Published online Aug 28, 2010. doi: 10.3748/wjg.v16.i32.4112
Revised: May 16, 2010
Accepted: May 23, 2010
Published online: August 28, 2010
Prompt revascularization of the superior mesenteric artery (SMA) thrombotic occlusion can prevent intestinal infarction and decrease necrosis of the bowel segment. Herein, we describe two cases who underwent successful endovascular recanalization for acute SMA thrombosis using a primary aspiration thrombectomy because of possible consequent laparotomy for survey of bowel viability. The two patients had dramatic pain relief immediately after the procedure and remained symptom-free during the follow-up period.
- Citation: Yang HJ, Cho YK, Jo YJ, Jung YY, Choi SA, Lee SH. Successful recanalization of acute superior mesenteric artery thrombotic occlusion with primary aspiration thrombectomy. World J Gastroenterol 2010; 16(32): 4112-4114
- URL: https://www.wjgnet.com/1007-9327/full/v16/i32/4112.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i32.4112
Acute mesenteric ischemia (AMI) is a fatal vascular emergency, representing 1%-2% of acute abdominal emergencies, and develops from a sudden decreased perfusion to the intestines caused by occlusive or non-occlusive impairment of arterial or venous blood flow. The reported overall mortality of AMI is 60%-80%, and its incidence is increasing[1-3]. Superior mesenteric artery (SMA) embolism is the most frequent cause of AMI, which is responsible for approximately 40%-50% of cases[4]. Among the diagnostic tools, conventional angiography shows a complete obstruction of the proximal SMA, 1-2 cm away from the origin of SMA without collateral circulation, which correlates with acute obstruction, and needs relevant treatment[5,6]. We report two cases who underwent successful endovascular thrombolysis of AMI with different methods, despite the presence of early changes in bowel ischemia.
A 72-year-old man sought evaluation in the emergency room (ER) because of sudden aggravation of abdominal pain and rebound tenderness 3 d ago. He had a 2-year history of diffuse, dull postprandial abdominal pain. The attending physician suspected a surgical abdomen. The patient was on medication for hypertension during the last 16 years. Laboratory data showed no significant abnormalities.An initial abdominal computed tomography (CT) showed a segmental, occlusive acute thromboembolism in the mid-portion of the main stem, and jejunal and colic branches of SMA with circumferential bowel wall thickening and decreased enhancement of mucosal layer in the right colon.
Initial SMA angiography confirmed an acute occlusive thromboembolism in the mid-trunk of SMA and the origin of jejunal and colic branches of SMA (arrows) (Figure 1A). Initially, we performed primary aspiration thrombectomy using a 6F aspiration catheter (Cordis, Johnson and Johnson, San Diego, CA, USA) after IV infusion of 5000 IU heparin. Angiography after repetitive thrombectomy showed nearly complete thrombi removal from the SMA main trunk and its branches and residual focal severe stenosis in the mid-portion of SMA main stem (arrow) (Figure 1B), which was considered the leading cause of thromboembolism. Final angiogram showed completely restored perfusion to the ischemic bowel through the patent main stem, and jejunal and colic branches of SMA after implantation of a 6 mm × 18 mm balloon expandable stent (arrow) (Genesis; Cordis, Johnson and Johnson, San Diego, CA, USA) (Figure 1C). The patient’s symptoms improved almost immediately after the operation, and he no longer complained of postprandial abdominal pain. He was instructed to continue taking warfarin after discharge.
A 67-year-old man complained of acute abdominal pain 2 d after admission. The patient’s symptom was localized at the periumbilical area, and direct tenderness was present at physical examination. The patient had a history of atrial fibrillation and myocardial infarction, which was treated with coronary angioplasty 2 years ago.
Echocardiography showed a 30% ejection fraction and no evidence of thrombi in the left atrium. Laboratory data showed an elevated hs-CRP level of 14.22 mg/dL (normal range, 0-0.3 mg/dL).
