Published online Mar 21, 2010. doi: 10.3748/wjg.v16.i11.1425
Revised: January 15, 2010
Accepted: January 22, 2010
Published online: March 21, 2010
Liver tumor and other benign liver diseases such as polycystic liver disease can cause massive hepatomegaly and may represent an indication for liver transplantation (LT) in some instances. In this setting, LT can be extremely difficult and challenging due to its decreased mobility and access to vascular supply. Benefit from either a right or a left partial liver resection during the transplant procedure has been advocated to safely accomplish the hepatectomy of the native liver. Although we believe that partial hepatectomy adds some risk to intra-operative bleeding, we alternatively advise a different approach. We have a successful experience with LT in 6 massive hepatomegaly patients due to giant liver lesions. All the transplant procedures were performed without intermediate partial liver resection, showing that selective use of veno-venous bypass can play a significant role in the treatment of massive hepatomegaly.
- Citation: Gruttadauria S, di Francesco F, Gridelli B. Liver transplantation for polycystic liver and massive hepatomegaly. World J Gastroenterol 2010; 16(11): 1425-1426
- URL: https://www.wjgnet.com/1007-9327/full/v16/i11/1425.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i11.1425
We read with great interest the article of Jiang et al[1], published in last October in World Journal of gastroenterology 2009 October 28; 15 (40): 5112-5113 regarding a case of liver transplantation (LT) for polycystic liver with massive hepatomegaly. After an unsuccessful attempt to defenestrate the cyst, they performed hepatectomy for the native liver during LT accomplishing a left hepatectomy followed by a right hepatectomy because the massive hepatomegaly resulting from the enlarged liver cysts caused a very small surgical space, thus making the classic dissection of the hilar structures extremely difficult. Although we agree with the authors that the polycystic liver is not only large but also rigid, and consequently the mobility and access to vascular supply are decreased, we think that performing either a right or a left partial liver resection during LT adds some risk to intra-operative bleeding and we alternatively advise a different approach.
Indeed, we have some successful experience with LT in 6 patients with massive hepatomegaly due to giant liver lesions.
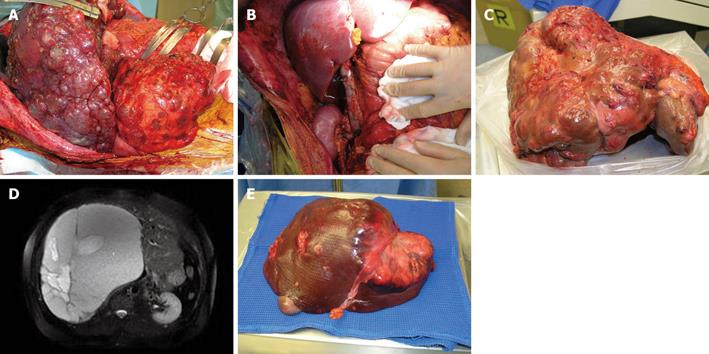
The primary indications for LT in 3 patients were polycystic kidneys and liver disease (Figure 1A), and two of them required a combined liver and kidney transplantation (Figure 1B) after bilateral nephrectomy.
LT was performed due to multifocal hepatocellular carcinoma (HCC) (Figure 1C), giant hepatic hemangioma (Figure 1D), and multiple metastases of carcinoid tumor (Figure 1E) for the 3 patients, respectively.
The recipient with giant multifocal HCC was obviously an exception to the Milan criteria (2) for LT in HCC patients.
After consulting our Internal Review Board, this patient was listed in a special list of potential recipients of “liver that nobody uses”[3]. All LT procedures were performed using cadaveric grafts except in 1 living case of right lobe donation in favor of the recipient with giant hemangioma.
The weight of all the explanted livers was more than 7 kg each (range: 5.440-10.000 g) and all the hepatectomies were extremely difficult because of the massive hepatomegaly.
In the HCC recipient and living donor, venous-venous bypass was performed during hepatectomy[4] and no systemic anti-coagulation occurred as previously described[5]. A standard hepatectomy technique instead of venous-venous bypass was used in the other 4 cases. Cystic defenestration was performed in the 6 cases using a large incision instead of thoracotomy for the spaces.
All the recipients had an uneventful post operative course and were alive at the time when they were followed up for 12 mo.
After two-disease free years, the HCC recipient developed a single bone lesion which was treated with selective radiotherapy.
We have never performed intermediate liver resection of massive hepatomegaly, because it may increase the risk of intra-operative bleeding.
We advise venous-venous bypass whether its access to vascular structures is difficult or impossible due to massive hepatomegaly.
Peer reviewer: Yasuhiko Sugawara, MD, Artificial Organ and Transplantation Division, Department of Surgery, Graduate School of Medicine University of Tokyo, Tokyo, Japan
S- Editor Tian L L- Editor Wang XL E- Editor Zheng XM
| 1. | Jiang WW, Zhang F, Pu LY, Wang XH, Kong LB. Liver transplantation for polycystic liver with massive hepatomegaly: a case report. World J Gastroenterol. 2009;15:5112-5113. |
| 2. | Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693-699. |
| 3. | Sotiropoulos GC, Paul A, Molmenti E, Lang H, Frilling A, Napieralski BP, Nadalin S, Treckmann J, Brokalaki EI, Gerling T. Liver transplantation for hepatocellular carcinoma in cirrhosis within the Eurotransplant area: an additional option with "livers that nobody wants". Transplantation. 2005;80:897-902. |
| 4. | Gruttadauria S, Marsh JW, Cintorino D, Biondo D, Luca A, Arcadipane A, Vizzini G, Volpes R, Marcos A, Gridelli B. Adult to adult living-related liver transplant: report on an initial experience in Italy. Dig Liver Dis. 2007;39:342-350. |