Published online Feb 7, 2010. doi: 10.3748/wjg.v16.i5.578
Revised: August 31, 2009
Accepted: September 7, 2009
Published online: February 7, 2010
AIM: To assess patients’ understanding for the reasons for taking 5-aminosalicylic acid or ursodeoxycholic acid as chemoprophylaxis against colorectal carcinoma associated with inflammatory bowel disease (IBD).
METHODS: A questionnaire-based study using a 5-point opinion scale was performed. One hundred and ninety-two patients with colitis only and 74 patients with primary sclerosing cholangitis and IBD were invited to take part.
RESULTS: Overall response rate was 58%. Sixty-four percent of patients claimed full concordance with chemoprophylaxis for maintenance of remission. Eighty-four percent of patients considered daily concordance during remission to be very important. Seventy-five percent stated they understood the reasons for taking the drugs. However, only 50% of the patients were aware of any link of their condition to bowel cancer. Seventy-nine percent of patients felt their concordance and understanding would be improved if they were informed of the chemoprophylactic potential of the medication.
CONCLUSION: Despite good self-reported concordance, half of the patients were unaware of an association between colitis and bowel cancer. Explaining the potential chemoprophylactic benefits may enhance patients’ overall concordance to 5-aminosalicylic acid and ursodeoxycholic acid and help maintain remission.
- Citation: Low A, Love M, Walt R, Kane K, Eksteen B, Goh J. Understanding of chemoprophylaxis and concordance in inflammatory bowel disease. World J Gastroenterol 2010; 16(5): 578-582
- URL: https://www.wjgnet.com/1007-9327/full/v16/i5/578.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i5.578
The risk of colorectal carcinoma (CRC) associated with inflammatory bowel disease (IBD) has long been established[1], increasing with the duration, extent and severity of inflammation. Primary sclerosing cholangitis (PSC) is known to be associated with colitis and an increased risk of CRC[2,3]. Over 60% of PSC patients have associated IBD, with associated increased risk of CRC as well as hepatocellular carcinoma. Five percent of patients with ulcerative colitis will go on to develop liver dysfunction, primarily cholestasis, of which 40% will develop PSC[4]. The risk of colorectal cancer in colitis patients has been estimated to be as high as 30% over 35 years in some populations[1]. There are similar rates of mucosal cell metaplasia and dysplasia in ulcerative colitis and Crohn’s colitis.
5-aminosalicylic acids (5-ASAs), for example mesalazine, are the most commonly prescribed anti-inflammatory drugs used in the management of IBD[5,6]. The evidence for their chemoprophylactic use in IBD is accumulating, including case control studies[7-10], prospective cohort studies[11,12], and a large UK based epidemiological study[5]. The use of ursodeoxycholic acid (UDCA) as a chemopreventative agent in PSC with ulcerative colitis is now accepted practice[13]. Chemoprophylaxis with these drugs is now part of core recommendations in the treatment of colitis published in guidelines, for example guidance issued by the British society of Gastroenterology[14]. The use of 5-ASA compounds for chemoprophylaxis in ulcerative colitis patients was considered to be evidence level 2 in recent guidance published by ECCO, and UDCA for PSC patients was considered to have an evidence level 1b[15].
Surveillance techniques for the detection of CRC and metaplastic cell changes are invasive endoscopic procedures. A systematic review of the available evidence concluded that while cancer was detected at an earlier stage through surveillance colonoscopy screening of colitis patients, there was no clear evidence of prolonged survival[16]. There was indirect evidence for screening programmes cost effectiveness, but the acceptability of colonoscopy to all patients remains an important prohibitive factor. It remains to be seen if novel techniques such as chromoendoscopy, confocal microscopy and emerging molecular markers can directly influence survival.
Chemoprophylaxis with 5-ASAs and UDCA as a means of reducing the risk of colorectal cancer to IBD and PSC/IBD patients is becoming an increasingly attractive concept. Current literature on drug concordance in IBD has been largely focussed on 5-ASA and factors influencing non-adherence[17-25]. Important factors identified include male gender, young age at diagnosis, occupation and depression[17,18]. The preparation and treatment regime for 5-ASA have also been highlighted as contributing to non-concordance and therefore poorer outcome[18-20]. All studies emphasize the importance of the physician-patient relationship and utilizing management strategies to reduce non-adherence. The concerns over 5-ASA preparations and dosing regimes are being addressed through the novel delivery of mesalazine as a once daily preparation[26,27]. Despite this and advancing knowledge of chemoprophylaxis, relatively little is known about patients’ understanding of the risk of developing colitis-associated CRC and the role of 5-ASA in reducing these risks. There is no doubt that patient education is important in not only establishing a good patient-physician working relationship, but also improving outcome through improved concordance with treatment regimes. More energy and strategies, such as the employment of specialist IBD nurse practitioners, are being used to educate patients about their conditions from the time of first diagnosis.
