Published online Jan 14, 2008. doi: 10.3748/wjg.14.260
Revised: November 14, 2007
Published online: January 14, 2008
AIM: To assess the role of echo-Doppler ultrasonography in postprandial hyperemia in cirrhotic patients by comparing the results with the hepatic vein catheterization technique.
METHODS: Patients with cirrhosis, admitted to the portal hemodynamic laboratory were included into the study. After an overnight fast, echo-Doppler ultrasonography (basal and 30 min after a standard meal) and hemodynamic studies by hepatic vein catheterization (basal, 15 min and 30 min after a standard meal) were performed. Ensure Plus (Abbot Laboratories, North Chicago, IL) was used as the standard liquid meal. Correlation analysis of the echo-Doppler and hepatic vein catheterization measurements were done for the basal and postprandial periods.
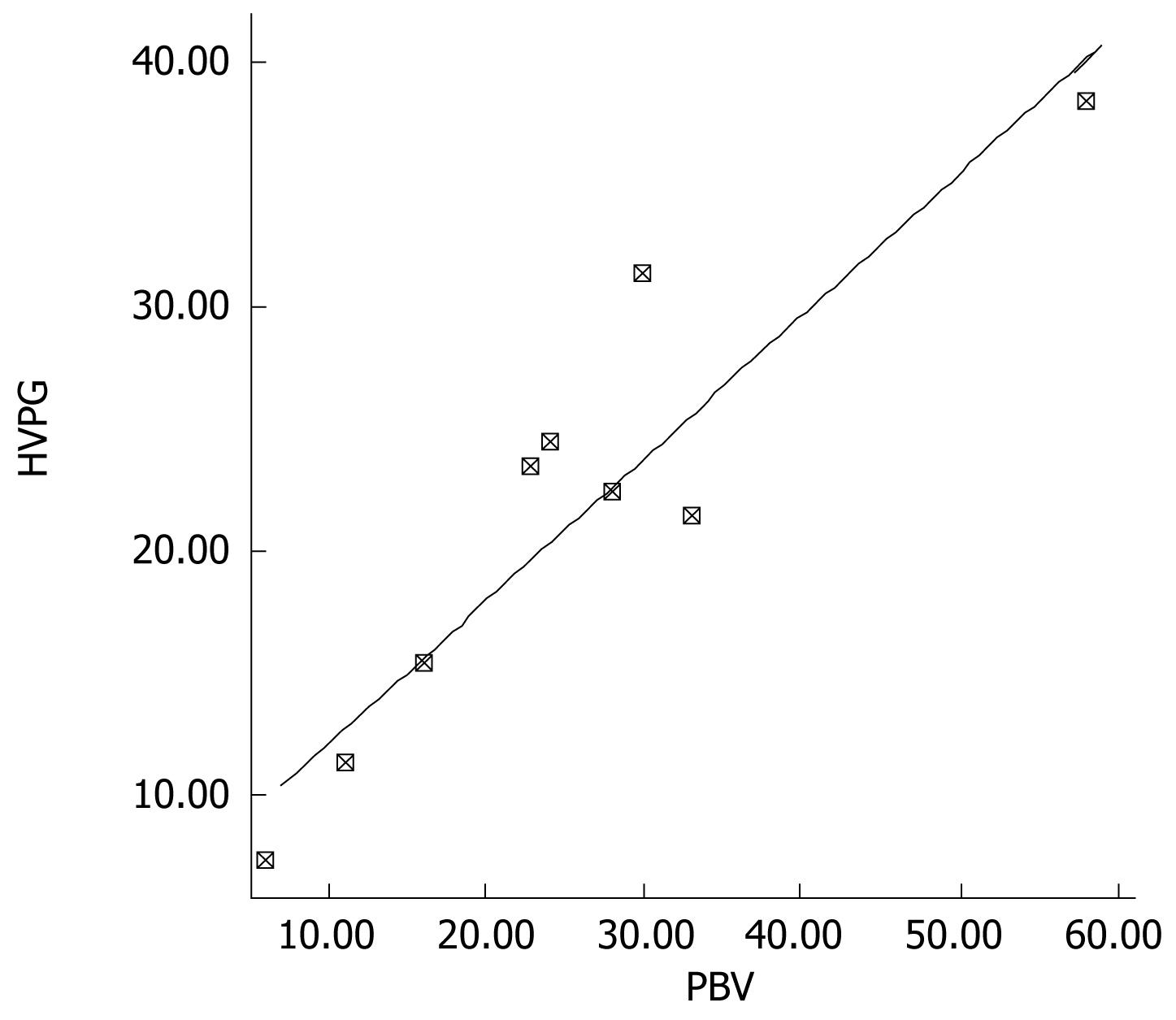
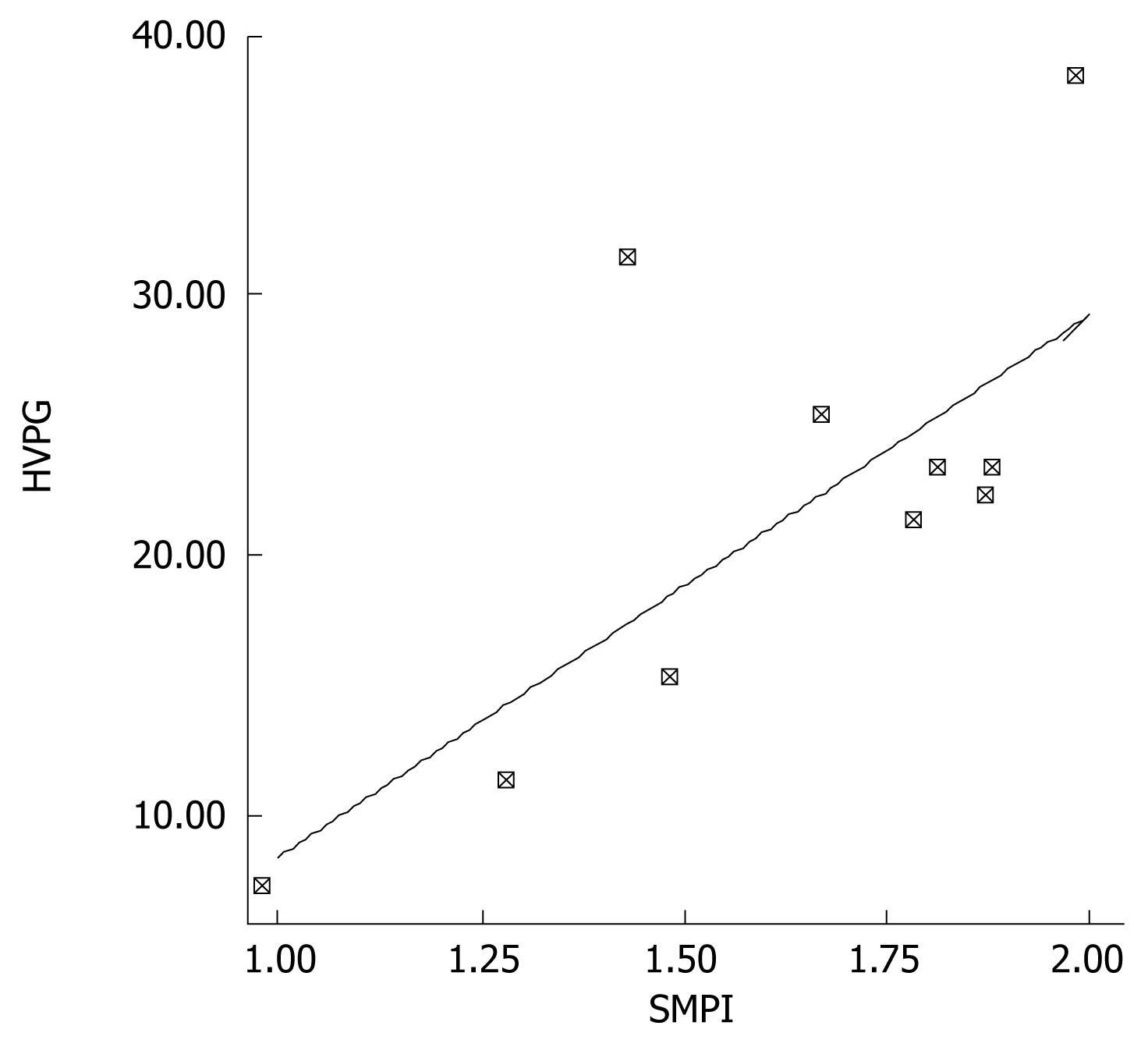
RESULTS: Eleven patients with cirrhosis (5 Child A, 4 Child B, 2 Child C) were enrolled into the study. After the standard meal, 8 of the 11 patients showed postprandial hyperemia with increase in portal blood flow, portal blood velocity and hepatic venous pressure gradient. Hepatic venous pressure gradient in the postprandial period correlated positively with postprandial portal blood velocity (r = 0.8, P < 0.05) and correlated inversely with postprandial superior mesenteric artery pulsatility index (r = -1, P < 0.01).
