Published online Dec 7, 2009. doi: 10.3748/wjg.15.5712
Revised: September 1, 2009
Accepted: September 8, 2009
Published online: December 7, 2009
AIM: To investigate the effects of a novel Leukotriene B4 receptor antagonist and/or tacrolimus on ischemia-reperfusion in a rat liver model.
METHODS: Male Lewis rats were pretreated with ONO-4057 (100 mg/kg) and/or tacrolimus (1 mg/kg) orally, and divided into four experimental groups; group 1 (control), group 2 (ONO-4057), group 3 (tacrolimus), group 4 (ONO-4057 + tacrolimus).
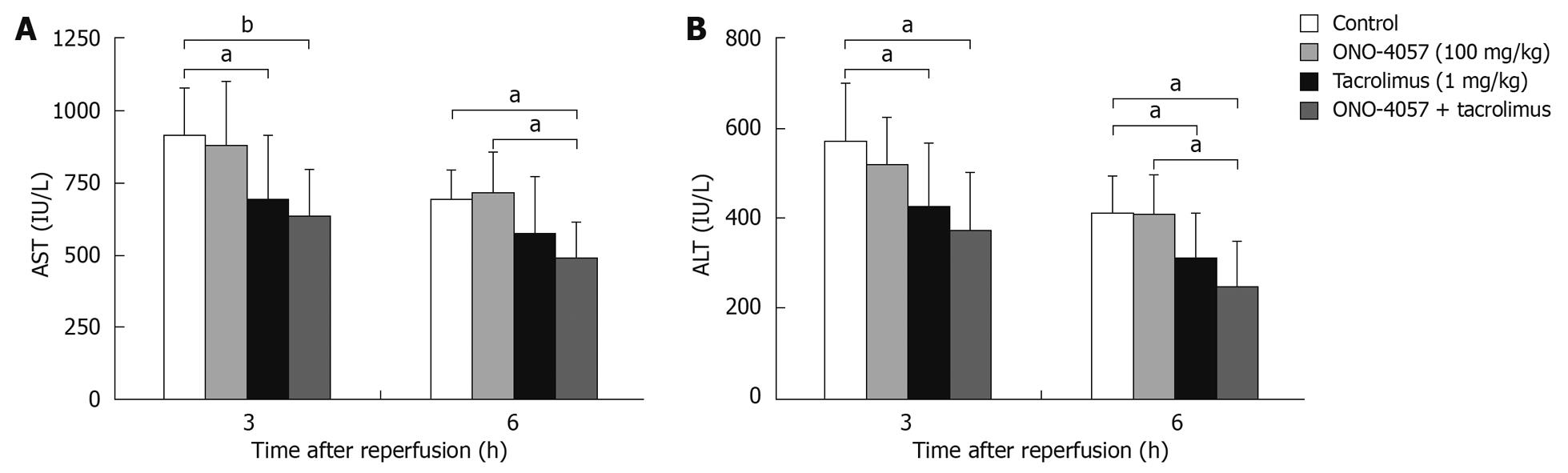
RESULTS: There was a tendency for long survival in the groups treated with tacrolimus alone and ONO-4057 plus tacrolimus. Post-reperfusion serum aspartate aminotransferase levels decreased more significantly in ONO-4057 plus tacrolimus group (P < 0.01), than in the tacrolimus alone group (P < 0.05), compared to controls.
CONCLUSION: This study demonstrated that pretreatment with ONO-4057 in combination with tacrolimus produced additive effects in a rat model of liver ischemia-reperfusion injury.
- Citation: Takeichi T, Uemoto S, Minamiguchi S, Takeyoshi I, Inomata Y, Tanaka K, Kobayashi E. Effect of ONO-4057 and tacrolimus on ischemia-reperfusion injury of the liver. World J Gastroenterol 2009; 15(45): 5712-5715
- URL: https://www.wjgnet.com/1007-9327/full/v15/i45/5712.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.5712
Neutrophils are mainly responsible for the physiopathological changes that occur after ischemia-reperfusion injury[1-3]. These cells are markedly activated when the ischemically damaged liver is transplanted. Experimental efforts have focused on understanding the etiology of ischemic injury and protecting the liver by pharmacological intervention[4-7].
