Published online Aug 28, 2009. doi: 10.3748/wjg.15.4083
Revised: July 29, 2009
Accepted: August 5, 2009
Published online: August 28, 2009
Most complications after appendectomy occur within ten days; however, we report the unusual case of a suture granuloma 12 years after open appendectomy. The afebrile 75-year-old woman presented with a slightly painful palpable mass in the right lower abdomen. There was no nausea or vomiting and bowel movements were normal. She lost 10 kg during the 3 mo before presentation. The patient had undergone an appendectomy 12 years previously. Physical examination revealed a tender mass, 10 cm in diameter, under the appendectomy scar. The preoperative laboratory findings, tumor markers and plain abdominal radiographs were normal. Multi-slice computed tomography scanning showed an inhomogenous abdominal mass with minimal vascularization in the right lower abdomen 8.6 cm × 8 cm × 9 cm in size which communicated with the abdominal wall. The abdominal wall was thickened, weak and bulging. The abdominal wall mass did not communicate with the cecum or the ascending colon. Complete excision of the abdominal wall mass was performed via median laparotomy. Histopathological examination revealed a granuloma with a central abscess. This case report demonstrates that a preoperative diagnosis of abdominal wall mass after open appendectomy warrants the use of a wide spectrum of diagnostic modalities and consequently different treatment options.
- Citation: Augustin G, Korolija D, Skegro M, Jakic-Razumovic J. Suture granuloma of the abdominal wall with intra-abdominal extension 12 years after open appendectomy. World J Gastroenterol 2009; 15(32): 4083-4086
- URL: https://www.wjgnet.com/1007-9327/full/v15/i32/4083.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.4083
Appendicitis was recognized as a surgical disease when Reginald Heber Fitz correctly pointed out that the frequent abscesses in the right iliac fossa were often due to perforation of the vermiform appendix, and he referred to the condition as appendicitis[1]. Since that discovery and the development of various surgical incisions and appendectomy techniques, many early and late postoperative complications and coincident conditions have become evident. One of these complications is a postoperative abdominal wall mass in the region of McBurney’s muscle-splitting incision. The diagnosis and management of abdominal wall masses after open appendectomy are challenging because various conditions such as appendectomy-related, primary-local (appendectomy-unrelated) and primary-systemic could be the cause of abdominal wall masses postoperatively. This report presents the first known case of a suture granuloma with intra-abdominal extension as a cause of an abdominal wall mass after open (muscle-splitting) appendectomy.
A 75 year-old woman presented with a slightly painful palpable mass in the right lower abdomen lasting for 6 mo. The pain in the right lower quadrant was described as continuous, nonradiating, mild and non-disturbing. There was no nausea or vomiting. Body temperature was 36.8°C and bowel movements were normal. She lost 10 kg during the 3 mo before presentation. The patient had undergone open appendectomy (muscle-splitting incision) 12 years previously. Five years ago she had undergone vaginal hysterectomy with bilateral salpingo-oophorectomy for uterine leiomyomata. Following surgery the patient was in good health and without any symptoms or complaints. She did not take any medications. Physical examination revealed a slightly tender mass, 10 cm in diameter, under the appendectomy scar in the right lower abdomen. The swelling was elastic and poor in mobility. Other resistances were not found, and the rest of the physical examination was normal.
