Published online Jul 14, 2008. doi: 10.3748/wjg.14.4257
Revised: May 23, 2008
Accepted: May 30, 2008
Published online: July 14, 2008
Biliary cystadenomas of the liver are rare, cystic neoplasms of the biliary ductal system usually occur in middle aged women. We report a case of synchronous multiple huge biliary mucinous cystadenomas with unique features. This is, according to our knowledge, the first report in the literature about three synchronously occurring hepatobiliary cystadenomas. Cystadenomas have a strong tendency to recur, particularly following incomplete excision, and a potential of malignant transformation. A therapeutic re-evaluation may be necessary when the diagnosis of hepatobiliary cystadenoma is made after the operation and an open liver resection should be considered.
- Citation: Manouras A, Lagoudianakis E, Alevizos L, Markogiannakis H, Kafiri G, Bramis C, Filis K, Toutouzas K. Laparoscopic fenestration of multiple giant biliary mucinous cystadenomas of the liver. World J Gastroenterol 2008; 14(26): 4257-4259
- URL: https://www.wjgnet.com/1007-9327/full/v14/i26/4257.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.4257
We have previously described a case of huge biliary cystadenoma in a middle aged woman and presented an extensive review of this uncommon entity[1]. We report, from the same institution, a case of synchronous, multiple, huge biliary mucinous cystadenomas with unique features.
A 70-year old woman presented in our institution with a 1-year history of low back pain. Abdominal ultrasonography revealed the presence of multiple hepatic cysts (the largest one measuring 16 cm in diameter) and cholelithiasis. Subsequent abdominal computer tomography (CT) scan showed multiple hepatic cysts in the right lobe of the liver and a smaller cyst in the left lobe (Figure 1). The cysts were unilocular, smooth, without septa but with homogeneous content. The cysts were well defined, had no irregular thickness, mural nodules or papillary projections. The radiological findings were consistent with simple liver cysts. Laboratory examination showed an elevation of CA 125 to 94.50 U/mL (reference value: ≤ 35 U/mL) and CA 15.3 to 45.10 U/mL (reference value: ≤ 35 U/mL), while carcinoembryonic antigen (CEA), α-fetoprotein (AFP) and CA19.9 were within the normal values.
The liver function tests and serum bilirubin levels were also within the normal range. The patient underwent a wide laparoscopic fenestration of the cysts and laparoscopic cholecystectomy, under general anaesthesia. Intraoperatively, three cysts were identified (Figure 2). Laparoscopic Lin fenestration[2] was performed following the decompression of the cysts with aspiration of their mucinous content. The cysts were unroofed and haemostasis was obtained with UltraCision harmonic scalpel. The frozen section examination was unrevealing. Finally, a typical laparoscopic cholecystectomy was performed. The postoperative period was uneventful. The patient was discharged on the second postoperative day.
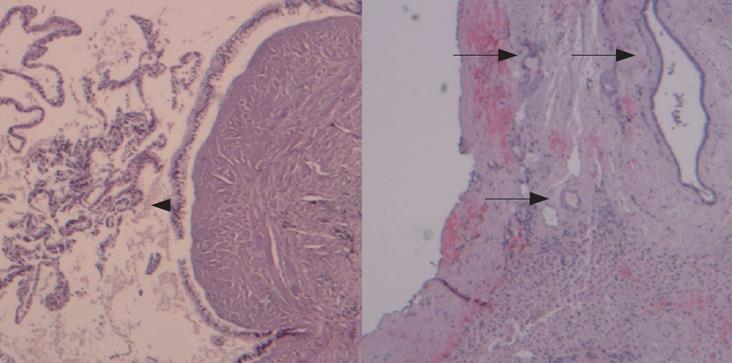
Pathologic evaluation of the paraffin-fixed material revealed that the cyst wall was comprised of a single layer of cuboidal-to-columnar epithelium, a moderately cellular stroma and an outer dense layer of collagenous connective tissue (Figure 3). These findings were consistent with cystadenoma without evidence of malignancy.
