Published online Jan 7, 2010. doi: 10.3748/wjg.v16.i1.63
Revised: September 7, 2009
Accepted: September 14, 2009
Published online: January 7, 2010
AIM: To evaluate the Z-line visualization by the PillCam™ SB2 using three different ingestion protocols.
METHODS: Ninety consecutive patients undergoing small bowel capsule endoscopy (SBCE) between January and May 2008 were included in the study. They swallowed the capsule in the standing (Group A = 30), supine (Group B = 30) and right supine positions (Group C = 30). Baseline patient characteristics, difficulties in capsule ingestion, esophageal transit times (ETT) and Z-line visualization were noted.
RESULTS: No significant differences were found between the groups with regard to baseline patient characteristics, ingestion difficulties and complete SB examinations (P > 0.05). At least 1 frame of the Z-line was detected in 15.8%, 46.7% and 90% of patients in groups A, B and C, respectively (P < 0.001). The average number of Z-line images was 0.21 ± 0.53, 3.23 ± 6.59 and 5.53 ± 7.55 and the mean % of the Z-line detected was 71.3, 25.1 and 8.3, in groups A, B and C, respectively (both P < 0.001). ETT times were longer in the supine group followed by the right supine and the standing groups (median of 237 s vs 64 s and 39 s, respectively; P < 0.001).
CONCLUSION: Z-line visualization in patients undergoing SBCE can be accurately achieved in most cases when the capsule is swallowed in the right supine position.
- Citation: Fernandez-Urien I, Borobio E, Elizalde I, Irisarri R, Vila JJ, Urman JM, Jimenez J. Z-line examination by the PillCam™ SB: Prospective comparison of three ingestion protocols. World J Gastroenterol 2010; 16(1): 63-68
- URL: https://www.wjgnet.com/1007-9327/full/v16/i1/63.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i1.63
Small bowel examination has recently become possible because of emerging procedures such as capsule endoscopy. As demonstrated by previous studies, capsule endoscopy is an accurate, easy and safe method which allows examination of the entire small bowel in most cases[1-3]. Moreover, capsule endoscopy has been demonstrated to be more effective than small bowel follow-through and push-enteroscopy for small bowel examination[4-8]. Nevertheless, images and lesions outside the small bowel (i.e. esophagus, stomach and colon) can also be detected by the capsule[9-11]. These images or lesions are sometimes missed by conventional endoscopy[12,13] which means that non-small bowel segments of capsule videos should be carefully reviewed by physicians. As the small bowel capsule is usually swallowed in the standing position, the esophageal transit time becomes very short resulting in few images taken in the esophagus. Recent advances in capsule designs have demonstrated that an accurate examination of the esophagus is feasible[14-18]. In fact, the esophageal capsule is swallowed by the patient in the supine or right supine positions in order to increase esophageal transit time allowing the capsule to take more images in the esophagus. However, the esophageal capsule battery lasts 20 min on average, which means that only upper gastrointestinal segments, usually including the esophagus and stomach, can be examined. Since the small bowel capsule has longer battery time, the esophagus in addition to the stomach, small bowel and colon, could be explored. Whether esophageal mucosa can be accurately explored by the small bowel capsule in the supine and right supine positions has not been previously studied. The aims of this study were to evaluate and compare the Z-line visualization by the PillCam™ SB in patients undergoing small bowel capsule endoscopy using three different ingestion protocols: standing, supine and right supine positions.
This study was conducted at a single hospital between January and May 2008. All patients who were not contraindicated to undergo capsule endoscopy, despite procedure indications, were suitable for inclusion in the study. Exclusion criteria were: age < 18 years, swallow and or esophageal motility disorders and previous prokinetic drugs administration. Patients were randomized, by means of computer-generated random numbers, to swallow the capsule in one of the three different positions: standing (Group A), supine (Group B) and right supine position (Group C).