Pretreatment with certain immunosuppressive drugs has been shown to protect against neutrophil-mediated reperfusion injury[4,5]. Calcineurin inhibiters are thought to suppress both proinflammatory cytokine production and expression of adhesive molecules of neutrophils[8]. Recently, ONO-4057 (5-[2-(2-carboxyethyl)-3-{6-(4-methoxyphenyl)-5E-hexenyl}yphenoxy]valeric acid), an orally administered active leukotriene B4 (LTB4) receptor antagonist, was developed and was shown to have an important effect on LTB4-induced neutrophil function[6,7].
In this study, we investigated the effect of pretreatment with ONO-4057 alone and in combination with tacrolimus on ischemia-reperfusion injury of the liver in rats.
Male Lewis rats (Charles River, Hamamatsu, Japan), 5-6 wk of age, were used in this study. The animals were housed in a pathogen-free, temperature- and light-controlled environment with free access to food and water. The rats were anesthetized with ether for induction and maintenance. All experimental protocols were approved by the institutional review board of Kyoto University.
The animals were divided into four experimental groups: group 1, controls; group 2, ONO-4057; group 3, tacrolimus; and group 4, ONO-4057 and tacrolimus (n = 9 in each group). The control groups received distilled water (DW) and NaHCO3 as a vehicle administered orally, and the other groups were pretreated with ONO-4057 (Ono Pharmaceutical Co., Ltd., Osaka, Japan) and tacrolimus (Fujisawa Pharmaceutical Co., Osaka). ONO-4057 was dissolved to a concentration of 30 mg/mL with NaHCO3, and tacrolimus was dissolved to a concentration of 0.3 mg/mL with DW. ONO-4057 was administered orally at a dose of 100 mg/kg and tacrolimus orally at a dose of 1 mg/kg. All agents were administered 1 h before ischemia was induced.
Whole-liver ischemia model: Normothermic ischemia of the entire liver (with intestinal congestion) was induced as described previously[8]. Briefly, a midline incision was made after the animals were anesthetized with ether and the portal vein, hepatic artery, and bile duct were clamped for 40, 50 and 60 min with a vascular micro-clip. The clip was then released and the abdominal wall was closed using a continuous running suture. The animals were returned to their cages for survival analysis for the following 2 wk.
Partial-liver ischemia model: To obtain data about more severe normothermic ischemia damage of the liver without intestinal congestion, the left and middle portal vein and hepatic artery were occluded for 60 min according to the procedure of Kawano et al[9] with a minor modification. This procedure induced 70% warm-ischemic liver damage, but 30% healthy liver remained to protect the animal’s life. After reperfusion, the abdominal wall was closed, and the treated rats were observed. One mL of the peripheral blood were obtained at 3 and 6 h after de-clamping, then the liver was perfused with 10 mL cold saline and immediately taken out. The damaged part of the liver was used for histological assessment and measurement of liver-tissue myeloperoxidase (MPO).
Using the peripheral blood obtained from the experimental animals, serum transaminase concentrations [aspartate aminotransferase (AST); alanine aminotransferase (ALT)] were measured by an ultraviolet method using an automatic analyzer (Hitachi 7170, Tokyo, Japan).
Hepatic samples were fixed in 10% buffered formaldehyde, embedded in paraffin, cut to 3 to 5 μm thick, and stained with hematoxylin and eosin. The specimens were blindly analyzed to evaluate the histological damage according to the modified classification of Suzuki et al[4].
