Published online Nov 21, 2008. doi: 10.3748/wjg.14.6757
Revised: October 5, 2008
Accepted: October 12, 2008
Published online: November 21, 2008
A 46-year-old Chinese woman presented with nausea, recurrent vomiting, and abdominal pain. Gastroduodenal endoscopic examination revealed an oval-shaped submucosal tumor at the prepyloric area on the posterior wall of the stomach. A degenerated gastrointestinal stromal tumor was suspected. Distal gastrectomy was performed and a histological diagnosis of heterotopic pancreas (HPs) was confirmed. The patient had an uneventful postoperative course and was discharged 7 d after operation. The patient remains healthy and symptom-free in the follow-up of 6 mo. This is a report of a case of gastric outlet obstruction resulting from pancreatic heterotopia in the gastric antrum in an adult woman.
- Citation: Jiang LX, Xu J, Wang XW, Zhou FR, Gao W, Yu GH, Lv ZC, Zheng HT. Gastric outlet obstruction caused by heterotopic pancreas: A case report and a quick review. World J Gastroenterol 2008; 14(43): 6757-6759
- URL: https://www.wjgnet.com/1007-9327/full/v14/i43/6757.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6757
Heterotopic pancreas (HPs), a rare entity, is defined as the presence of pancreatic tissue outside its normal localization and without anatomic and vascular continuity with the pancreas itself. Other terms such as pancreatic rest, ectopic, aberrant, or accessory pancreas are also used [1]. It can occur anywhere in the gastrointestinal (GI) tract. The etiology of HP is unknown. In most cases, HP does not cause symptoms, but it can occasionally present as nausea, vomiting and abdominal pain. Peptic ulceration and upper GI bleeding are rare presentations, as are malignant degeneration, pancreatitis and pseudocysts[2]. HP tissue is found in persons of all ages and slightly more often in man[3]. HP has been reported as the cause of gastric outlet obstruction in infant[4] or child[5]. This is a report of a case of gastric outlet obstruction resulting from pancreatic heterotopias in the gastric antrum in an adult woman.