The aim of our study was to assess patients’ understanding of the risk of developing colitis-associated CRC and their understanding of the role of 5-ASA/UDCA as part of their treatment, as well as identifying means of improving overall concordance with chemoprophylaxis, through a qualitative questionnaire-based survey and patient feedback.
A simple patient questionnaire comprising of seven questions using a validated five-point opinion scale, was designed. The questionnaires were altered appropriately for the PSC/IBD patients giving two similar short questionnaires. Patients were also provided with clear written instruction on how to complete questions using a five-point opinion scale and contact details if they had any further queries. Finally, they were given the opportunity to provide feedback on proposed methods we could use to improve overall concordance as well as their own opinions on the matter.
The questions assessed disease activity, the importance patients assigned to daily concordance when both symptomatic and in remission, how often they forgot to take their medication, whether they understood the reasons for being on the medication, how well their doctor had explained the reasons for taking 5-ASA/UDCA and whether they were aware that 5-ASA/UDCA may help reduce the risk of developing CRC. PSC/IBD patients were also asked whether the UDCA was to treat their liver, bowel, or both to further assess how fully they understood reasons for taking UDCA daily. The patients’ opinions on ways of improving concordance were also sought. They were asked to rate how much the following proposals could improve concordance: a once-daily preparation, a clear explanation of the reasons for taking the medication and how it works from a health care professional, and being provided with evidence that 5-ASA/UDCA can reduce risk of CRC.
One hundred and ninety two patients with IBD (both Crohn’s disease and ulcerative colitis patients) receiving 5-ASAs were identified from our University Hospital Birmingham IBD database and a further 74 patients with PSC and associated IBD from our Liver Medicine department records were also included. The patients in the IBD group were in clinical remission at the time of the study. The PSC/IBD group were a post-liver transplant cohort with their colon intact.
Patients were given the questionnaires to complete on a voluntary basis when they attended the out-patient department clinics. All responses were anonymised for results analysis. Patients who were not given the opportunity to complete a questionnaire in the clinic were posted questionnaires with a stamped, addressed return envelope.
The questionnaire was approved by the hospitals Clinical governance board. Responses were processed and analysed by two of the authors using a standardised database.
Response rates were 59% (114/192) and 56% (42/74) for the IBD only and the IBD/PSC cohorts, respectively. Of the 42 patients in the IBD/PSC group who responded, 5 patients were excluded from further analysis as they were not taking UDCA (1 had never been prescribed it and 4 had stopped it due to side effects), making the total for subsequent analysis 37.
Sixty-four percent (98/151) of the total responders stated that they were fully concordant with 5-ASA/UDCA (60% IBD vs 78% IBD/PSC). Sixty-two percent of patients had had a flare up of symptoms in the past year, and of these, 67% reported full concordance with their medications, suggesting that disease activity may improve overall concordance.