Emergent CT angiography showed complete occlusion of the mid-portion of the main stem and origin of the ileocolic and right colic branches of SMA due to thromboembolism, with circumferential bowel wall thickening at the cecum and ascending colon. Surgical laparotomy was later considered because of heart failure.
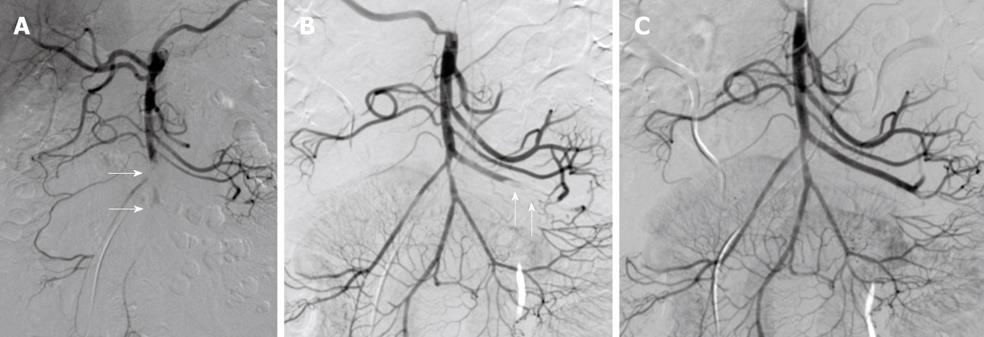
The initial SMA arteriography showed complete thrombotic occlusion of the mid to distal SMA trunk and the origin of ileocolic and right colic branches of SMA (arrows) (Figure 2A). Initially, we performed primary aspiration thrombectomy using a 6F aspiration catheter (Cordis, Johnson and Johnson, San Diego, CA, USA) after IV infusion of 5000 IU heparin. After repetitive aspiration thrombectomy, follow-up angiography showed that although most thrombi were removed from the SMA main trunk, small thrombi had a migrated and occluded distal portion of the jejunal branch of SMA during aspiration thrombectomy (arrows) (Figure 2B). Finally, most thrombi in the main stem and jejunal branch of SMA were completely removed immediately after an additional aspiration thrombectomy, and the lumen of SMA was completely recanalized (Figure 2C). After the procedure, the patient’s symptoms dramatically improved and the hs-CRP level decreased to 2.2 mg/dL, and he did not have recurrent symptoms during the 12-mo follow-up period.
AMI is caused by embolism (40%-50%), SMA thrombosis (20%-25%), non-occlusive mesenteric ischemia (20%), and mesenteric venous thrombosis (5%)[1-4]. Embolic or thrombotic occlusion of SMA frequently occurs on a background of generalized atherosclerotic changes in the involved arteries.
In our two cases, acute mesenteric thrombosis was managed with aspiration thrombectomy without any pharmacologic thrombolysis due to consequent laparoscopic survey to bowel.
Unfortunately, the non-specific symptoms are a frequent cause of delayed diagnosis, and most AMIs and CMIs can be asymptomatic for a long time. Contrast-enhanced CT can shows an arterial occlusion of SMA, frequently accompanied with severe stenosis of the celiac artery, and findings suggestive of bowel ischemia, including pneumatosis intestinalis, bowel wall thickening, ileus, and bowel dilatation[7]. Angiography can define the location and origin of the arterial occlusion and provide the potential for intervention if mesenteric ischemia is diagnosed prior to ischemic bowel necrosis[5,6]. Bloody diarrhea or signs of peritonitis, including abdominal rigidity and rebound tenderness, are signs of advanced bowel ischemia and bowel infarction, requiring urgent surgery. An area of transmural bowel necrosis in AMI can appear within 15 min after onset and after 6 h, and irreversible gangrene of the affected segments may ensue[8]. In our cases, the two patients were diagnosed with AMI by CT examination soon after the onset of symptoms. Although we performed endovascular treatment despite the presence of early ischemic bowel changes, such as bowel wall thickening and engorgement of the vasa recta, on initial or follow-up CT, we obtained good results as reflected by the dramatic improvement in symptoms.