A 46-year-old woman was admitted to our hospital with a 5-year history of chronic epigastric pain and recurrent vomiting after meal. The patient had an unremarkable medical history. The physical examination was normal. She was afebrile with stable vital signs. The abdomen was soft and nontender with no palpable mass and normal bowel sounds. Stools tested negative for occult blood. Hematologic examination and blood chemical findings were normal as well.
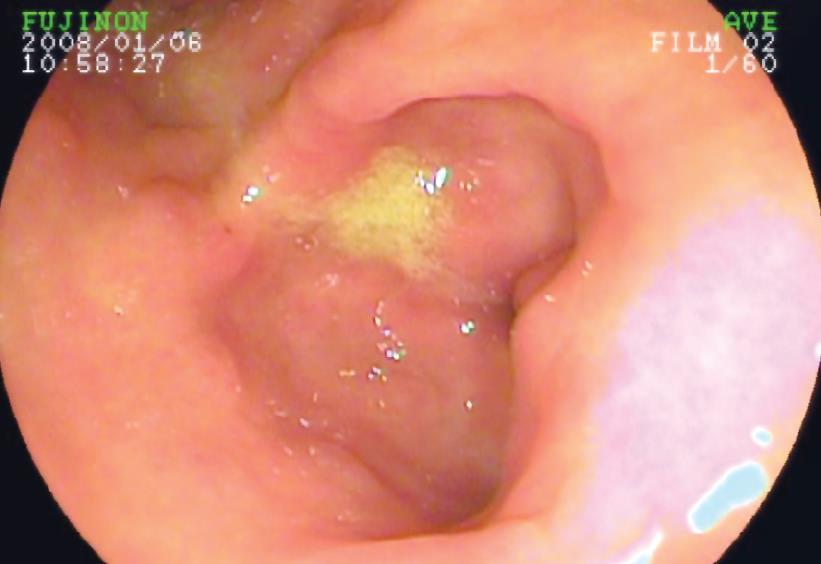
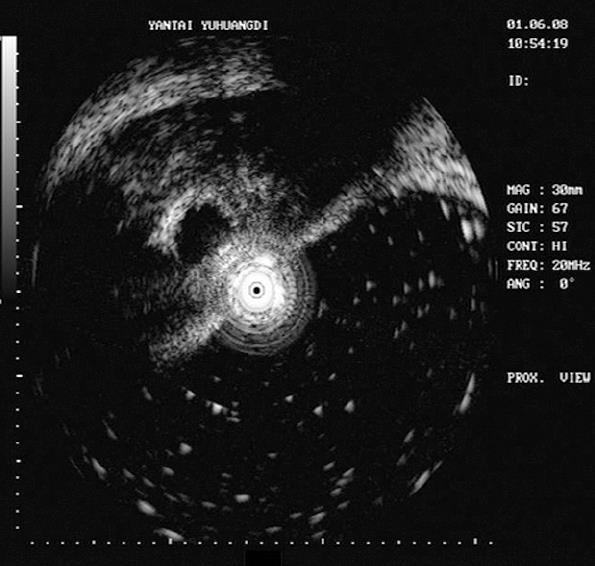
Gastroscopy showed antritis and a submucosal lesion in the prepyloric posterior gastric wall (Figure 1). Proton pump inhibitors were started but did not relieve the symptoms. A computer tomography scan showed thickness of posterior gastric wall, measuring 1 cm × 1.5 cm in the lower body of the stomach (Figure 2). Endoscopic ultrasonography revealed a lesion of 1.5 cm in diameter, with low and high complex echogenicity around this tissue, located within either the third or fourth echo-layers (Figure 3).
The results of biopsy were nondiagnostic, and disclosed only mild gastritis. Attempts of ploric dilation once proved unsuccessful, because the patient remained symptomatic: recurrent vomiting and epigastric pain despite helicobacter eradication and ploric dilation. A surgical exploration was proposed.
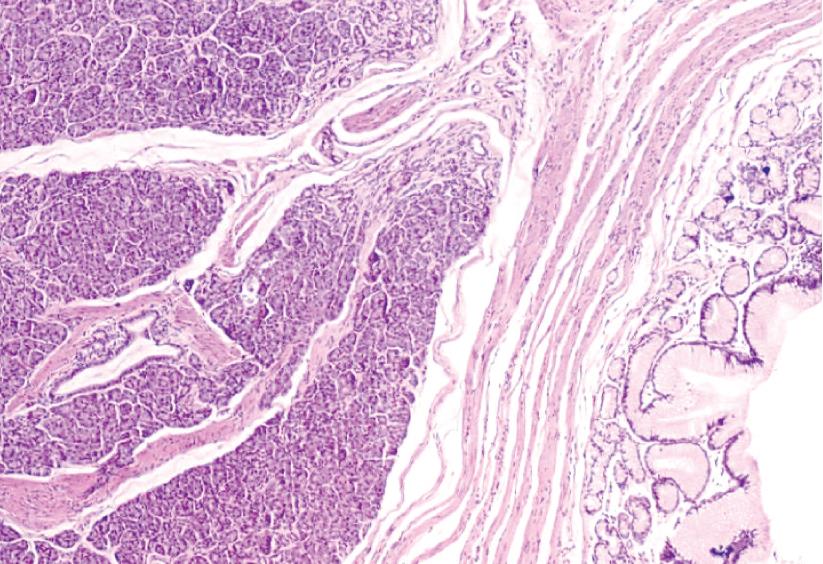
The lesion was removed with gastrectomy and gastrojejunostomy due to a presumed diagnosis of gastric outlet obstruction and submucosal tumor and because endoscopic biopsy was not diagnostic. The resected mass measured 1.5 cm × 2.0 cm × 1.0 cm with no ulceration or excessive induration. Some mucosal areas were remarkable for the presence of heterotopic pancreatic tissue with fully developed acini and ducts (Figure 4). The margins of the resection were negative, and the lymph nodes were benign.
The postoperative course was uneventful. After the operation, vomiting episodes ceased, the patient gained 3 kg of body weight, and returned to full physical activity. The patient remained healthy and symptom-free in the follow-up of 6 mo.