CONCLUSION: Postprandial hyperemia can be efficiently measured by echo-Doppler ultrasonography and the results are comparable to those obtained with the hemodynamic studies.
- Citation: Ozdogan O, Atalay H, Cimsit C, Tahan V, Tokay S, Giral A, Imeryuz N, Baltacioglu F, Tuney D, Erzen C, Tozun N. Role of echo Doppler ultrasonography in the evaluation of postprandial hyperemia in cirrhotic patients. World J Gastroenterol 2008; 14(2): 260-264
- URL: https://www.wjgnet.com/1007-9327/full/v14/i2/260.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.260
It is well known that portal pressure increases during the postprandial period. It is caused by an augmentation of blood flow into the splanchnic area, a phenomenon known as “postprandial hyperemia”[12]. In portal hypertensive patients, postprandial hyperemia may increase the variceal wall tension and trigger acute variceal bleeding. Therefore, an assessment of postprandial hyperemia (PPH) in cirrhotic patients may provide a better understanding of the pathophysiology of variceal bleeding, and consequently impact our treatment strategy.
Hepatic venous pressure gradient measurement by hepatic vein catheterization is the gold standard technique for the assessment of portal pressure changes in postprandial period in patients with cirrhosis[3]. However, this procedure is costly, is uncomfortable for the patients and is not available in every hepatology unit. By contrast, echo-Doppler ultrasonography (USG) is inexpensive, easy for the patients and is available in most hospitals. Sabba et al studied the sensitivity of echo-Doppler USG in detecting hemodynamic changes caused by postprandial hyperemia in an observer-blinded study. They found that echo-Doppler USG was highly sensitive for the evaluation of postprandial hyperemia[4]. Additionally, several studies have been done to investigate the effects of different drugs on postprandial hyperemia by using echo-Doppler USG[5–8]. However, to the best of our knowledge, there is no study which compares the hepatic venous catheterization with echo-Doppler USG in the assessment of PPH in patients with cirrhosis. Therefore, the aim of present study was to investigate the sensitivity of echo-Doppler USG in the assessment of PPH by comparing results with the gold standard test, hepatic vein catheterization.
All cirrhotic patients who were admitted to the portal hemodynamic laboratory of Marmara University School of Medicine, Department of Gastroenterology from November 2003 to March 2004, for the hemodynamic measurements before initiation of primary or secondary variceal bleeding prophylaxis were evaluated for the enrollment into the study. The exclusion criteria were age less than 18 or greater than 80 years, presence of hepatocellular carcinoma, coronary heart disease, hypertension, diabetes mellitus, portal vein thrombosis, refractory ascites, chronic lung disease, hepatic encephalopathy, hepatorenal syndrome and refusal to participate in the study.
The study was approved by the ethical committee of Marmara University School of Medicine and all patients gave written informed consent prior to participating in the study.