All capsule procedures were performed with the PillCam™ SB2 (Given Imaging Ltd; Yoqneam, Israel). Two CE-experienced gastroenterologists (Fernandez-Urien I and Borobio E) reviewed the videos helped by the latest version of the program RAPID® 5.1.
All patients underwent capsule endoscopy after an 8-h fast. Prokinetics, laxatives or simethicone were not used, and all patients were asked to drink 100 mL of water before capsule ingestion in order to clear the esophagus of secretions. They were also kindly asked not to talk during the ingestion procedure.
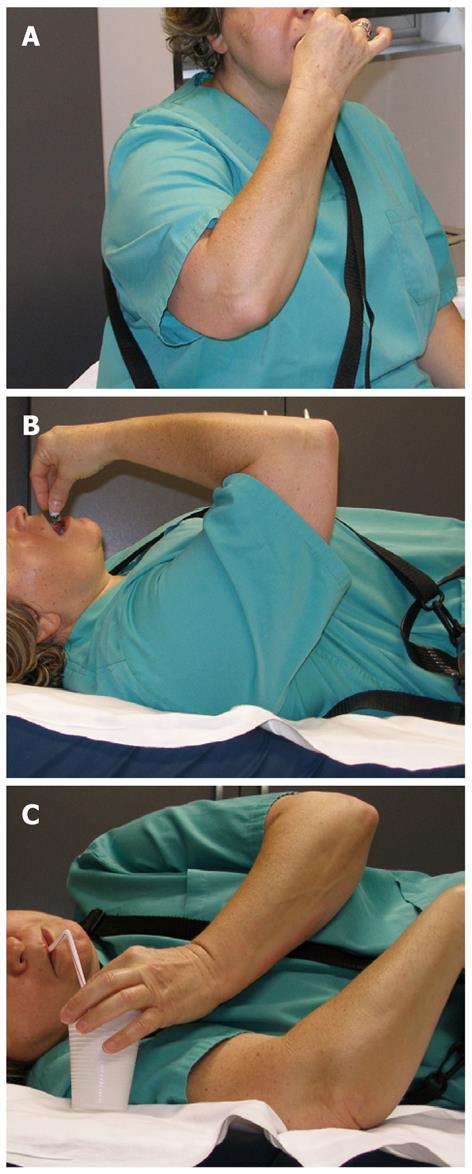
Standing position (Figure 1A): Patients from Group A were asked to swallow the capsule in the standing position with a small amount of water if required (no more than 20 mL).
Supine position (Figure 1B): Patients from Group B were asked to swallow the capsule in the supine position with a small amount of water if required (no more than 20 mL). They remained in this position for two min and then they were raised to an inclination of 30 degrees for 2 min and 60 degrees for additional 1 min in order to facilitate the transit of the capsule through the esophagus. Then, all patients were asked to drink a small sip of water (10 mL), allowed to sit upright and then asked again to drink 10 mL of water (in order to ensure complete esophageal examinations).
Right supine position (Figure 1C): Patients from Group C were asked to swallow the capsule in the right supine position with a small amount of water if required (no more than 20 mL). They remained in this position for 7 min and then were asked to drink small sips of water (10 mL) every 30 s helped by a flexible straw in order to ensure that the capsule reached the distal part of the esophagus. After that, all patients were allowed to sit upright and asked to drink 10 mL of water (in order to ensure complete esophageal examinations).