The first case report of HP was made by Schultz in 1729. It is possible that early in fetal life, during rotation of the foregut and fusion of the dorsal and ventral parts of the pancreas, small parts are separated from it, and continue to develop in the wrong location[3]. Most often, HP is found in the stomach, duodenum and jejunum, but it may also be found anywhere in the digestive tract, intra-abdominally, in the mediastinum, and in the lung[1].
HP tissue is often found incidentally in patients operated on for other reasons or during autopsies. The condition is relatively uncommon, it has been found in 1%-2% of patients in autopsy studies and encountered in about 1 of 500 operations in the upper abdomen[6]. Macroscopically, HP consists of lobular white or yellow nodular tumors about 1-4 cm in diameter[1]. The mean size of HP was 1.52 cm in diameter (range 0.2-4 cm)[7]. A central mucosal depression, also described as volcanic of crater-like, is often recognized at endoscopy. The endoscopic appearance of gastric depends on the localization, HP may present with various symptoms. Nausea (27%) and vomiting, epigastric pain (27%) and ulceration (27%) were the most frequent clinical signs[7]. Heartburn and dyspepsia are also frequent for gastric HP, but often there are symptoms due to mechanical obstruction[1]. In the series of 34 patients with pancreatic heterotopia of Armstrong et al, 8 lesions were located in the stomach and 6 of those had produced symptoms[8]. There was a significant correlation between the size of the lesion and the presence of symptoms. Armstrong et al found that symptoms are related to the size of HP lesion. They postulated that size greater than 1.5 cm is more likely to be of clinical significance[8]. Other less common symptoms were bleeding mimicking jejunal tumor[9], pancreatitis, and malignant transformation[10-12].
Macroscopically, the tissue often localized in the submucosa, but may also be found in the muscularis mucosa, subserously or in the serosa. In some cases, it streches through several or all of these layers[3]. Although imaging studies such as computer tomography (CT), radiographic contrast studies, and upper endoscopy are of assistance in the initial assessment of patients, the preoperative diagnosis of pancreatic heterotopia is often difficult.
Ormarsson et al reported that all patients examined with CT were inconclusive[1]. Cho et al also reported CT findings interpreted as HP in only two cases (17%)[13]. A diagnosis can occasionally be made on the basis of endoscopic biopsies. Histological examinations are inconclusive in about 50% of the cases because normal gastric mucosa covers the lesions[14]. Only in 4 out 10 patients did a biopsy lead to the correct diagnosis[1]. In most cases, however, the diagnosis is confirmed only by surgical resection.
Endoscopic ultrasonography (EUS) is widely used to evaluate submucosal lesions in the upper GI tract[15]. In a retrospective study of postresection histologic features compared with preoperative EUS findings in 10 patients with gastric HP, there was a close correlation between histology and EUS findings. EUS-guided aspiration has been reported to be helpful in diagnosis of HP[16]. If endoscopic resection is considered, EUS is also extremely useful for pre-excision assessment[17].
Most patients with HP are asymptomatic and require no treatment. The lesion is usually discovered incidentally. There was no correlation between the histological type of HP and the presence of symptoms[1,18]. Surgery is frequently needed to make a definitive diagnosis and to plan further treatment because the differential diagnosis of pancreatic rests includes leiomyoma, lymphoma, carcinoid tumors, and other malignancies[19].
If HP is discovered as an incidental finding, local excision is recommended. When HP results in symptoms, the lesion should be resected[20,21]. Increasingly, some are removed endoscopically with satisfactory postoperative results. Endoscopic excision can be considered in select cases depending on the size and location of the mass, especially for treating the benign lesions of HP.