Diuretics and beta-blocker drugs were stopped 3 d before the study. After an overnight fast, baseline echo-Doppler (ATL, Ultramark 8 echo-Doppler duplex system) study was performed and the systolic (SBP), diastolic blood pressure (DBP) and heart rate (HR) were obtained. After these procedures, the patients were prepared for hepatic vein catheterization to obtain baseline hemodynamic measurements. Right hepatic vein catheterization was performed percutaneously through the jugular vein and the pressures were recorded in both the wedged and free position, using a balloon catheter (Medi Tech, Cooper Scientific Corp, Watertown, MA). The wedged position was controlled by the absence of reflux after the injection of 2 mL of contrast medium. Pressures were measured by a strain gauge transducer previously calibrated, and the findings were recorded on paper. Each pressure reading was recorded twice and the mean of the two values was used for the final result.
After the baseline measurements were obtained, a standard mixed liquid meal was given which consisted of 237 mL, of balanced dietary supplement (Ensure Plus, Abbot Laboratories, North Chicago, IL), containing 355 kcal as 14.7 g protein, 53.3 g carbohydrate and 32 g lipid. The meal was consumed over a period of 10 min. The mixed liquid meal was chosen because of ease of consumption, and standard formula and calorie intake. Hemodynamic measurements were repeated at 15, 30 and 60 min after the meal. At 30th min after the meal, echo-Doppler USG measurements were repeated simultaneously with the hemodynamic study. Because of technical difficulties (transport of the patients to the Doppler room), echo-Doppler USG could not be performed at the 15th and 60th min of postprandial period.
Mean arterial pressure (MAP) = (systolic + diastolic × 2)/3.
Hepatic venous pressure gradient (HVPG) = Wedge hepatic venous pressure (WHVP) - Free hepatic venous pressure (FHVP).
Portal Blood Flow (PBF) = Portal vein cross-sectional area (A) mm2× Portal blood velocity (PBV) cm/s.
An area was obtained from the cross-section of the vessel visualized by B-mode after defining the major and minor diameters of the vessel. Velocity measurements were performed in quiet suspended inspiration and averaged over a few seconds. These measurements were obtained from the longitudinal section of the vessel by positioning the sample volume cursor over the vessel at a known angle of insonation, defined as an angle between the Doppler beam and the long axis of the vessel. The Doppler sample volume probe was positioned over the middle of the vessel and was manipulated to cover about 90% of the vessel section in order to detect the maximum Doppler frequency shift, related to the maximum velocity (4).
According to the Doppler equation:
Δf = (2 foV max cos Q)/c
c: speed of the sound in the tissue
Q: angle between the ultrasound beam and the director of the blood flow (angle of insonation)
Vm = 0.57 × Vmax
Additionally, pulsatility index (PI) for the superior mesenteric artery (SMA) was measured according to the formula:
PI = Vmax - Vmin/Vmean
To decrease the inter-observer variability, all measurements were repeated 3 times by 2 different investigators and the mean value was used for statistical analysis.
Baseline results for the measurements are given as mean ± SE of absolute values. The values over time (Basal, 15 and 30 min after the test meal) were compared by ANOVA and the Student’s t test. Spearman correlation tests were done between the measurements of echo-Doppler USG and hemodynamic studies.
One hundred patients attending the hepatology outpatient clinic of the Marmara University Hospital were screened. However, only 11 patients were included in the study; the remainder were excluded due to factors such as clinical status, high Child-Pugh score, hematologic parameters, patients not providing informed consent and other exclusion criteria. The characteristics of the 11 patients are shown in Table 1. Eight out of the 11 patients showed postprandial hyperemia as judged by both echo-Doppler and hemodynamic studies, shown in Table 2. The maximum postprandial hyperemia was obtained at the 15 min. measurement by hepatic vein catheterization. Three patients did not show any increase in the hemodynamic or echo-Doppler parameters during the postprandial period (data not shown).