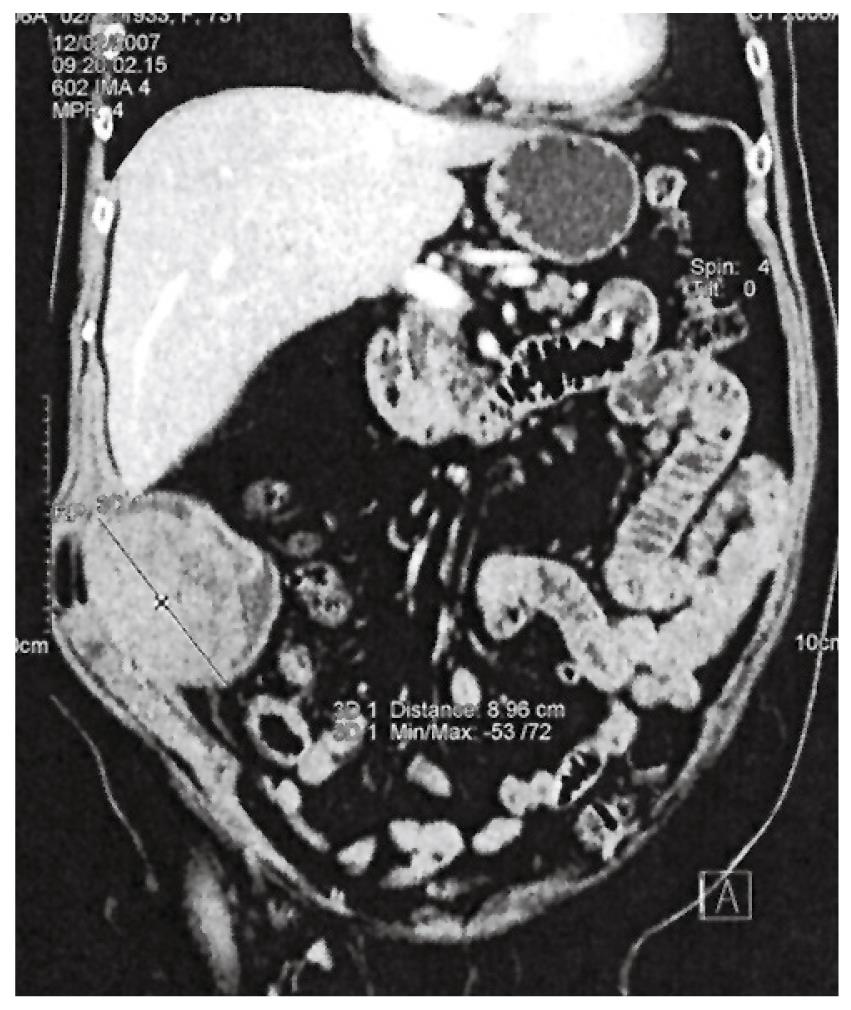
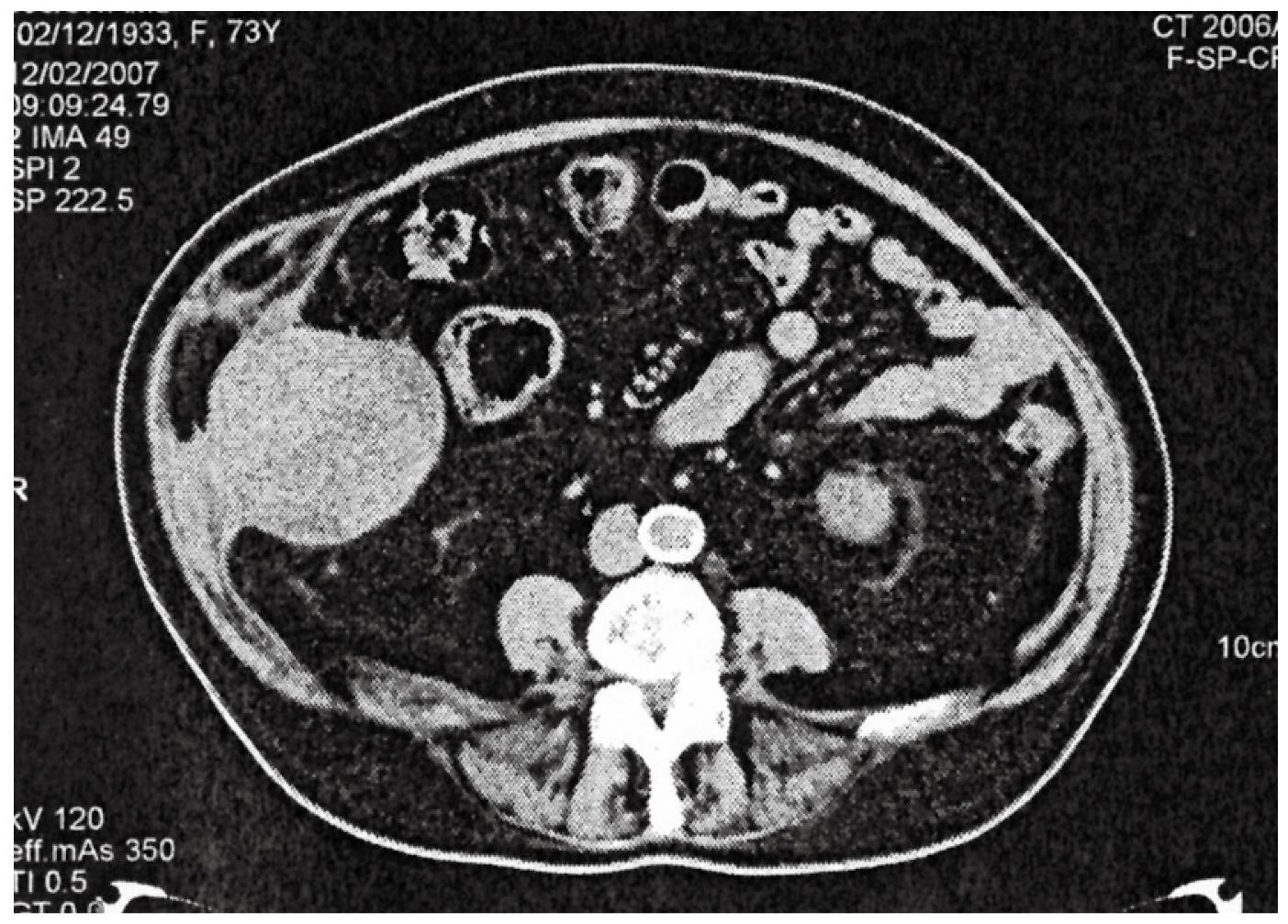
Preoperative laboratory findings and plain abdominal radiographs were normal. Tumor markers were as follows: CEA = 2.42 μg/L; AFP 1.24 μg/L; CA19.9 = 4.89 kU/L and CA 125 = 5.80 kU/L. Abdominal ultrasonography demonstrated a low-echoic mass lesion 8 cm × 8 cm just lateral to the cecum and in communication with the lateral abdominal wall. No peristalsis or communication with the bowel lumen was observed. Esophagogastroscopy revealed chronic gastritis and colonoscopy revealed sigmoid diverticulosis and normal mucosa in the cecum with normal ileocecal valve. Multi-slice CT scanning showed an inhomogenous abdominal mass with minimal vascularization in the right lower abdomen which was 8.6 cm × 8 cm × 9 cm in size and communicated with the abdominal wall. The abdominal wall was thickened, weak and bulging (Figure 1). There was no communication between the cecum and the abdominal wall which was also confirmed by previous colonoscopy (Figure 2). From these findings an abdominal wall tumor was suspected and elective surgery was performed.
