed the presence of gastric mucosa with moderate Helicobacter pylori (H. pylori)-related gastritis in both cavities.
Definitively attributing the patient’s symptoms to this structure was difficult, but after 6 mo of omeprazole therapy (associated with H. pylori eradication therapy), the patient was asymptomatic and was referred to a surgeon.
Gastric duplications are uncommon congenital anomalies, rarely found in adults, and can involve any part of the gastrointestinal tract, from the mouth to the rectum[1]. They constitute about 4% of all alimentary tract duplications[1]. Gastric duplications share a common blood supply with the native bowel, though the stomach is the site least often affected, regardless of age. The etiology of duplication of the alimentary tract is likely multifactorial[2] (e.g. persistence of embryonic diverticula during development of the alimentary tract and recanalization and fusion of embryologic longitudinal folds). They can be cystic or tubular, are more common in females, and are, typically, diagnosed in children[2]. Gastric duplications can communicate with the gastric lumen or not. Communicating duplications usually do not require any intervention when both gastric lumens are patent, in contrast with non-communicating duplications, which require surgical treatment.
The clinical presentation is usually nonspecific; signs and symptoms of gastric duplications depend on the localization, size and whether or not there is communication with the gastric lumen. The most common symptoms are epigastric pain or discomfort, vomiting, and gastrointestinal bleeding[4]. In some cases, they can give rise to unusual complications, such as recurrent pancreatitis[5] or bile duct fistula[6], infection, peptic ulcers developing in the cyst, obstruction, and carcinoma arising in the cyst[7]. They can be associated with other congenital abnormalities: esophageal and duodenal diverticula, duplication cysts elsewhere in the digestive tract, annular and ectopic pancreas[8], and spinal abnormalities[9].
This is, to the best of our knowledge, the first report on a gastric duplication associated with a pancreas divisum. Alimentary tract duplications must be considered during evaluation of thoracic and abdominal masses, gastrointestinal hemorrhage of unclear etiology, intussusceptions and mechanical bowel obstructions.
This report presents a rare case of communicating gastric duplication associated with a pancreatic abnormality (pancreas divisum), diagnosed with a multidisciplinary approach, including not only imaging techniques (CT and MRI), but also ultrasound endoscopy and the histological pattern of the biopsy to confirm the gastric nature of both cavities, in order to refer the patient to surgery after a full evaluation.
Peer reviewer: Edward L Bradley III, MD, Professor of Surgery, Department of Clinical Science, Florida State University College of Medicine, 1600 Baywood Way, Sarasota, FL 34231, United States
S- Editor Tian L L- Editor Cant MR E- Editor Lin YP
| 1. | Ildstad ST, Tollerud DJ, Weiss RG, Ryan DP, McGowan MA, Martin LW. Duplications of the alimentary tract. Clinical characteristics, preferred treatment, and associated malformations. Ann Surg. 1988;208:184-189. |
| 2. | Sebbah F, Chourak M, Ahalat M, Raiss M, Hrora Ael M, Benamer A, Laalim SA, Tounsi A. [Gastric duplication]. Presse Med. 2008;37:1506-1507. |
| 3. | Blinder G, Hiller N, Adler SN. A double stomach in an adult. Am J Gastroenterol. 1999;94:1100-1102. |
| 4. | Klimopoulos S, Gialvalis D, Marougas M, Zotos D, Orfanos N, Roussakis A, Argyriou P, Pantelidaki C. Unusual case of massive hemorrhage of a gastric duplication cyst in a very advanced age. Langenbecks Arch Surg. 2009;394:745-747. |
| 5. | Moss RL, Ryan JA, Kozarek RA, Hatch EI. Pancreatitis caused by a gastric duplication communicating with an aberrant pancreatic lobe. J Pediatr Surg. 1996;31:733-736. |
| 6. | Kaneko K, Ando H, Watanabe Y, Seo T, Harada T, Ito F. Gastric duplication communicating with the left hepatic duct: a rare case of recurrent hemobilia in a child. J Pediatr Surg. 1999;34:1539-1540. |
| 7. | Coit DG, Mies C. Adenocarcinoma arising within a gastric duplication cyst. J Surg Oncol. 1992;50:274-277. |
| 8. | Shinde T, Lindner J, Silverman J, Agrawal R, Dhawan M. Gastric-duplication cyst with an aberrant pancreatic-ductal system: an unusual cause of recurrent abdominal pain. Gastrointest Endosc. 2009;69:377-379. |
| 9. | Thurston SE, Lenn NJ. The association of spinal and gastroesophageal anomalies. Case report and review. Clin Pediatr (Phila). 1984;23:652-654. |