Peer reviewer: Taku Aoki, MD, Division of Hepato-Biliary-Pancreatic and Transplantation Surgery, Department of Surgery, Graduate School of Medicine, University of Tokyo, 7-3-1 Hongo, Bunkyo-ku, Tokyo 113-8655, Japan
S- Editor Li DL L- Editor Ma JY E- Editor Ma WH
| 1. | Ormarsson OT, Gudmundsdottir I, Marvik R. Diagnosis and treatment of gastric heterotopic pancreas. World J Surg. 2006;30:1682-1689. |
| 2. | Chou SJ, Chou YW, Jan HC, Chen VT, Chen TH. Ectopic pancreas in the ampulla of vater with obstructive jaundice. A case report and review of literature. Dig Surg. 2006;23:262-264. |
| 3. | Pang LC. Pancreatic heterotopia: a reappraisal and clinicopathologic analysis of 32 cases. South Med J. 1988;81:1264-1275. |
| 4. | Ozcan C, Celik A, Guclu C, Balik E. A rare cause of gastric outlet obstruction in the newborn: Pyloric ectopic pancreas. J Pediatr Surg. 2002;37:119-120. |
| 5. | Ertem D, Tutar E, Cam S, Ugras M, Pehlivanoglu E. Severe gastric outlet obstruction in a child with ectopic pancreas: is there a role for Helicobacter pylori? J Pediatr Gastroenterol Nutr. 2006;43:385-387. |
| 6. | Matsushita M, Hajiro K, Okazaki K, Takakuwa H. Gastric aberrant pancreas: EUS analysis in comparison with the histology. Gastrointest Endosc. 1999;49:493-497. |
| 7. | Eisenberger CF, Gocht A, Knoefel WT, Busch CB, Peiper M, Kutup A, Yekebas EF, Hosch SB, Lambrecht W, Izbicki JR. Heterotopic pancreas--clinical presentation and pathology with review of the literature. Hepatogastroenterology. 2004;51:854-858. |
| 8. | Armstrong CP, King PM, Dixon JM, Macleod IB. The clinical significance of heterotopic pancreas in the gastrointestinal tract. Br J Surg. 1981;68:384-387. |
| 9. | Joo YE, Kim HS, Choi SK, Rew JS, Park CS, Kim YJ, Kim SJ. Massive gastrointestinal bleeding caused by ectopic pancreas mimicking jejunal tumor. Digestion. 2001;64:133-136. |
| 10. | Ura H, Denno R, Hirata K, Saeki A, Hirata K, Natori H. Carcinoma arising from ectopic pancreas in the stomach: endosonographic detection of malignant change. J Clin Ultrasound. 1998;26:265-268. |
| 11. | Jeong HY, Yang HW, Seo SW, Seong JK, Na BK, Lee BS, Song GS, Park HS, Lee HY. Adenocarcinoma arising from an ectopic pancreas in the stomach. Endoscopy. 2002;34:1014-1017. |
| 12. | Song DE, Kwon Y, Kim KR, Oh ST, Kim JS. Adenocarcinoma arising in gastric heterotopic pancreas: a case report. J Korean Med Sci. 2004;19:145-148. |
| 13. | Cho JS, Shin KS, Kwon ST, Kim JW, Song CJ, Noh SM, Kang DY, Kim HY, Kang HK. Heterotopic pancreas in the stomach: CT findings. Radiology. 2000;217:139-144. |
| 14. | Laurent T, Fournier D, Doenz F, Karaaslan T, Wassmer FA. Complex lesion of the gastric wall: an unusual presentation of ectopic pancreas. J Clin Ultrasound. 1995;23:438-441. |
| 15. | Yasuda K, Cho E, Nakajima M, Kawai K. Diagnosis of submucosal lesions of the upper gastrointestinal tract by endoscopic ultrasonography. Gastrointest Endosc. 1990;36:S17-S20. |
| 16. | Rodriguez FJ, Abraham SC, Allen MS, Sebo TJ. Fine-needle aspiration cytology findings from a case of pancreatic heterotopia at the gastroesophageal junction. Diagn Cytopathol. 2004;31:175-179. |
| 17. | Dolan RV, ReMine WH, Dockerty MB. The fate of heterotopic pancreatic tissue. A study of 212 cases. Arch Surg. 1974;109:762-765. |
| 18. | Lai EC, Tompkins RK. Heterotopic pancreas. Review of a 26 year experience. Am J Surg. 1986;151:697-700. |
| 19. | McLean A, Fairclough P. Endoscopic ultrasound--current applications. Clin Radiol. 1996;51:83-98. |
| 20. | Matsushita M, Hajiro K, Okazaki K, Takakuwa H. Preoperative histological diagnosis of heterotopic pancreas. Dig Dis Sci. 1999;44:552. |