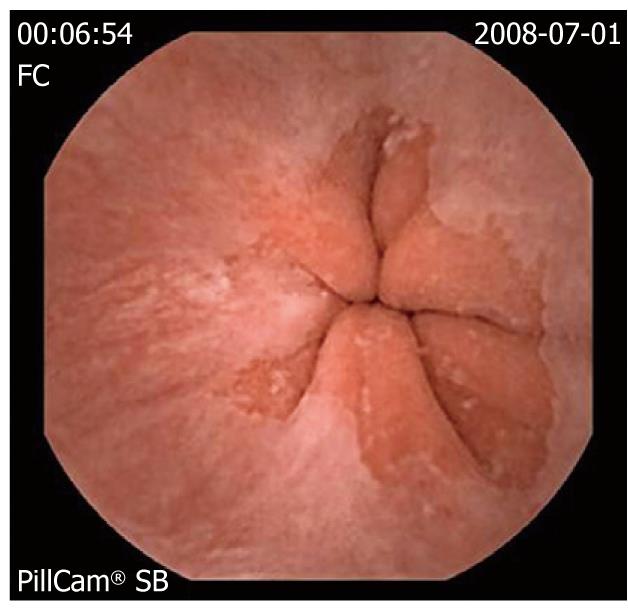
Baseline patient characteristics, difficulties in capsule ingestion, esophageal transit times (from mouth to stomach) and Z-line visualization were prospectively noted. Difficulties in capsule ingestion were classified as follows: easy when the capsule was swallowed before 1 min and without nausea, difficult when the capsule was swallowed after 1 min and/or with nausea, and impossible when the capsule was not swallowed by the patient. The Z-line visualization was measured on screen using a 4-quadrant scale (Figure 2).
Sample size estimation is not possible in the absence of data regarding the incidence of Z-line visualization with the PillCam™ SB2 ingested in the supine and right supine positions. However, assuming an incidence of Z-line visualization of 10% in the standing position, 35% in the supine position and 70% in the right supine position, 30 patients would be required in each group to detect significant differences (with α level set at 0.05 and β at 95%).
Data from quantitative variables which did not follow a Gaussian distribution are presented as median and interquartile range (IQR) and compared using the Kruskal-Wallis and the Mann-Whitney tests. Those data from quantitative variables which followed a Gaussian distribution are presented as mean and standard deviation and compared using ANOVA and Tamhane tests (for post-hoc comparisons, if needed). Qualitative variables (presented as simple proportions) and proportions are compared using the Pearson-Fischer χ2 tests. Statistical analysis was performed with SPSS version 15.0 (SPSS Inc; Chicago, Ill, USA). Values of P < 0.05 were considered to be statistically significant.
Baseline patient characteristics are shown in Table 1. There were no statistically significant differences in age, gender, body mass index (BMI), procedure indication and outpatient setting between groups A, B and C (P > 0.05).
Capsule ingestion was possible in all patients (results of capsule ingestion are summarized in Table 2). Capsule ingestion was easy in more than 90% of the patients in all positions. No significant differences were observed between groups A, B and C (P > 0.05).
Esophageal transit times were significantly longer in the supine group followed by the right supine and the standing groups [median (IQR) of 237 s (80-474), 64 s (40-108) and 39 s (24-55), respectively; P < 0.001]. Post-hoc comparisons showed that the differences group by group were also statistically significant (P < 0.05) (Table 3).
Table 4 shows the results concerning Z-line visualization in the standing, supine and right supine positions. At least one image of the Z-line was detected by the capsule in 15.8%, 37.3% and 90% of patients when the capsule was swallowed in the standing, supine and right supine positions, respectively (P < 0.001). Post-hoc comparisons showed that the differences found group by group were also significant (P < 0.05). The Z-line was detected by the capsule in 5.5 ± 7.5, 3.2 ± 6.5 and 0.2 ± 0.5 frames per procedure in the right supine, supine and standing groups. Although these differences were significant (P < 0.05), post-hoc comparisons showed that only the differences between the standing and the right supine groups were significant (P < 0.05). The mean % of Z-line detected by the capsule was 71.3% in the right supine group, 25.1% in the supine group and 8.6% in the standing group. These differences were also significant (P < 0.001) but post-hoc comparisons group by group demonstrated that the differences between the standing and the supine group were not significant (P > 0.05).