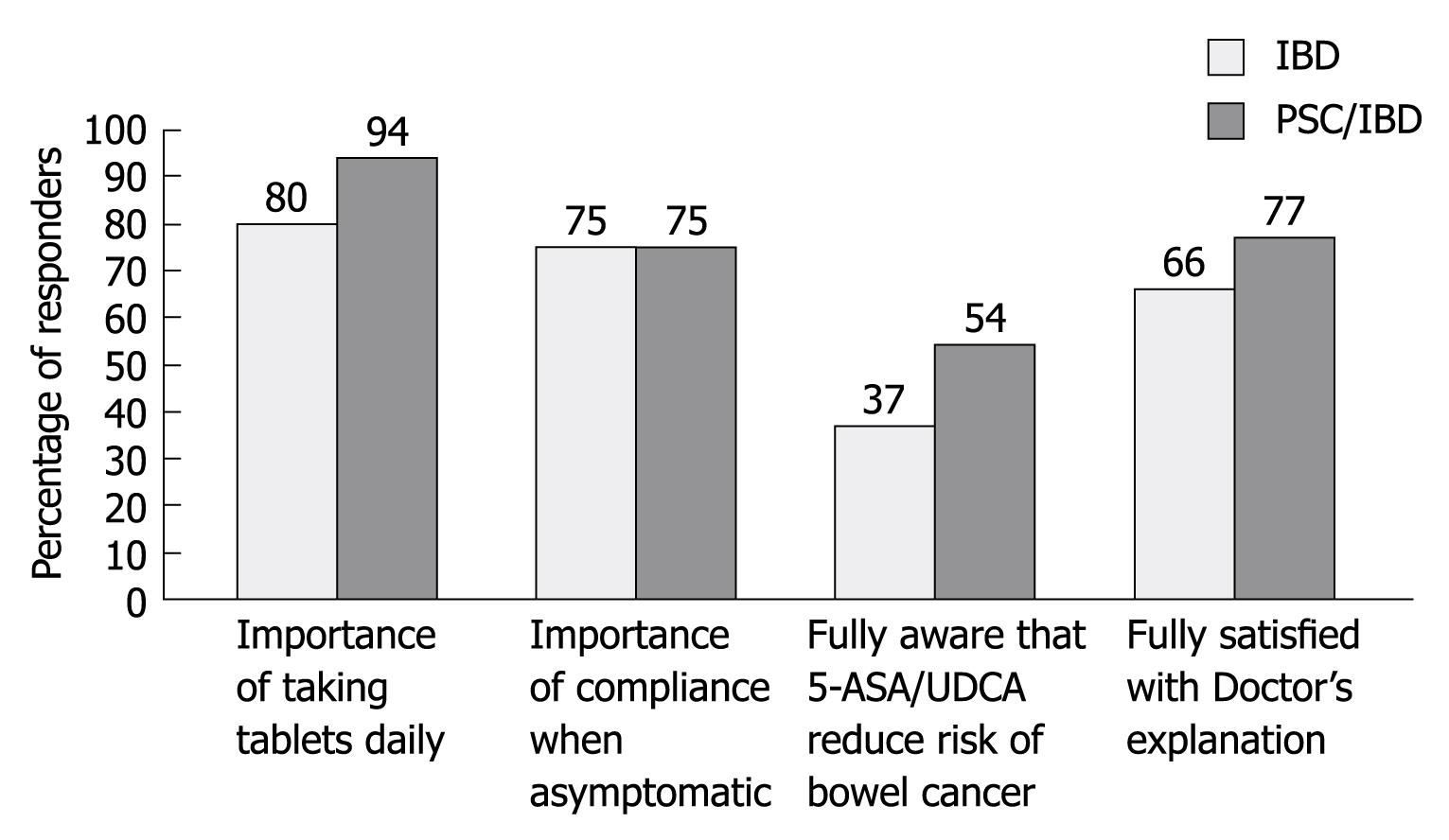
Eighty-four percent (126/151) of patients considered daily concordance to be very important and 75% (114/151) maintained concordance to be very important while in remission, stating that they fully understood the reasons for being prescribed the medications. Sixty-seven percent (101/151) of patients felt they had been given a full explanation by their doctor for 5-ASA/UDCA maintenance treatment (66% IBD vs 70% IBD/PSC). Twenty percent of patients had only received a partial explanation while 13% (12% IBD vs 16% IBD/PSC) felt they had received no explanation from either their doctor or any health professional. A bar chart comparing the responses of the IBD cohort to the PSC/IBD cohort is shown in Figure 1.
Despite 75% of patients claiming full understanding of the reasons for 5-ASA/UDCA maintenance treatment, 50% of the total cohort reported that they were completely unaware of any link between their condition and CRC (54% IBD vs 37% IBD/PSC). Of the IBD/PSC cohort, only 55% of patients were aware that UDCA is protective for both bowel and liver, suggesting the patients may not have been fully informed, despite 75% believing they fully understood the reasons for taking UDCA.
Of the three methods proposed to improve overall concordance in the future, 92% of patients agreed that a once daily preparation of 5-ASA would improve their overall concordance, 87% felt that a clear and full explanation from a health professional would be beneficial, and 94% felt that it would be helpful if they were given evidence that 5-ASA would help to reduce the risks of developing colitis-associated CRC.