| Age | 48 ± 11.2 |
| Male/Female | 8/3 |
| Alcoholic etiology (yes/no) | 2/9 |
| Child-Pugh Score | 7.6 ± 2.3 |
| Child-Pugh Class (A/B/C) | 5/4/2 |
| History of variceal bleeding | |
| Yes | 6 |
| No | 5 |
| History of encephalopathy | |
| Yes | 4 |
| No | 7 |
| History of ascites | |
| Yes | 6 |
| No | 5 |
| History of SBP | |
| Yes | 2 |
| No | 9 |
| ALT (IU/L) | 52.27 ± 24.2 |
| Total protein (g/L) | 6.97 ± 0.9 |
| Albumin (g/d) | 3.52 ± 0.5 |
| PT (s) | 17.3 ± 2.9 |
| Total bilirubin (mg/dL) | 1.81 ± 0.5 |
| Baseline | Postprandial (15 min) | Postprandial (30 min) | P | |
| Hemodynamic measurements | ||||
| FHVP (mmHg) | 14.2 ±3.6 | 15.2 ± 4.1 | 15.9 ± 5.9 | NS |
| WHVP (mmHg) | 30.5 ± 7.6 | 38.7 ± 11.8b | 37.1 ± 10.4 | < 0.05 |
| HVPG (mmHg) | 16.5 ± 6.7 | 23.7 ± 11.1d | 21.2 ± 9.5 | < 0.05a |
| Echo-Doppler measurements | ||||
| PBF (L/min) | 1.5 ± 0.9 | 2.4 ± 1.1 | < 0.05 | |
| PBV (cm/s) | 23.5 ± 11.6 | 32.9 ± 12.3 | < 0.01 | |
| SMA-V (cm/s) | 120.2 ± 23.3 | 158.1 ± 59.9 | < 0.05 | |
| SMA-PI | 2.8 ± 0.5 | 1.7 ± 0.2 | < 0.05 | |
| Systemic measurements | ||||
| MAP (mmHg) | 85 ± 12.9 | 80 ± 9.6 | < 0.05 | |
| Pulse Rate (min) | 89.70 ± 21.2 | 85.3 ±13.3 | < 0.05 | |
When compared with the baseline parameters, there was a statistically significant difference in WHVP, HVPG, PBF, PBV, SMA-V, SAMA-PI, MAP and pulse rate at the 15th and 30th min of the postprandial period, with the portal vein velocity showing the highest increase (P < 0.01) (Table 2).
Spearman correlation tests were performed in order to evaluate the correlation between the echo-Doppler and hemodynamic parameters. Postprandial PBV showed a positive correlation with post-prandial HVPG values (r = 0.8, P < 0.05) (Figure 1), whereas SMA-PI showed an inverse correlation with the HVPG (r = -1, P < 0.01) (Figure 2). The percent increase in the echo-Doppler and hemodynamic measurements did not show any correlation between the echo-Doppler and hemodynamic tests.
The development of a non-invasive test for monitoring portal hemodynamics has been the subject of debate ever since the importance of portal pressure in cirrhotic patients was established. The increase in portal pressure in the postprandial period may initiate variceal bleeding in cirrhotic patients[9]. Therefore, it is important to identify patients who experience increased postprandial hyperemic response, and treat these patients appropriately. Echo-Doppler ultrasonography is a non-invasive test which is widely used to determine portal blood flow[47810] In an observer-blinded study, it was shown that echo-Doppler USG is highly sensitive in detecting post-prandial hemodynamic changes[4]. Since hepatic venous pressure gradient measurement is the gold standard for the evaluation of portal hemodynamic changes, the aim of the present study was to compare the results obtained with this technique with echo-Doppler ultrasonography.