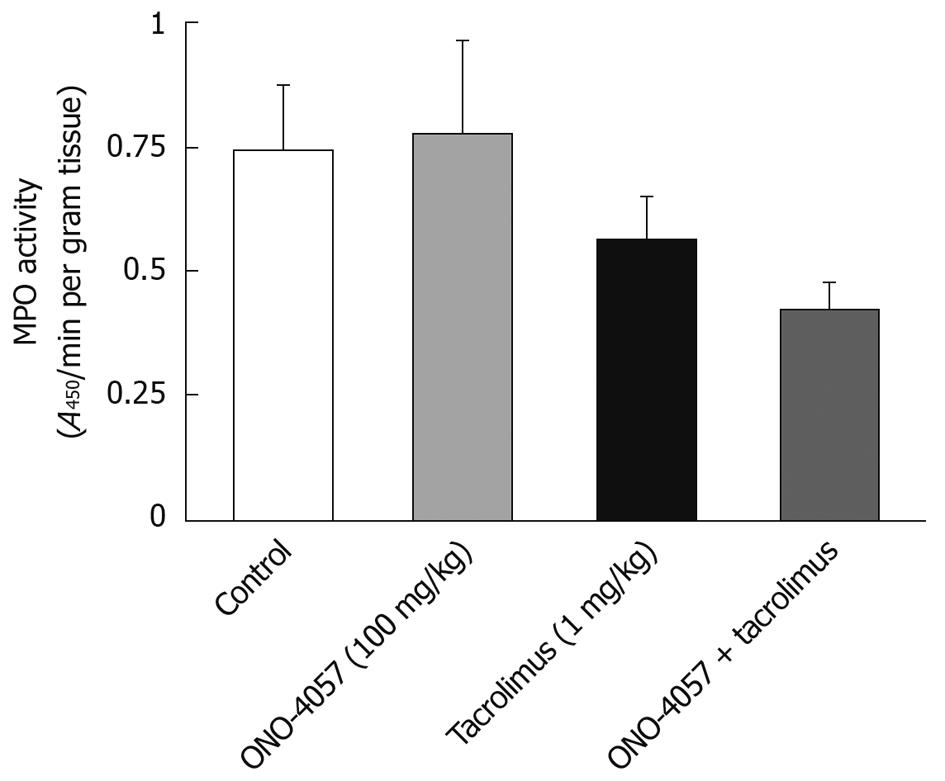
Liver-tissue MPO activity: MPO tissue level is considered to be an index of neutrophil infiltration in the liver. Liver samples obtained at 6 h after reperfusion were frozen in liquid nitrogen and stored at -70°C until the time of measurement. Tissue samples were then homogenized in 10 mL phosphate-buffered saline and centrifuged at 100 000 g and 4°C for 30 min. The resultant supernatant was assayed for MPO activity using the modified method of Shindler et al[10]. Briefly, the reaction mixture, containing 10:l of supernatant and 200:l of 100 mol/L ABTS buffer with H2O2, was incubated in 96-well plate for 60 min at 25°C. The optical density at 414 nm was determined by a plate reader (SPECTRA max™ 340; Molecular Devices Co., CA, USA). The MPO activity was calculated using an extinction coefficient of (3.6 × 104)/(mol per cm) for ABTS and normalized to protein levels (μmol/mg protein). The protein concentration was determined by the method of Lowry et al[11].
The repeated measurement analysis of variance (ANOVA) was performed among the groups. If repeated measurement ANOVA revealed a significant interaction, the statistical significance among the four groups at each time point was determined using post hoc tests. A P value of less than 0.05 was considered statistically significant.
Survival after pretreatment with ONO-4057 and/or tacrolimus on whole-liver ischemia in rats is shown in Table 1. Because 40 to 50 min of whole liver ischemia in adult Lewis rats (about weighting 280-330 g) was sublethal, we initially evaluated the 40 to 50 min ischemic damage in young Lewis rats in this study. However, all rats that had undergone 40 or 50 min of whole-liver ischemia survived indefinitely. When the results of 60 min of ischemia were evaluated, there was no significant difference in survival rate among the groups. However, the survival rate was slightly higher in the groups treated with tacrolimus alone (P = 0.053) and ONO-4057 plus tacrolimus. Serum AST values at 3 and 6 h after partial-liver ischemia-reperfusion are shown in Figure 1A. In the group pretreated with tacrolimus alone, the serum AST value was significantly lower than the control group at 3 and 6 h after reperfusion (P < 0.05), respectively. In the group pretreated with ONO-4057 plus tacrolimus, the AST level was more significantly lower compared with the control group (P < 0.01). Pretreatment with ONO-4057 and tacrolimus produced additive effects, but not when compared with the group treated with tacrolimus alone. ONO-4057 alone could not decrease the transaminase levels. Serum ALT values demonstrated a similar pattern (Figure 1B).
| Duration of ischemia (min) | Survival rates (%) | |||
| Controls | ONO-4057 | Tacrolimus | ONO-4057 + tacrolimus | |
| 40 | 6/6 (100) | 6/6 (100) | NT | NT |
| 50 | 6/6 (100) | 6/6 (100) | NT | NT |
| 60 | 2/9 (22) | 4/9 (44) | 6/9 (66) | 5/9 (56) |
The liver MPO levels after 6 h of reperfusion are shown in Figure 2. There was no significant difference among the groups in MPO activity. However, the MPO level in the group treated with ONO-4057 plus tacrolimus tended to be lower compared with that in the control group, although it was not statistically significant (P = 0.059). At 6 h from the reperfusion after 60 min of partial liver ischemia, the liver damage (congestion, vacuolization, and necrosis) that was observed histologically was not significantly different among the groups.