Because of its favorable results, endovascular thrombolysis of acute SMA occlusion has gained popularity and has become one of the most used methods with or without combined open surgery[9]. Pharmacologic thrombolysis with or without mechanical aspiration thrombectomy is a good treatment option in terms of high survival, bowel preservation rates and low complication rate regardless of the nature of thromboembolism, period of occlusion, presence of collateral vessels and severe atherosclerotic disease.
The effect of primary aspiration thrombectomy for acute SMA thrombosis without pharmacologic thrombolysis remains a matter of debate and requires better definition. If consequent laparotomy is considered for assessment of bowel viability and use of anticoagulant is restricted due to a bleeding tendency, aspiration thrombectomy can be performed as the primary procedure. Despite contraindication or strict use of anticoagulant, a small amount of local anticoagulant use is mandatory for prevention of distal migration of small thrombi or recurrent thrombus formation.
Treatment of the underlying stenosis with angioplasty and stent implantation after intra-arterial thrombolysis has been described with at least good short-term results, but the higher restenosis rate of stents during follow-up has been reported in the recent literature[10]. We had a good short-term outcome, despite early ischemic changes, and continued long-term follow-up for recurring symptoms and restenosis of stents with CT angiography.
In conclusion, if the diagnosis of AMI is made early and there are no signs of advanced bowel ischemia, such as peritonitis, endovascular treatment for AMI. Primary aspiration thrombectomy can be performed for rapid and sufficient revascularization of acute thrombotic SMA occlusion in limited cases, consequent laparotomy must be planned to survey for bowel viability or if there is a contraindication to use an anticoagulant.
Peer reviewer: John K Marshall, MD, Associate Professor of Medicine, Division of Gastroenterology (4W8), McMaster University Medical Centre, 1200 Main Street West, Hamilton, Ontario L8N 3Z5, Canada
S- Editor Tian L L- Editor Wang XL E- Editor Ma WH
| 1. | Heys SD, Brittenden J, Crofts TJ. Acute mesenteric ischaemia: the continuing difficulty in early diagnosis. Postgrad Med J. 1993;69:48-51. |
| 2. | Barakate MS, Cappe I, Curtin A, Engel KD, Li-Kim-Moy J, Poon MS, Sandeman MD. Management of acute superior mesenteric artery occlusion. ANZ J Surg. 2002;72:25-29. |
| 3. | Björck M, Acosta S, Lindberg F, Troëng T, Bergqvist D. Revascularization of the superior mesenteric artery after acute thromboembolic occlusion. Br J Surg. 2002;89:923-927. |
| 4. | Berland T, Oldenburg WA. Acute mesenteric ischemia. Curr Gastroenterol Rep. 2008;10:341-346. |
| 5. | Demirpolat G, Oran I, Tamsel S, Parildar M, Memis A. Acute mesenteric ischemia: endovascular therapy. Abdom Imaging. 2007;32:299-303. |
| 6. | Wakabayashi H, Shiode T, Kurose M, Moritani H, Fujiki S, Morimoto N, Kusachi S. Emergent treatment of acute embolic superior mesenteric ischemia with combination of thrombolysis and angioplasty: report of two cases. Cardiovasc Intervent Radiol. 2004;27:389-393. |
| 7. | Chou CK, Mak CW, Tzeng WS, Chang JM. CT of small bowel ischemia. Abdom Imaging. 2004;29:18-22. |
| 8. | Gartenschlaeger S, Bender S, Maeurer J, Schroeder RJ. Successful percutaneous transluminal angioplasty and stenting in acute mesenteric ischemia. Cardiovasc Intervent Radiol. 2008;31:398-400. |
| 9. | Acosta S, Sonesson B, Resch T. Endovascular therapeutic approaches for acute superior mesenteric artery occlusion. Cardiovasc Intervent Radiol. 2009;32:896-905. |
| 10. | Lee RW, Bakken AM, Palchik E, Saad WE, Davies MG. Long-term outcomes of endoluminal therapy for chronic atherosclerotic occlusive mesenteric disease. Ann Vasc Surg. 2008;22:541-546. |