The pathologic examination of the specimen from the largest cyst, measuring 17 cm in diameter, showed papillary projections, internal smaller cysts, calcifications and hyaline degeneration of the stroma (Figure 4). These findings were not found in the smaller cysts and might represent the natural course of the cystadenoma. The absence of cellular atypia and intestinal metaplasia indicated the benign nature of this tumour.
The patient was informed about the possibility of malignant degeneration of the lesions and declined a further surgical intervention. No evidence of recurrence was found after a 6-mo follow-up period.
This is, according to our knowledge, the first report in the literature about three synchronously occurring hepatobiliary cystadenomas.
Hepatobiliary cystadenoma is an unusual cystic lesion, occurring more commonly in middle age women in the fifth decade of life and its size varies from 2 to 25 cm[34]. The exact etiology of biliary cystadenoma is unknown. The tumor is thought to result from the development of ectopic rests of primitive foregut sequestered within the liver or from the obstruction of the congenitally aberrant bile duct[5]. Malignant transformation is known to occur from hepatobiliary cystadenoma to cystadenocarcinoma[3].
The diagnosis of liver cyst can be easily made by ultrasonography, CT and magnetic resonance imaging (MRI). Hepatobiliary cystadenoma can be differentiated from simple cysts due to internal echogenic content or other ultrasonographic features[6]. However, in our patient, the differentiation of the cystadenomas from simple cysts was not possible by either ultrasound or even CT scan.
Radical excision of the tumor is the first choice of treatment. Operative removal is essentially important considering the high rate of recurrence (90%) if excision is not complete, and the possibility of a malignant transformation. Frozen sections are used to direct the surgical treatment but they can miss the diagnosis of hepatobiliary cystadenoma during a fenestration as was the case in our patient[7]. Thomas et al[8] reported that tumor recurrence occurs in two thirds of the patients, who have only local or pericystic excision. In contrast, only 10% of the patients, who have hepatic lobectomy, hemihepatectomy or radical excision of cystadenoma with a rim of normal tissue with a diameter of 2 cm, require further surgery for recurrence. Therefore, the detection of hepatobiliary cystadenoma after a laparoscopic surgical approach implies many challenging therapeutic dilemmas[89].
In conclusion, differential diagnosis of cystic lesions of the liver should always include hepatobiliary cystadenoma. There are no major reports addressing the diagnosis, treatment and follow-up outcome of laparoscopic surgery for hepatobiliary cystadenoma. A therapeutic evaluation may be necessary when the diagnosis of hepatobiliary cystadenoma is made after the operation and an open liver resection should be considered.
| 1. | Manouras A, Markogiannakis H, Lagoudianakis E, Katergiannakis V. Biliary cystadenoma with mesenchymal stroma: report of a case and review of the literature. World J Gastroenterol. 2006;12:6062-6069. |
| 2. | Lin TY. Hepatic tumors, surgical treatment and its results. Jpn J Surg. 1977;7:189-198. |
| 3. | Wheeler DA, Edmondson HA. Cystadenoma with mesenchymal stroma (CMS) in the liver and bile ducts. A clinicopathologic study of 17 cases, 4 with malignant change. Cancer. 1985;56:1434-1445. |
| 4. | Carson JG, Huerta S, Butler JA. Hepatobiliary cystadenoma: a case report and a review of the literature. Curr Surg. 2006;63:285-289. |
| 5. | Florman SS, Slakey DP. Giant biliary cystadenoma: case report and literature review. Am Surg. 2001;67:727-732. |
| 6. | Hsu KL, Chou FF, Ko SF, Huang CC. Laparoscopic fenestration of symptomatic liver cysts. Surg Laparosc Endosc Percutan Tech. 2005;15:66-69. |
| 7. | Fiamingo P, Veroux M, Cillo U, Basso S, Buffone A, D'Amico DF. Incidental cystadenoma after laparoscopic treatment of hepatic cysts: which strategy? Surg Laparosc Endosc Percutan Tech. 2004;14:282-284. |