Published online Jun 7, 2010. doi: 10.3748/wjg.v16.i21.2702
Revised: March 3, 2010
Accepted: March 10, 2010
Published online: June 7, 2010
Acute cholecystitis is not a common complication of gastrectomy. Its clinical presentations and management strategies in old patients have not been well described in available literature. This report describes the clinical features, management strategies, and treatment outcome of acute cholecystitis immediately after gastrectomy. Acute cholecystitis immediately after gastrectomy in old patients has different clinical presentations, such as fever and high plasma C-reaction protein level. Abdominal computed tomography (CT) scan and ultrasonography showed acute cholecystitis in our cases, which was treated with antibiotics and ultrasound-guided percutaneous transhepatic gallbladder drainage (PTGD). The results indicate that abdominal CT scan and ultrasonography can effectively diagnose acute cholecystitis after gastrectomy, which can be effectively treated with antibiotics and PTGD.
- Citation: Liu XS, Zhang Q, Zhong J, Zhu KK, Mu YC, Yu JR. Acute cholecystitis immediately after radical gastrectomy: A report of three cases. World J Gastroenterol 2010; 16(21): 2702-2704
- URL: https://www.wjgnet.com/1007-9327/full/v16/i21/2702.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i21.2702
Radical gastrectomy is the main procedure for advanced gastric carcinoma. Acute cholecystitis following radical gastrectomy has been rarely reported[1], although bile stasis and gallbladder ischemia may occur after vagotomy and gastrohepatic ligament dissection[2]. Compared with acute cholecystitis in the general population, acute cholecystitis immediately after radical gastrectomy, a clinical situation not well-recognized in old patients, is characterized by a delayed diagnosis and a high mortality rate. In this paper, we report its clinical features, management strategies, and treatment outcomes of 3 old patients.
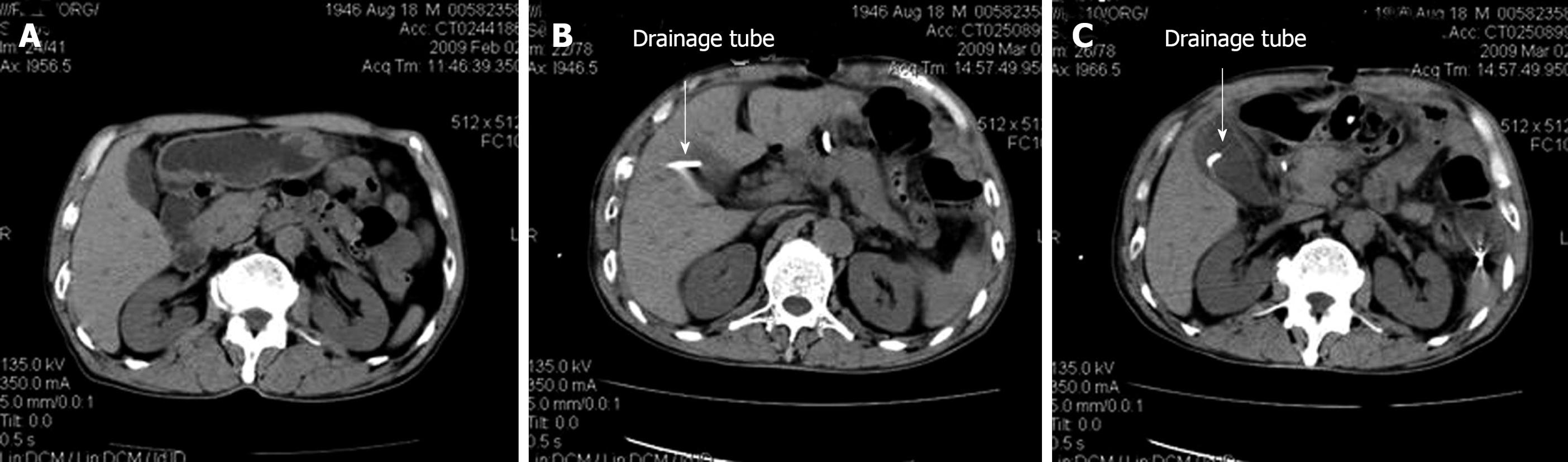
A 64-year-old Chinese female patient presented with upper abdominal discomfort and a 10 kg weight loss for 10 mo. Gastroscopy revealed an ulcerated tumor at the gastric antrum. Biopsy demonstrated a poorly- differentiated adenocarcinoma with no metastasis. This patient had no history of gallstones and cholecystitis. Preoperative computed tomography (CT) displayed a normal gallbladder (Figure 1A). Six days after distal gastrectomy, D2 lymphadenectomy and Billroth II reconstruction, she received enteral nutrition via a transnasal jejunal feeding tube. The patient had slight right abdominal and left shoulder pain but no fever and chilly on day 9 after operation. Physical examination showed right upper quadrant abdominal tenderness and muscle tension, but no rebound tenderness and Murphy’s sign. Laboratory test showed normal white blood cells (WBC) and neutrophils in peripheral blood, as well as normal amylase level and liver function. Abdominal ultrasound and CT scan on day 12 after operation demonstrated thickened gallbladder wall and biliary sludge deposition (Figure 1B). She was given intravenous antibiotics on day 12 after operation for 24 d. Her symptoms disappeared on day 24 after treatment with antibiotics. The patient was discharged 50 d after gastrectomy. Abdominal CT scan displayed a normal gallbladder (Figure 1C) without abdominal pain 7 mo after gastrectomy.
