Published online Mar 14, 2010. doi: 10.3748/wjg.v16.i10.1296
Revised: December 28, 2009
Accepted: January 4, 2010
Published online: March 14, 2010
Infective colitis can be a cause of massive lower gastrointestinal bleeding requiring acute surgical intervention. Causative organisms include entamoeba and histoplasma species. However, concurrent colonic infection with both these organisms is very rare, and the in vivo consequences are not known. A 58-year-old male presented initially to the physicians with pyrexia of unknown origin and bloody diarrhea. Amoebic colitis was diagnosed based on biopsies, and he was treated with metronidazole. Five days later, the patient developed massive lower gastrointestinal bleeding with hemorrhagic shock. Emergency total colectomy with end-ileostomy was performed. However, he deteriorated and died on the second postoperative day. Histopathological examination revealed multiple deep ulcers at the hepatic flexure where fungal bodies of mycelial and yeast forms were noted. Isolated lymph nodes showed abscess formation with fungal bodies. Infective fungal colitis with Histoplasma capsilatum was diagnosed. In vitro, amoebic parasites can increase virulence and pathogenicity of histoplasma which may account for the fulminant presentation in this patient. Although rare, this unusual dual infection should be considered in the differential diagnosis of infective colitis, as appropriate antimicrobial treatment may prevent progression to massive lower gastrointestinal bleeding, obviating the need for urgent surgical intervention.
- Citation: Koh PS, Roslani AC, Vimal KV, Shariman M, Umasangar R, Lewellyn R. Concurrent amoebic and histoplasma colitis: A rare cause of massive lower gastrointestinal bleeding. World J Gastroenterol 2010; 16(10): 1296-1298
- URL: https://www.wjgnet.com/1007-9327/full/v16/i10/1296.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i10.1296
Massive lower gastrointestinal bleeding can be fatal and emergency surgery may be required. There are various etiologies leading to such a presentation, with infective colitis being one of the causes. Causative organisms in infective colitis include entamoeba, a parasite, and histoplasma, a dimorphic fungus. Both these organisms can be virulent individually, where mortality is estimated to be 50% in fulminant amoebic colitis, and mortality rates of 20%-25% are estimated in gastrointestinal histoplasma in those who are immunocompromised[1,2]. However, concurrent infection with both these organisms is very rare. We present a case of amoebic and histoplasmic colitis causing fatal massive lower gastrointestinal bleeding.
A 58-year-old male presented initially to the physicians with pyrexia of unknown origin for a month prior to admission. There was associated bloody diarrhea with loss of appetite and weight. There was no history to suggest any respiratory or urinary tract infection and he denied any high risk behavior. There was also no alteration in bowel habit prior to these symptoms.
Blood investigations were unremarkable except for elevated white cell count, erythrocyte sedimentation rate and C-reactive protein levels. Cultures were negative and stools did not show evidence of ova and cysts.
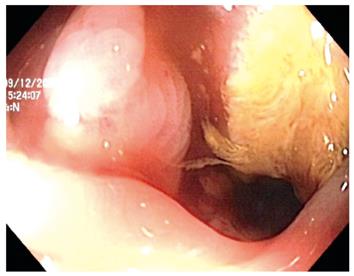
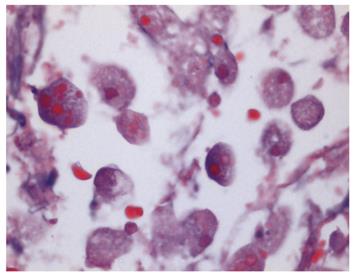
Colonoscopy revealed mucosal inflammation along the rectum and sigmoid interspersed with normal colonic mucosa, with further inflammation and ulcers seen along the hepatic flexure (Figure 1). There was no active bleeding noted. Amoebic colitis was diagnosed based on biopsies from colonoscopy (Figure 2), and he was treated appropriately with metronidazole.
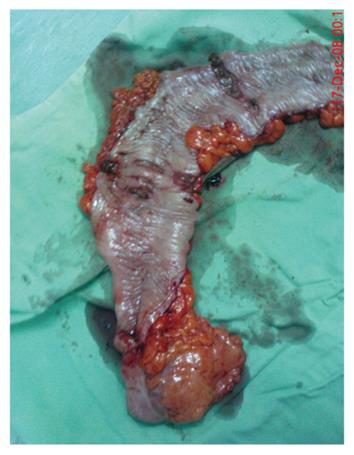
Five days later, the patient developed massive lower gastrointestinal bleeding with hemorrhagic shock. Resuscitation was commenced but he remained unstable and underwent emergency laparotomy. A total colectomy (Figure 3) with end-ileostomy was performed. Mesenteric lymphadenopathy was noted intra-operatively. His condition deteriorated postoperatively with subsequent disseminated intravascular coagulopathy. The patient died on the second postoperative day.
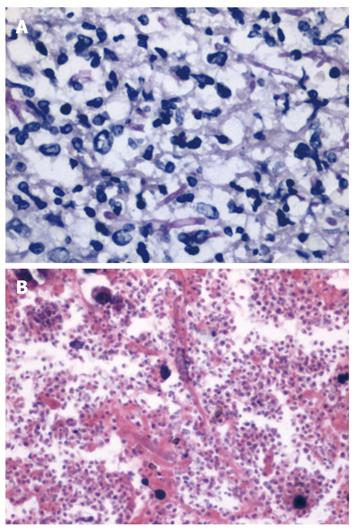
Histopathological examination revealed multiple deep ulcers into the muscularis propria at the hepatic flexure, where fungal bodies with mycelial and yeast formations were seen (Figure 4). Abscesses were also seen in the submucosal and serosal layers containing fungal bodies of yeast form. Isolated lymph nodes showed abscess formation with fungal bodies (yeast form). There was no evidence of malignancy or residual amoebic parasites. Infective fungal colitis with Histoplasma capsulatum was diagnosed.