Methods of improving patient concordance with 5-ASA/UDCA are proposed in Table 1. Table 2 contains samples of feedback patients gave of ways that their concordance to chemoprophylactic medications could be improved. Some salient examples include “Re-enforcement about why I’m on a treatment when it has been started and stopped in the past would be useful” and “newsletters and workshops on developments in research and treatment…”.
| Proposed method to improve concordance | Agree (%) | Disagree (%) |
| Given evidence 5-ASA/UDCA reduces CRC risk | 94 | 6 |
| Once a day preparation | 92 | 8 |
| Clear explanation from Health Professional | 87 | 13 |
| Difficult to remember when feeling well. Reminders would be useful |
| Unaware of reasons for taking the medication |
| Need reassurance regarding side effects |
| Full explanation, counselling and education on condition |
| Newsletters and workshops on developments in research and treatment |
| Re-enforcement about why on treatment when it has been started and stopped in the past |
| Unfortunately you cannot teach common sense if they do not stick to the prescribed dose there is not a lot you can do |
| Smaller, easier to take tablets |
Patients had a high self-reported level of concordance with their medications. Our study made no attempt to verify this through biochemical testing[22]. A study using urinary analysis identified 6 (12.7%) out of 47 patients who self reported full concordance tested negative for mesalamine or its metabolite[23,24]. We did not verify patients’ concordance against the frequency of pharmacy prescription collection. These results suggest that overall concordance in our patient group may be lower than claimed.
It is clear from patients’ responses that their understanding of the reasons for being on maintenance treatment and chemoprophylaxis is incomplete and that not all patients are fully informed about the risk of colitis-associated CRC. Patients need to have this information given to them by health professionals and reinforced by other resources. This information would also help IBD/PSC patients to better understand the need to continue their medication even when their condition is quiescent.
While the risk of CRC in IBD and PSC has been fully appreciated by health care professionals for decades, it is evident from our study that this knowledge is not being clearly communicated to patients. Potential obstacles may include time pressure in clinics, the physicians’ reluctance to discuss cancer potential with an asymptomatic patient, or patients not retaining this information. From our unpublished data, many patients undergoing regular colonoscopy surveillance for IBD are not fully aware of the cancer association and the potential need for colectomy in the event of dysplasia detection.
Patient education has been demonstrated to improve clinical outcome in the management of diabetes mellitus[28] and can easily be applied to IBD. The role of nurse practitioners in gastroenterology, in particular IBD, is evolving. An exceedingly useful resource, they work alongside gastroenterologists in the clinics and on the wards to educate patients on their condition and treatment[29]. Additional resources for patient education include patient information leaflets in a language that is easy to interpret, support groups and relevant websites.
Reassurance with regards to the safety, efficacy and side effect profile of these medications has also been identified by our patients as an important factor to improve concordance. This observation is in keeping with the study by Loftus et al[25], who also identified a lower pill burden and less frequent dosing as important. Ninety-two percent of patients in our study believed that a once daily preparation would improve concordance. Several once daily 5-ASA preparations are now available[26,27,30].
Optimising surveillance strategy using risk stratification and novel techniques coupled with advances in molecular markers may transform the way we manage this at-risk group. The emerging link between inflammation and cancer presents a very strong case for optimal disease control and chemoprophylaxis with 5-ASA and UDCA.
While the definitive randomised control study proving the benefit of chemoprophylaxis may remain elusive for the near future, the accumulating in vitro, in vivo and observational evidence are hard to ignore. To translate this into clinical benefit, it is important that physicians communicate these clinical rationales clearly to patients with IBD to improve the likelihood of them taking these medications even when they feel well.
Risk of colorectal neoplastic changes increase with length and duration of inflammation, making inflammatory bowel disease (IBD) and primary sclerosing cholangitis (PSC) patients particularly at risk of colorectal carcinoma. Management of these patients now includes chemoprophylaxis with 5-aminosalicylic acid and ursodeoxycholic acid during disease quiescence as well as symptomatic flare ups. These therapies are now endorsed in guidance on disease management such as that issued by the British Society of Gastroenterology and European Crohn’s and Colitis Organisation, and is therefore accepted clinical practice, yet little is known of patient’s understanding of why they are taking these therapies, their understanding of the risks of colorectal carcinoma associated with their condition and how their concordance to chemoprophylaxis may be improved.