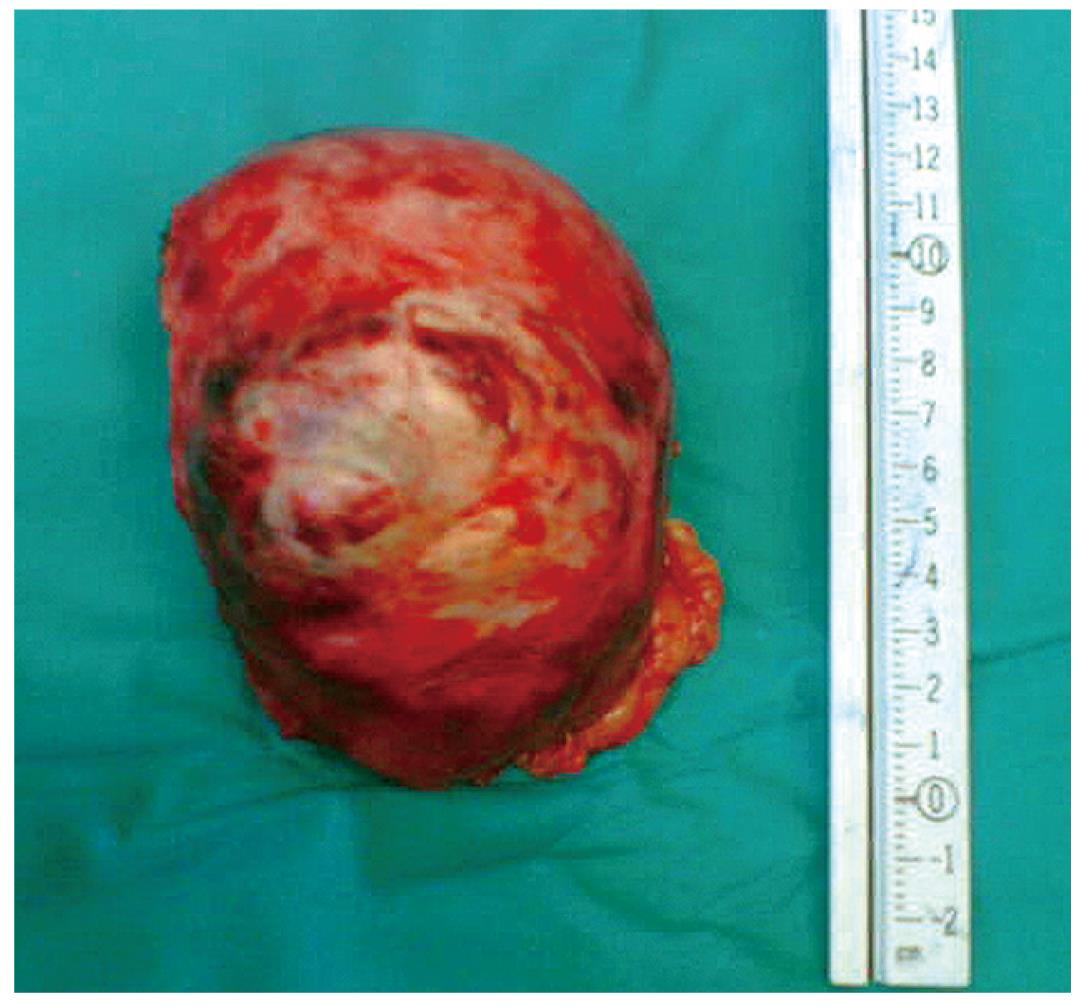
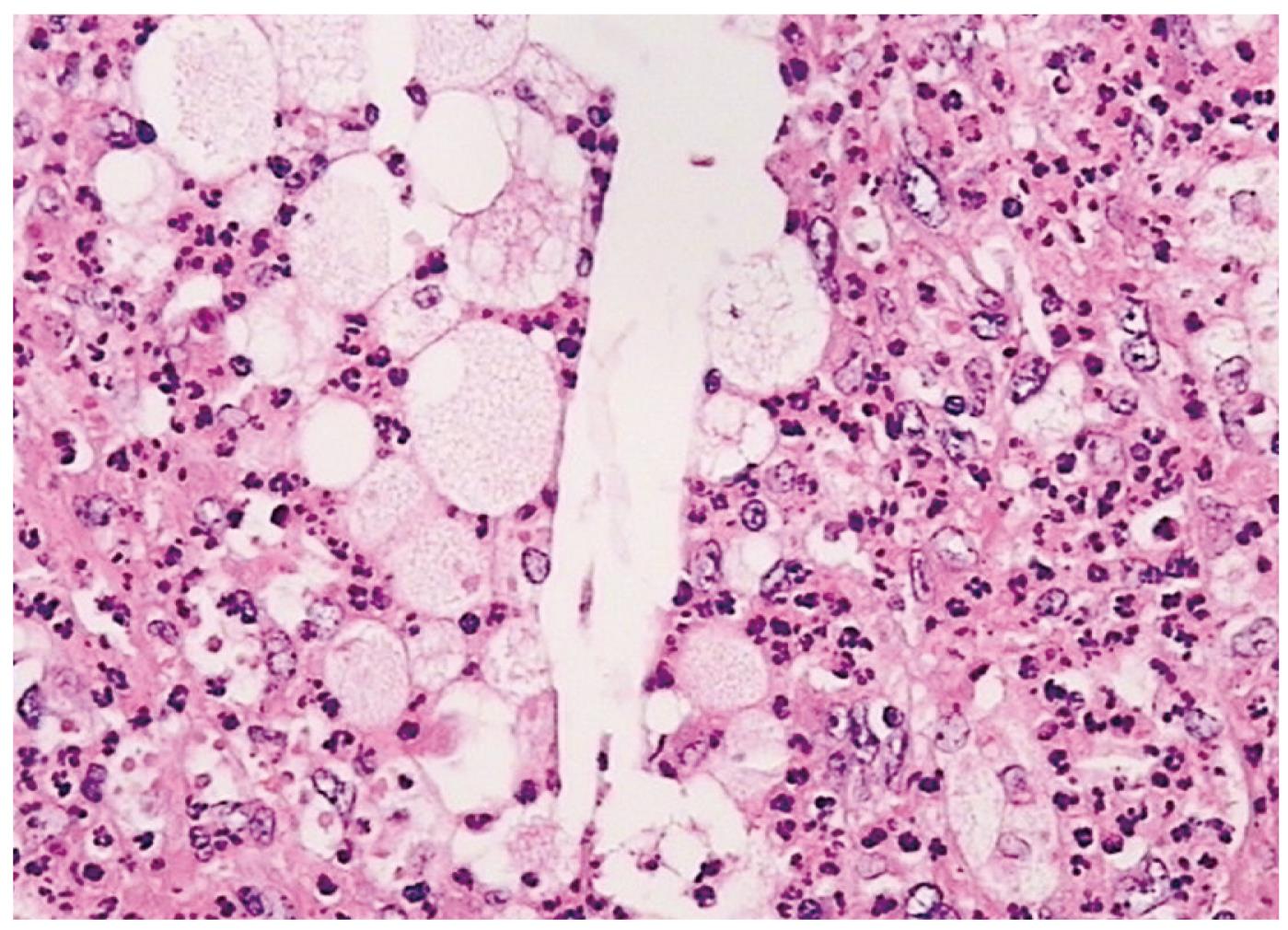
After a midline laparotomy and adhesiolysis, the greater omentum was detached from the mass in the right lower abdomen which was located intraperitoneally. There was no free intraperitoneal fluid or fibrin deposits. The elastic mass was adherent to the abdominal wall and there was no communication with the small and large bowel, retroperitoneal or vascular structures. After partial omentectomy, the mass was completely extirpated from the abdominal wall (Figure 3). Histopathological examination revealed a foreign-body granuloma with a central abscess (Figure 4). The patient’s early postoperative course was uneventful and she left hospital on the 10th postoperative day. On several control examinations during the first 18 mo, the patient was completely symptomless.