| Group A (standing) | Group B (supine) | Group C (right supine) | P value | |
| % | 4/30 (15.8%) | 11/30 (37.3%) | 27/30 (90%) | < 0.0011 |
| Mean % Z-line | 8.68 ± 22.96 | 25.16 ± 34.52 | 71.33 ± 33.47 | < 0.0012 |
| Mean frames | 0.21 ± 0.53 | 3.23 ± 6.59 | 5.53 ± 7.55 | 0.0172 |
| Standing vs supine | Standing vs right supine | Supine vs right supine | ||
| % patients | P = 0.0273 | P < 0.0013 | P < 0.0013 | (-) |
| Mean % Z-line | NS4 | P < 0.0014 | P < 0.0014 | (-) |
| Mean frames | NS4 | P = 0.0024 | NS4 | (-) |
The cecum was reached by the capsule in 89.5%, 86.2% and 96.7% of cases in the standing, supine and right supine positions, respectively. These differences were not statistically significant (P > 0.05).
Wireless capsule endoscopy has opened a new era for small bowel examination. In fact, more than 500 000 capsule procedures have been performed worldwide. Capsule endoscopy offers excellent images of the small bowel but also from the esophagus, stomach and colon in most cases. As demonstrated by some previous studies[12,13], non-small bowel lesions detected by capsule endoscopy are sometimes missed by conventional endoscopy which means that non-small bowel segments of capsule videos should be carefully reviewed by physicians. However, esophageal examination with the PillCam™ SB has been demonstrated not to be feasible in the standing position[19] but possible in the supine and right supine positions as shown with the PillCam™ ESO capsule[14-18]. Esophageal images taken by the capsule when it is swallowed in the standing position are not usually enough in terms of number and quality. Since the first small bowel examinations, capsule endoscopy has been performed in the standing position in most institutions and the reason for this seems to be simple, to reach the duodenum as soon as possible to ensure complete small bowel examinations. Currently, the rate of complete examinations is up to 80% in published series[20] and it depends on factors such as previous abdominal surgery, patient hospitalization and diabetes. Although there are no references in the literature, it seems that capsule ingestion in the standing position does not improve the rate of complete examinations. Moreover, there is a recent study which concludes that the right supine position after capsule ingestion improves the rate of complete examinations[21]. Thus, there are no specific reasons to perform small bowel capsule endoscopy in the standing position.
The main objective of our study which was to analyze the Z-line visualization with the PillCam™ SB in the supine and right supine positions has not been previously analyzed. This new modality of the small bowel capsule endoscopy procedure could optimize the capsule resources without affecting small bowel examinations and patients’ tolerability. In fact, we did not find significant differences in the rate of complete small bowel examinations and patients’ swallowing difficulties despite their positions during capsule ingestion. Capsule ingestion in the right supine position was significantly more effective for Z-line visualization than the standing and supine positions. On the one hand, our results showed that the Z-line was detected in most patients who swallowed the capsule in the right position. On the other hand, the frequency and the quality of Z-line images taken by the capsule were greater in the right supine position than in the standing and supine positions. Although in some patients it was not completely visualized by the capsule in the right supine position, the Z-line was detected more than 5 times per procedure on average. Therefore, it seems reasonable to affirm that the Z-line was almost completely visualized in most cases. These results are consistent with those previously obtained by esophageal capsule endoscopy[22,23].
Surprisingly, esophageal transit times which were significantly longer in the supine group did not affect the Z-line visualization. More time in the esophagus did not mean more and better images from the Z-line. A reasonable explanation for this may be the position of the His angle at the gastroesophageal junction. While the capsule remains too long in the mid and distal esophagus but far away from the Z-line when is swallowed in the supine position, it rapidly reaches the distal esophagus but is kept by the His angle over the Z-line for several seconds in the right supine position. Therefore, the right supine position seems to be anatomically optimal for Z-line examination. Moreover, a previous study by Gralnek et al[22] in healthy volunteers using the PillCam™ ESO, tested several ingestion procedures including standing, supine, right supine and left supine positions, concluding that the right supine position was the best approach to explore the distal esophagus.