In liver transplantation, ischemia-reperfusion injury is one of the major factors that might influence early graft function and late changes. The importance of neutrophils in the development of ischemia-reperfusion injury in the liver has been demonstrated[12,13].
LTB4, a metabolite formed via the 5-lipoxygenase pathway from arachidonic acid, is one of the most potent chemotactic and proinflammatory mediators. LTB4 causes neutrophil adhesion to vascular endothelial cells and infiltration into vascular endothelial cells. We investigated the effect of the LTB4 receptor antagonist, ONO-4057, on hepatic ischemia-reperfusion injury to determine whether they affect neutrophil infiltration into the liver and attenuate neutrophil-induced post-ischemic injury. Recent reports have also shown that some immunosuppressive drugs protect or attenuate the neutrophil-mediated ischemia-reperfusion injury in various organs (liver, small intestine, kidney, and heart)[5,14,15]. As tacrolimus has variable effects[16], we tested the effect of a combination of ONO-4057 with tacrolimus. The results showed that ischemia-reperfusion injury in the liver was not reduced by pretreatment with ONO-4057 alone. Tacrolimus was necessary for protection from I/R injury. Pretreatment with ONO-4057 had additive effects on the protective function of tacrolimus. Although the I/R damage was significantly prevented with the use of Tac and ONO-4057, the main damage might be related directly to the role of immunosuppressants. The suppression of the elevation of transaminases after I/R in this experiment might be mainly caused by the effect of tacrolimus. The MPO level in the liver specimens and the blood level of the transaminases did not correlate well in this study. MPO levels might be affected sub-significantly by the ONO-4057-mediated modification of neutrophils infiltration, but it did not directly prevent the hepatic damage.
Hepatic ischemia-reperfusion injury is caused by many factors, and this study has limited because it only focused on neutrophils’ infiltration. Two main causes have been reported for I/R injury; oxygen free radicals and neutrophil-mediated damage. Recent reports showed a beneficial effect of neutrophil-mediated inhibitors, such as neutrophil elastase inhibitor and tissue factor pathway inhibitor, on hepatic reperfusion injury[17,18]. In another study, treatment with leukotriene biosynthesis inhibitor (L664,536) had no effect on hepatic injury, although LTB4 formation was inhibited[19]. We showed the added effect of a LTB4 receptor antagonist and immunosuppressive drug. As ONO-4057 has been also reported to have an immunosuppressive effect in allogenic rat liver grafts[20], co-administration of ONO-4057 and tacrolimus might be reasonable for liver transplantation. Before any clinical trials, experiments using the transplantation model might be necessary.
In conclusion, our data showed that pretreatment with ONO-4057 in combination with tacrolimus produced additive effects in liver reperfusion-injury of rat, although treatment with ONO-4057 alone had no effect.
Ischemia-reperfusion injury is a major factor that might influence early graft function in liver transplantation. In this study, we investigated the effect of oral administration, a novel Leukotriene B4 (LTB4) receptor antagonist, and/or Tacrolimus on ischemia-reperfusion of rat liver model.
In ischemia-reperfusion injury of the liver, an excessive inflammatory response is considered as a key mechanism. The role of neutrophils in ischemia-reperfusion injury has recently been the focus of several investigations. In this study, we focused the importance of neutrophils.
We tested the combined effect of a LTB4 receptor antagonist with Tacrolimus for ischemia-reperfusion injury of the liver.
The findings in this study support the hypothesis that co-administration of ONO-4057 and tacrolimus might be reasonable for liver transplantation in the future.
This manuscript is sufficiently written and provides information concerning therapeutic options in I/R injury of the liver.