This case represents an unusual complication of a suture granuloma with intra-abdominal extension as a cause of an abdominal wall mass 12 years after open appendectomy. To our knowledge (Medline search 1962-2007) this is the third case of such a complication after appendectomy. Abdominal wall abscesses after appendectomy were diagnosed by Matsuda et al[2] 11 years postoperatively and by Ichimiya et al[3] 25 years postoperatively.
A unique feature in our case was the intra-abdominal extension of the abdominal wall suture granuloma with a central abscess which complicated definitive diagnosis.
Since the development of various surgical incisions and appendectomy techniques, many early and late postoperative complications and coincident conditions have become evident. One of these complications is a postoperative abdominal wall mass in the region of McBurney’s muscle-splitting incision. Morbidity associated with appendectomy can be as high as 25% in complicated cases[4]. Morbiditiy can be divided into early and late complications. Early complications are more common and mostly include wound hematoma, seroma, abscess or intra-abdominal abscess due to persistence of cavities between the muscle layers and the subcutaneous tissue which encourages fluid collections[5]. These complications can then result in cystic formations or masses that can simulate a tumor of the abdominal wall, if they are not readily resolved. For this reason, a meticulous surgical technique, careful hemostasis and placement of suction drains in the subcutaneous tissue are recommended, principally in obese patients[6]. Late complications are rare and can include obstruction due to adhesions, postoperative hernia or progression of inflammatory bowel disease not evident at operation for suspected appendicitis. Most of these complications can present as an abdominal mass. An abdominal mass as a primary pathology or postoperative finding always makes precise preoperative diagnosis difficult. A complete list of differential diagnoses of late presenting abdominal wall masses after open appendectomy is shown in Table 1.