Several studies have previously evaluated the feasibility of capsule endoscopy in the evaluation of the esophagus, however, the majority of them employed the PillCam™ ESO. The PillCam ESO and the ESO2 offer excellent images of more than 75% of the Z-line in most patients[22,23]. However, to our knowledge, there is only one study which has evaluated the role of the small bowel capsule for esophageal examinations[19]. In that study, an adequate assessment of the Z-line (50% and 100% of the circumference) was achieved in 10.4% and 0% of patients in the standing position and in 12.5% and 37.5% of patients in the supine position. Therefore, the authors concluded that esophageal examinations using small bowel capsule endoscopy was not feasible. Our results in patients who swallowed the capsule in the standing and supine positions are consistent with those obtained in that study, however, those authors did not include the right supine position as an additional comparative arm.
In this situation, the main question is: should all patients undergoing capsule endoscopy, despite indications, swallow the capsule in the right supine position? The answer is probably yes, because this alternative is easy to perform, is not uncomfortable for the patient, is not time consuming for physicians and the most importantly, it offers excellent images of the Z-line in most cases. However, the PillCam™ SB has to demonstrate that it is accurate in detecting esophageal lesions such as gastroesophageal reflux disease (GERD) lesions or varices. Other capsule prototypes such as the PillCam ESO capsule have demonstrated a high diagnostic accuracy for detecting GERD lesions, Barrett’s esophagus and esophageal varices[14-16]. Nevertheless, it has to be taken into account that this capsule prototype takes 14 images per second and the PillCam SB, only 2 per second. Therefore, future studies in patients with suspected esophageal diseases should be performed. If favourable results are obtained, then this alternative should be used in all capsule procedures including small bowel, colon and of course, esophageal examinations.
Capsule endoscopy has become a very important tool for small bowel examination. However, images from other parts of the gastrointestinal (GI) tract, can also be detected by the capsule. These images or lesions are sometimes missed by conventional endoscopy, which means that images from the esophagus, stomach and colon should be carefully reviewed.
Esophageal examination is not feasible if the capsule is ingested in the standing position as shown by previous studies. With recent prototypes designed for esophageal examination, new ingestion protocols have been evaluated. The supine and right supine positions have been demonstrated to be good positions to achieve a good esophageal examination. Whether the small bowel capsule is capable of examining the esophagus in these positions has not been previously studied.
This study demonstrates that the PillCam SB can accurately explore the Z-line when it is ingested in the supine and right supine positions.
Esophageal examination could be of interest in those patients who undergo capsule endoscopy of the small bowel. Missed lesions in the esophagus by conventional endoscopy could be detected by the capsule if it is ingested in the right supine position.
This study demonstrate that Z-line examination is those patients undergoing small bowel capsule endoscopy is feasible if the capsule is ingested in the right supine position.
Peer reviewer: Francis Seow-Choen, Professor, Seow-Choen Colorectal Centre, Mt Elizabeth Medical Centre, Singapore, 3 Mt Elizabeth Medical Centre #09-10, Singapore 228510, Singapore
S- Editor Li LF L- Editor Webster JR E- Editor Lin YP
| 2. | Appleyard M, Glukhovsky A, Swain P. Wireless-capsule diagnostic endoscopy for recurrent small-bowel bleeding. N Engl J Med. 2001;344:232-233. |