Peer reviewer: Valentin Fuhrmann, MD, Department of Internal Medicine 4, Intensive Care Unit, Medical University Vienna, Waehringer Guertel 18-20, A-1090 Vienna, Austria
S- Editor Tian L L- Editor Stewart GJ E- Editor Zheng XM
| 1. | Schmeling DJ, Caty MG, Oldham KT, Guice KS, Hinshaw DB. Evidence for neutrophil-related acute lung injury after intestinal ischemia-reperfusion. Surgery. 1989;106:195-201; discussion 201-202. |
| 2. | Kurtel H, Fujimoto K, Zimmerman BJ, Granger DN, Tso P. Ischemia-reperfusion-induced mucosal dysfunction: role of neutrophils. Am J Physiol. 1991;261:G490-G496. |
| 3. | Garcia-Criado FJ, Palma-Vargas JM, Valdunciel-Garcia JJ, Gomez-Alonso A, Srivastava O, Ezrin A, Anderson MB, Toledo-Pereyra LH. Sulfo-Lewis(x) diminishes neutrophil infiltration and free radicals with minimal effect on serum cytokines after liver ischemia and reperfusion. J Surg Res. 1997;70:187-194. |
| 4. | Suzuki S, Toledo-Pereyra LH, Rodriguez FJ, Cejalvo D. Neutrophil infiltration as an important factor in liver ischemia and reperfusion injury. Modulating effects of FK506 and cyclosporine. Transplantation. 1993;55:1265-1272. |
| 5. | Mizuta K, Ohmori M, Miyashita F, Kitoh Y, Fujimura A, Mori M, Kanno T, Hashizume K, Kobayashi E. Effect of pretreatment with FTY720 and cyclosporin on ischaemia-reperfusion injury of the liver in rats. J Pharm Pharmacol. 1999;51:1423-1428. |
| 6. | Kishikawa K, Matsunaga N, Maruyama T, Seo R, Toda M, Miyamoto T, Kawasaki A. ONO-LB-457: a novel and orally active leukotriene B4 receptor antagonist. Adv Prostaglandin Thromboxane Leukot Res. 1991;21A:407-410. |
| 7. | Kishikawa K, Tateishi N, Maruyama T, Seo R, Toda M, Miyamoto T. ONO-4057, a novel, orally active leukotriene B4 antagonist: effects on LTB4-induced neutrophil functions. Prostaglandins. 1992;44:261-275. |
| 8. | Ohmori M, Kobayashi E, Harada K, Kitoh Y, Mizuta K, Uchida H, Ogino Y, Fujimura A. Do immunosuppressants directly affect neutrophils, resulting in protection of the liver against ischemia-reperfusion injury? Transplantation. 1998;66:940-941. |
| 9. | Kawano K, Kim YI, Kaketani K, Kobayashi M. The beneficial effect of cyclosporine on liver ischemia in rats. Transplantation. 1989;48:759-764. |
| 10. | Shindler JS, Childs RE, Bardsley WG. Peroxidase from human cervical mucus. The isolation and characterisation. Eur J Biochem. 1976;65:325-331. |
| 11. | Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951;193:265-275. |
| 12. | Jaeschke H, Farhood A, Smith CW. Neutrophils contribute to ischemia/reperfusion injury in rat liver in vivo. FASEB J. 1990;4:3355-3359. |
| 13. | Poggetti RS, Moore FA, Moore EE, Bensard DD, Anderson BO, Banerjee A. Liver injury is a reversible neutrophil-mediated event following gut ischemia. Arch Surg. 1992;127:175-179. |
| 14. | Nishinaka Y, Sugiyama S, Yokota M, Saito H, Ozawa T. Protective effect of FK506 on ischemia/reperfusion-induced myocardial damage in canine heart. J Cardiovasc Pharmacol. 1993;21:448-454. |
| 15. | Sakr M, Zetti G, McClain C, Gavaler J, Nalesnik M, Todo S, Starzl T, Van Thiel D. The protective effect of FK506 pretreatment against renal ischemia/reperfusion injury in rats. Transplantation. 1992;53:987-991. |
| 16. | Garcia-Criado FJ, Palma-Vargas JM, Valdunciel-Garcia JJ, Toledo AH, Misawa K, Gomez-Alonso A, Toledo-Pereyra LH. Tacrolimus (FK506) down-regulates free radical tissue levels, serum cytokines, and neutrophil infiltration after severe liver ischemia. Transplantation. 1997;64:594-598. |
| 17. | Soejima Y, Yanaga K, Nishizaki T, Yoshizumi T, Uchiyama H, Sugimachi K. Effect of specific neutrophil elastase inhibitor on ischemia/reperfusion injury in rat liver transplantation. J Surg Res. 1999;86:150-154. |
| 18. | Yoshimura N, Kobayashi Y, Nakamura K, Yamagishi H, Oka T. The effect of tissue factor pathway inhibitor on hepatic ischemic reperfusion injury of the rat. Transplantation. 1999;67:45-53. |
| 19. | Hughes H, Farhood A, Jaeschke H. Role of leukotriene B4 in the pathogenesis of hepatic ischemia-reperfusion injury in the rat. Prostaglandins Leukot Essent Fatty Acids. 1992;45:113-119. |
| 20. | Ii T, Izumi R, Shimizu K. The immunosuppressive effects of a leukotriene B4 receptor antagonist on liver allotransplantation in rats. Surg Today. 1996;26:419-426. |