A 76-year-old Chinese male patient presented with melena for 6 mo. Gastroscopy showed an ulcerated tumor at the gastric antrum and biopsy demonstrated a moderately-differentiated adenocarcinoma with no metastasis. The patient had no history of gallstones and cholecystitis. Preoperative CT scan displayed a normal gallbladder (Figure 2A). Four days after distal gastrectomy, D2 lymphadenectomy and Billroth II reconstruction, he received enteral nutrition via a transnasal jejunal feeding tube. The patient developed high fever (39.4°C) and septic shock without abdominal pain on day 14 after operation. His plasma C-reaction protein (CRP) level was increased to 82.3 mg/L with normal WBC and neutrophils in peripheral blood as well as normal amylase level and liver function. Peripheral blood culture was positive for Escherichia coli. He received intravenous antibiotics on day 14 after operation for 6 d, but his body temperature did not become normal. Abdominal BUS and CT scan on day 15 after operation revealed thickened rough gallbladder wall (Figure 2B), and bile culture demonstrated Escherichia coli. Three days after ultrasound-guided percutaneous transhepatic gallbladder drainage (PTGD), his temperature returned to normal. He was discharged 30 d after gastrectomy.
A 64-year-old Chinese male patient presented with abdominal pain for 1 year. Gastroscopy showed a cardiac ulcerated tumor and biopsy demonstrated a poorly-differentiated adenocarcinoma with no metastasis. The patient had no history of gallstones and cholecystitis. Preoperative CT and BUS displayed a normal gallbladder. Four days after total gastrectomy, D2 lymphadenectomy and Roux-en-Y reconstruction, the patient received enteral nutrition via a transnasal jejunal feeding tube and developed severe right upper abdominal pain on day 14 after operation. Physical examination showed severe right upper abdominal tenderness. His body temperature was 38.8°C and plasma C-reaction protein (CRP) level was increased to 57.6 mg/L. The number of WBC in peripheral blood was 10.4 × 109/L with 82.1% of neutrophils. Abdominal BUS demonstrated thickened gallbladder wall with biliary sludge deposition on day 14 after operation and he underwent ultrasound-guided PTGD. Bile culture demonstrated Escherichia coli. His symptoms disappeared and body temperature decreased to 37.6°C on day 15 after operation. He was discharged 22 d after gastrectomy.
Acute cholecystitis immediately after radical gastrectomy has been rarely reported[3-5]. Although its pathogenesis is still unclear, it may result from ischemia of gallbladder and biliary stasis, impaired contractile motility of gallbladder after gastrectomy and vagotomy, digestive tract reconstruction, and long-time preoperative fasting[2-4]. Its clinical features are inconsistent with those of acute cholecystitis in general population. Since the symptoms of acute cholecystitis in old patients appear on days 9-14 after gastroectomy, its diagnosis is often delayed and physical findings may be confused with other postoperative complications, such as duodenal stump leakage, postanastomotic leakage, abdominal cavity infection and incisional discomfort. Acute cholecystitis immediately after radical gastrectomy differs significantly from that in general population. The majority of old acute cholecystitis patients have right upper quadrant pain, fever, leukocytosis, and high plasma CRP. Severe bacterial infection may be an exclusive sign of acute cholecystitis immediately after radical gastrectomy in old patients. Case 2 had bacteremia and septic shock but no abdominal pain and tenderness. Abdominal CT and BUS scan confirmed acute cholecystitis immediately after radical gastrectomy by revealing a thickened gallbladder wall, gallstones or gallbladder sludge, pericholecystic fluid and inflammation. In case 1, acute cholecystitis immediately after radical gastrectomy was confused with incisional discomfort, which was diagnosed by abdominal CT and BUS scan on day 3 after operation. It was reported that cholecystectomy, cholecystostomy, ultrasound-guided percutaneous drainage or percutaneous transhepatic gallbladder drainage are the treatment modalities for acute cholecystitis immediately after radical gastrectomy. However, these treatment modalities are still controversial because their efficiency and safety have not been well evaluated. The mortality rate of patients with acute cholecystitis immediately after radical gastrectomy is over 20%[1]. According to our experience with the 3 cases, ultrasound-guided PTGD should be considered for patients with acute cholecystitis immediately after gastrectomy. When physical findings and/or laboratory test reveal postoperative infection, abdominal CT and BUS scan should be performed to diagnose acute cholecystitis immediately after gastrectomy. Ultrasoun-guided PTGD, as a minimal invasive surgical approach, is an efficient and safe method for acute cholecystitis immediately after gastrectomy in old patients.
Peer reviewer: Michael Leitman, MD, FACS, Chief of General Surgery, Beth Israel Medical Center, 10 Union Square East, Suite 2M, New York, NY 10003, United States
S- Editor Tian L L- Editor Wang XL E- Editor Ma WH
| 1. | Oh SJ, Choi WB, Song J, Hyung WJ, Choi SH, Noh SH. Complications requiring reoperation after gastrectomy for gastric cancer: 17 years experience in a single institute. J Gastrointest Surg. 2009;13:239-245. |
| 2. | Takahashi T, Yamamura T, Utsunomiya J. Pathogenesis of acute cholecystitis after gastrectomy. Br J Surg. 1990;77:536-539. |
| 4. | Akatsu T, Yoshida M, Kubota T, Shimazu M, Ueda M, Otani Y, Wakabayashi G, Aiura K, Tanabe M, Furukawa T. Gallstone disease after extended (D2) lymph node dissection for gastric cancer. World J Surg. 2005;29:182-186. |