| 3. | Lewis BS, Swain P. Capsule endoscopy in the evaluation of patients with suspected small intestinal bleeding: Results of a pilot study. Gastrointest Endosc. 2002;56:349-353. |
| 4. | Appleyard M, Fireman Z, Glukhovsky A, Jacob H, Shreiver R, Kadirkamanathan S, Lavy A, Lewkowicz S, Scapa E, Shofti R. A randomized trial comparing wireless capsule endoscopy with push enteroscopy for the detection of small-bowel lesions. Gastroenterology. 2000;119:1431-1438. |
| 5. | Costamagna G, Shah SK, Riccioni ME, Foschia F, Mutignani M, Perri V, Vecchioli A, Brizi MG, Picciocchi A, Marano P. A prospective trial comparing small bowel radiographs and video capsule endoscopy for suspected small bowel disease. Gastroenterology. 2002;123:999-1005. |
| 6. | Ell C, Remke S, May A, Helou L, Henrich R, Mayer G. The first prospective controlled trial comparing wireless capsule endoscopy with push enteroscopy in chronic gastrointestinal bleeding. Endoscopy. 2002;34:685-689. |
| 7. | Eliakim R, Fischer D, Suissa A, Yassin K, Katz D, Guttman N, Migdal M. Wireless capsule video endoscopy is a superior diagnostic tool in comparison to barium follow-through and computerized tomography in patients with suspected Crohn's disease. Eur J Gastroenterol Hepatol. 2003;15:363-367. |
| 8. | Carretero C, Fernandez-Urien I, Betes M, Muñoz-Navas M. Role of videocapsule endoscopy for gastrointestinal bleeding. World J Gastroenterol. 2008;14:5261-5264. |
| 9. | Schäfer C, Göke B. Do we underestimate capsule endoscopy in the upper gastrointestinal tract? Digestion. 2005;72:239-241. |
| 10. | Peter S, Heuss LT, Beglinger C, Degen L. Capsule endoscopy of the upper gastrointestinal tract -- the need for a second endoscopy. Digestion. 2005;72:242-247. |
| 11. | Tang SJ, Zanati S, Kandel G, Marcon NE, Kortan P. Gastric intestinal vascular ectasia syndrome: findings on capsule endoscopy. Endoscopy. 2005;37:1244-1247. |
| 12. | Kitiyakara T, Selby W. Non-small-bowel lesions detected by capsule endoscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2005;62:234-238. |
| 13. | Sidhu R, Sanders DS, McAlindon ME. Does capsule endoscopy recognise gastric antral vascular ectasia more frequently than conventional endoscopy? J Gastrointestin Liver Dis. 2006;15:375-377. |
| 14. | Eliakim R, Yassin K, Shlomi I, Suissa A, Eisen GM. A novel diagnostic tool for detecting oesophageal pathology: the PillCam oesophageal video capsule. Aliment Pharmacol Ther. 2004;20:1083-1089. |
| 15. | Koslowsky B, Jacob H, Eliakim R, Adler SN. PillCam ESO in esophageal studies: improved diagnostic yield of 14 frames per second (fps) compared with 4 fps. Endoscopy. 2006;38:27-30. |
| 16. | Sharma P, Wani S, Rastogi A, Bansal A, Higbee A, Mathur S, Esquivel R, Camargo L, Sampliner RE. The diagnostic accuracy of esophageal capsule endoscopy in patients with gastroesophageal reflux disease and Barrett's esophagus: a blinded, prospective study. Am J Gastroenterol. 2008;103:525-532. |
| 17. | Fernandez-Urien I, Carretero C, Armendariz R, Muñoz-Navas M. Esophageal capsule endoscopy. World J Gastroenterol. 2008;14:5254-5260. |
| 18. | de Franchis R, Eisen GM, Laine L, Fernandez-Urien I, Herrerias JM, Brown RD, Fisher L, Vargas HE, Vargo J, Thompson J. Esophageal capsule endoscopy for screening and surveillance of esophageal varices in patients with portal hypertension. Hepatology. 2008;47:1595-1603. |
| 19. | Neu B, Wettschureck E, Rösch T. Is esophageal capsule endoscopy feasible? Results of a pilot. Endoscopy. 2003;35:957-961. |
| 20. | Rondonotti E, Herrerias JM, Pennazio M, Caunedo A, Mascarenhas-Saraiva M, de Franchis R. Complications, limitations, and failures of capsule endoscopy: a review of 733 cases. Gastrointest Endosc. 2005;62:712-716; quiz 752, 754. |
| 21. | Liao Z, Li F, Li ZS. Right lateral position improves complete examination rate of capsule endoscope: a prospective randomized, controlled trial. Endoscopy. 2008;40:483-487. |