Infective colitis can be severe and fatal. The spectrum of clinical presentation ranges from an asymptomatic state, a mild form with symptoms such as abdominal pain, fever or diarrhea, to a severe state which may result in gastrointestinal bleeding or colonic perforation[3-5]. When presenting with massive gastrointestinal bleeding, surgery is warranted[6].
Appropriate therapy with antimicrobials is vital in the treatment of infective colitis. Metronidazole had been shown to be effective in treatment of amoebic colitis[4]. Despite a negative stool culture and examination as seen in our case, the endoscopic biopsy was positive, and this had been shown to be most effective in diagnosing amoebic infection[7,8]. It is also interesting to note skip colonic ulcerative lesions were present on our endoscopic findings, which may suggest an inflammatory bowel disease. One tends to associate their appearance with Crohn’s colitis but skip lesions in infective colitis does occur[9,10].
Histoplasma infection is an endemic mycosis commonly found in North and Central America, and complete recovery has been well documented with the use of antifungal therapy such as amphotericin B or itraconazole[11,12]. Isolated gastrointestinal histoplasmosis is rare as it is usually asymptomatic with clinical manifestation occurring in less than 5% of the population, though it may be more common in those who are immunocompromised[12-14].
In our case, concurrent histoplasmic infection was initially unsuspected, which may have caused progression to the severe end of the clinical spectrum. In vitro tests have shown that amoebic parasites may contribute to the virulence or pathogenic traits of histoplasma[15].
Concurrent colonic infection with both amoeba and histoplasma has not been documented in the literature to our knowledge, although it has been reported in lung infections[15]. The above case presents to us as a very rare form of colitis, which was eventually fatal.
In conclusion, massive lower gastrointestinal bleeding warrants urgent surgical intervention. Infective colitis, especially with this unusual dual infection, as a cause of such a presentation is rare, but should be considered in the differential diagnosis.
Peer reviewer: Dr. Paulino Martínez Hernández Magro, Department of Colon and Rectal Surgery, Hospital San José de Celaya, Eje Vial Norponiente No 200-509, Colonia Villas de la Hacienda, 38010 Celaya, México
S- Editor Wang JL L- Editor Cant MR E- Editor Ma WH
| 1. | Li E, Stanley SL Jr. Protozoa. Amebiasis. Gastroenterol Clin North Am. 1996;25:471-492. |
| 2. | Assi M, McKinsey DS, Driks MR, O’Connor MC, Bonacini M, Graham B, Manian F. Gastrointestinal histoplasmosis in the acquired immunodeficiency syndrome: report of 18 cases and literature review. Diagn Microbiol Infect Dis. 2006;55:195-201. |
| 3. | Gironés Vila J, Roig García J, Codina Cazador A, Masvidal Calpe R, García Oria M, Codina Barreras A, Pérez Bueno F. [Low digestive hemorrhage caused by amebic colitis]. Rev Esp Enferm Dig. 1996;88:223-225. |
| 4. | Wandono H. Colitis amebiasis with symptom of occasional dripped anal bleeding. Acta Med Indones. 2007;39:183-185. |
| 5. | Deshpande RB, Bharucha MA, Modhe JM, Bhalerao RA. Necrotising arteritis in amoebic colitis. J Postgrad Med. 1992;38:151-152. |
| 6. | Eggleston FC, Verghese M, Handa AK. Amebiasis causing massive gastrointestinal bleeding. Arch Surg. 1978;113:1472. |
| 7. | Jammal MA, Cox K, Ruebner B. Amebiasis presenting as rectal bleeding without diarrhea in childhood. J Pediatr Gastroenterol Nutr. 1985;4:294-296. |
| 8. | Rozen P, Baratz M, Rattan J. Rectal bleeding due to amebic colitis diagnosed by multiple endoscopic biopsies: report of two cases. Dis Colon Rectum. 1981;24:127-129. |
| 9. | Clarkston WK, Bonacini M, Peterson I. Colitis due to Histoplasma capsulatum in the acquired immune deficiency syndrome. Am J Gastroenterol. 1991;86:913-916. |
| 10. | Wong SY, Ng FH, Kwok KH, Chow KC. Skip colonic ulceration in typhoid ileo-colitis. J Gastroenterol. 1999;34:700-701. |
| 11. | Buhk T, Stellbrink HJ, Albrecht H, Sobottka I. [Severe colitis due to Histoplasma capsulatum in an AIDS patient]. Z Gastroenterol. 2006;44:603-607. |
| 12. | Aubry P, Hovette P. [Digestive disorders in histoplasmosis. Report of a case of ulcerous enterocolitis caused by Histoplasma capsulatum (author’s transl)]. Med Trop (Mars). 1981;41:207-213. |
| 13. | Jain S, Koirala J, Castro-Pavia F. Isolated gastrointestinal histoplasmosis: case report and review of the literature. South Med J. 2004;97:172-174. |
| 14. | Averbach M, Cutait R, Corrêa P, Duarte MI, Leite K, Borges JL. [Colorectal diseases in AIDS patients and endoscopic findings]. Arq Gastroenterol. 1998;35:104-109. |
| 15. | Steenbergen JN, Nosanchuk JD, Malliaris SD, Casadevall A. Interaction of Blastomyces dermatitidis, Sporothrix schenckii, and Histoplasma capsulatum with Acanthamoeba castellanii. Infect Immun. 2004;72:3478-3488. |