Research is focussing on improved surveillance techniques and screening in this high risk group to try to ensure early detection of neoplastic changes. However, interventions have little impact on overall patient survival and acceptability of invasive screening procedures such as colonoscopy remains in doubt. Therefore, management focuses increasingly on chemoprophylaxis in the meantime.
Those prescribing chemoprophylaxis to IBD/PSC patients should take the time to explain to patients the reason for starting these therapies, even during times of disease quiescence, especially the fact that inflammation is associated with a higher chance of subsequent lower gastrointestinal carcinoma and that it is therefore important to minimise the risks with chemoprophylaxis. This information should not just be given at initial consultation, but should be regularly re-enforced to improve overall concordance with chemoprophylaxis. Specialist nurses have a key role in this educational aspect of disease management and patient education should be utilised for optimal results.
This paper is acceptable for publication with some revision.
Peer reviewer: Kiron M Das, MD, PhD, FACP, FRCP, Chief of Gastroenterology and Hepatology, Professor of Medicine, Director of Crohn's and Colitis Center of NJ, 1 Robert Wood Johnson Place, MEB Rm. 478, New Brunswick, NJ 08903, United States
S- Editor Cheng JX L- Editor O'Neill M E- Editor Lin YP
| 1. | Bernstein CN, Blanchard JF, Kliewer E, Wajda A. Cancer risk in patients with inflammatory bowel disease: a population-based study. Cancer. 2001;91:854-862. |
| 2. | Kornfeld D, Ekbom A, Ihre T. Is there an excess risk for colorectal cancer in patients with ulcerative colitis and concomitant primary sclerosing cholangitis? A population based study. Gut. 1997;41:522-525. |
| 3. | Vera A, Gunson BK, Ussatoff V, Nightingale P, Candinas D, Radley S, Mayer AD, Buckels JA, McMaster P, Neuberger J. Colorectal cancer in patients with inflammatory bowel disease after liver transplantation for primary sclerosing cholangitis. Transplantation. 2003;75:1983-1988. |
| 4. | Olsson R, Danielsson A, Järnerot G, Lindström E, Lööf L, Rolny P, Rydén BO, Tysk C, Wallerstedt S. Prevalence of primary sclerosing cholangitis in patients with ulcerative colitis. Gastroenterology. 1991;100:1319-1323. |
| 5. | van Staa TP, Card T, Logan RF, Leufkens HG. 5-Aminosalicylate use and colorectal cancer risk in inflammatory bowel disease: a large epidemiological study. Gut. 2005;54:1573-1578. |
| 6. | Travis SPL, Stange EF, Lémann M, Øresland T, Bemelman WA, Chowers Y, Colombel JF, D'Haens G, Ghosh S, Marteau P. European evidence-based Consensus on the management of ulcerative colitis: Current management. J Crohn's Colitis. 2008;2:24-62. |
| 7. | Eaden J, Abrams K, Ekbom A, Jackson E, Mayberry J. Colorectal cancer prevention in ulcerative colitis: a case-control study. Aliment Pharmacol Ther. 2000;14:145-153. |
| 8. | Pinczowski D, Ekbom A, Baron J, Yuen J, Adami HO. Risk factors for colorectal cancer in patients with ulcerative colitis: a case-control study. Gastroenterology. 1994;107:117-120. |
| 9. | Bernstein CN, Blanchard JF, Metge C, Yogendran M. Does the use of 5-aminosalicylates in inflammatory bowel disease prevent the development of colorectal cancer? Am J Gastroenterol. 2003;98:2784-2788. |
| 10. | Rutter M, Saunders B, Wilkinson K, Rumbles S, Schofield G, Kamm M, Williams C, Price A, Talbot I, Forbes A. Severity of inflammation is a risk factor for colorectal neoplasia in ulcerative colitis. Gastroenterology. 2004;126:451-459. |
| 11. | Bus PJ, Nagtegaal ID, Verspaget HW, Lamers CB, Geldof H, Van Krieken JH, Griffioen G. Mesalazine-induced apoptosis of colorectal cancer: on the verge of a new chemopreventive era? Aliment Pharmacol Ther. 1999;13:1397-1402. |