| Suture granuloma |
| Rectus hematoma |
| Spontaneous |
| Traumatic |
| Postoperative |
| Wound hematoma (organized) |
| Abscess |
| Abdominal wall (various etiologies) |
| Intra-abdominal (extension) |
| Hernia |
| Incisional |
| Spigelian |
| Groin |
| Keloid |
| Traumatic neuroma |
| Heterotopic bone formation |
| Incisional |
| Traumatic |
| Abdominal wall tumors |
| Benign (various) |
| Malignant (various) |
| Metastatic |
| Hematogenous |
| Post-instrumentation |
| Port site/trocar metastases |
| Incisional site metastases |
| Percutaneous |
| Intra-abdominal malignancy (extension) |
| Urachal remnant/cyst/inflammatory mass |
| Uterine/extrauterine (lipo) leiomyomas |
| Primary |
| Incisional |
| Endometriosis |
| Cutaneous (primary) |
| Surgical scar endometriosis |
| Mastocytosis |
| Systemic juvenile xanthogranulomatosis |
| Lymphoproliferative disorders (congenital/acquired) |
| Parasitic (abscess or granuloma) |
| Enterobius vermicularis |
| Hydatid cyst |
| Mycetoma (endemic) |
| Actinomycosis |
| Extension from intestinal actinomycosis |
| Abdominal wall (hematogenous) |
Several points should be stressed. Firstly, abdominal wall masses could be: (1) appendectomy-related; (2) primary; (3) posttraumatic; and (4) related to other interventions in the surrounding area for other pathologic conditions. Thus, history taking and physical examination are crucial. The time interval from appendectomy is essential because it determines the difference between early and late complications of appendectomy. Furthermore, symptoms and signs of unrelated diseases (local or systemic) should be confirmed or ruled out (abdominal wall tumors, extension of intra-abdominal malignancy, endometriosis, lymphoproliferative disorders etc). Confirmation of invasive interventions in the surrounding area is very important. Open/laparoscopic surgery for intra-abdominal malignancy/infectious diseases, percutaneous or laparoscopic biopsy or percutaneous fine-needle aspiration for malignant hepatobiliary disease could be the cause of abdominal wall port site or incisional metastases or abscesses.
Secondly, by delineating the peritoneal line, the intraperitoneal or extraperitoneal location of the lesion can be determined. This is important for several reasons. First, the entrance into the peritoneal cavity could be avoided during surgery if the lesion is located extraperitoneally. Also if the abscess is the cause (acute or chronic) then the extraperitoneal route avoids spillage of contents into the abdominal cavity thus eliminating the possibility of intra-abdominal abscess as a postoperative complication.
Generally, early postoperative masses are easier to diagnose and treat, while late postoperative abdominal wall masses could be of various etiologies that warrant the use of a wide spectrum of diagnostic modalities and consequently different treatment options. All these facts signify the importance of preoperative diagnosis. Thus, abdominal ultrasound, contrast-enhanced multi-slice CT and other diagnostic modalities should be used according to clinical findings. It is concluded that late postoperative abdominal wall masses after open appendectomy can be of various etiologies that warrant the use of a wide spectrum of diagnostic modalities and consequently different treatment options.
| 1. | Fitz RH. Perforating inflammation of the vermiform appendix: with special reference to its early diagnosis and treatment. Am J Med Sci. 1886;92:321–346. |
| 2. | Matsuda K, Masaki T, Toyoshima O, Ono M, Muto T. The occurrence of an abdominal wall abscess 11 years after appendectomy: report of a case. Surg Today. 1999;29:931-934. |
| 3. | Ichimiya M, Hamamoto Y, Muto M. A case of suture granuloma occurring 25 years after an appendectomy. J Dermatol. 2003;30:634-636. |
| 4. | Yagmurlu A, Vernon A, Barnhart DC, Georgeson KE, Harmon CM. Laparoscopic appendectomy for perforated appendicitis: a comparison with open appendectomy. Surg Endosc. 2006;20:1051-1054. |