| 12. | Reinacher-Schick A, Seidensticker F, Petrasch S, Reiser M, Philippou S, Theegarten D, Freitag G, Schmiegel W. Mesalazine changes apoptosis and proliferation in normal mucosa of patients with sporadic polyps of the large bowel. Endoscopy. 2000;32:245-254. |
| 13. | Chan EP, Lichtenstein GR. Chemoprevention: risk reduction with medical therapy of inflammatory bowel disease. Gastroenterol. Clin North Am. 2006;35:675-712. |
| 14. | Guidelines for the Management of Inflammatory Bowel Disease in Adults. September 2004. British Society of Gastroenterologists. Accessed on April 16. 2008; Available from: http://www.bsg.org.uk/bsgdisp1.php?id=8be805c7ca570d72d9cd&h=1&sh=1&i=1&b=1&m=00023. |
| 15. | Biancone L, Michetti P, Travis S, Escher JC, Moser G, Forbes A, Hoffmann JC, Dignass A, Gionchetti P, Jantschek G. For the European Crohn’s and Colitis Organisation (ECCO). European evidence-based Consensus on the management of ulcerative colitis: Special situations. J Crohn's Colitis. 2008;2:63-92. |
| 16. | Collins PD, Mpofu C, Watson AJ, Rhodes JM. Strategies for detecting colon cancer and/or dysplasia in patients with inflammatory bowel disease. Cochrane Database Syst Rev. 2006;CD000279. |
| 17. | Ediger JP, Walker JR, Graff L, Lix L, Clara I, Rawsthorne P, Rogala L, Miller N, McPhail C, Deering K. Predictors of medication adherence in inflammatory bowel disease. Am J Gastroenterol. 2007;102:1417-1426. |
| 18. | Hawthorne AB, Rubin G, Ghosh S. Review article: medication non-adherence in ulcerative colitis--strategies to improve adherence with mesalazine and other maintenance therapies. Aliment Pharmacol Ther. 2008;27:1157-1166. |
| 19. | Bernal I, Domènech E, Garcia-Planella E, Marín L, Mañosa M, Navarro M, Cabré E, Gassull MA. Medication-taking behavior in a cohort of patients with inflammatory bowel disease. Dig Dis Sci. 2006;51:2165-2169. |
| 20. | Shale MJ, Riley SA. Studies of compliance with delayed-release mesalazine therapy in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18:191-198. |
| 21. | Kane SV. Systematic review: adherence issues in the treatment of ulcerative colitis. Aliment Pharmacol Ther. 2006;23:577-585. |
| 22. | Shaw IS, Jobson BA, Silverman D, Ford J, Hearing SD, Ball D, Johnson E, Day A, Probert CS. Is your patient taking the medicine? A simple assay to measure compliance with 5-aminosalicylic acid-containing compounds. Aliment Pharmacol Ther. 2002;16:2053-2059. |
| 23. | Cervený P, Bortlík M, Kubena A, Vlcek J, Lakatos PL, Lukás M. Nonadherence in inflammatory bowel disease: results of factor analysis. Inflamm Bowel Dis. 2007;13:1244-1249. |
| 24. | Kane SV, Cohen RD, Aikens JE, Hanauer SB. Prevalence of nonadherence with maintenance mesalamine in quiescent ulcerative colitis. Am J Gastroenterol. 2001;96:2929-2933. |
| 25. | Loftus EV Jr. A practical perspective on ulcerative colitis: patients' needs from aminosalicylate therapies. Inflamm Bowel Dis. 2006;12:1107-1113. |
| 26. | Sandborn WJ, Kamm MA, Lichtenstein GR, Lyne A, Butler T, Joseph RE. MMX Multi Matrix System mesalazine for the induction of remission in patients with mild-to-moderate ulcerative colitis: a combined analysis of two randomized, double-blind, placebo-controlled trials. Aliment Pharmacol Ther. 2007;26:205-215. |
| 27. | Kamm MA, Sandborn WJ, Gassull M, Schreiber S, Jackowski L, Butler T, Lyne A, Stephenson D, Palmen M, Joseph RE. Once-daily, high-concentration MMX mesalamine in active ulcerative colitis. Gastroenterology. 2007;132:66-75; quiz 432-433. |
| 28. | Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N. The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation. Health Technol Assess. 2003;7:iii, 1-iii190. |
| 29. | Read AM, Mayberry JF. Doctor or nurse? The patients' choice. Postgrad Med J. 2000;76:212-214. |