We observed that patients who showed postprandial increase in HVPG also demonstrated an increase in the parameters by echo-Doppler ultrasonography. Initially, we did not find any correlation between the basal measurements obtained by echo-Doppler and hemodynamic studies. However, postprandial portal blood flow increased significantly in patients who showed significant postprandial HVPG increase. Moreover, correlation analysis showed a strong correlation between postprandial PBV and hepatic venous pressure gradient (Figure 1). The SMA index showed a negative correlation with the HVPG (Figure 2). However, we did not find any correlation between portal blood flow and hemodynamic measurements. Portal blood velocity and SMA-PI are both velocity measurements which were obtained by direct measurements. However, measurement of portal blood flow requires assessment of cross sectional portal vein area which depends on the position of the probe as well as that of the patient, which may result in marked variability of portal blood flow readings. It is difficult to explain the lack of correlation in the basal measurements obtained by echo-Doppler and hemodynamic studies, although there was a good correlation during the postprandial period. This may be due to individual differences in the basal parameters obtained by echo-Doppler studies, which is why the echo-Doppler studies cannot replace the gold standard hemodynamic studies in the primary and secondary prophylaxis of variceal bleeding.
Hepatic venous pressure gradient measurement is the gold standard for the evaluation of portal hemodynamics. To the best of our knowledge, the present study is the only one which has compared hepatic vein catheter and echo-Doppler measurements. Assessment of patients with significant increase in postprandial portal pressure allows the use of several treatment options. It was recently observed that administration of low dose isosorbide mononitrate attenuates postprandial hyperemia[10]. By contrast, propranolol is ineffective in blunting postprandial hyperemia but has some effect in reducing postprandial portal blood flow[11]. Somatostatin analogs have a favorable effect in reducing postprandial hyperemia in cirrhotic patients[12–14]. Most of these studies are performed by echo-Doppler measurement[81213].
Another unexpected finding in the present study was the absence of postprandial hyperemia in 3 patients (data not shown). These 3 patients showed more collateral vessels in the splanchnic area on echo-Doppler studies, compared to the other patients. In a recent study, it was shown that the extent of collateral circulation influences postprandial increase in portal pressure in patients with cirrhosis[15]. Other factors such as circadian rhythm, posture, age and gender did not have any effect in patients who failed to show a significant increase in postprandial pressure[16–20]. We believe that an increase in collateral circulation prevents postprandial rise in portal pressure despite increased blood flow in the splanchnic area.
In conclusion, if properly performed, echo-Doppler ultrasonography is a good test to measure postprandial portal hemodynamics. Future studies are needed to assess the usefulness of echo-Doppler measurements in primary and secondary prophylaxis of variceal bleeding.
Echo-Doppler USG is widely used for evaluation of the mechanisms of postprandial hyperemia in healthy people and cirrhotic patients, although the findings have not been validated.
This is the first study which investigated the validity of echo-Doppler USG in postprandial hyperemia by comparing the results with the gold standard test, hepatic vein catheterization.
Postprandial pressure and portal blood flow were evaluated in eleven patients enrolled from a cohort of cirrhotic patients, by hepatic vein catheterization and echo-Doppler USG at 15 min and 30 min after a standard liquid meal. Although, basal parameters did not show any correlation, hepatic venous pressure gradient and portal blood velocity showed a positive corelation in postprandial measurements.
Although there were some limitations in the present study, it can be stated that the evaluation of postprandial hemodynamic alterations can be performed safely by echo-Doppler USG, and the measurements obtained by echo-Doppler study reflect accurately the postprandial parameters in cirrhotic patients.
This is an experimental work conducted in humans, comparing hepatic vein catheterization with echodoppler measurement of post prandial hyperemia in cirrhotics. The authors conclude that the increased portal pressure observed in the post prandial period can be reliably measured by echo-doppler. The work is novel and may be clinically relevant.
| 1. | Lee SS, Hadengue A, Moreau R, Sayegh R, Hillon P, Lebrec D. Postprandial hemodynamic responses in patients with cirrhosis. Hepatology. 1988;8:647-651. |
| 2. | Gallavan RH Jr, Chou CC. Possible mechanisms for the initiation and maintenance of postprandial intestinal hyperemia.. Am J Physiol. 1985;249:G301-G308. |
| 3. | Tsunoda T, Ohnishi K, Tanaka H. Portal hemodynamic responses after oral intake of glucose in patients with cirrhosis. Am J Gastroenterol. 1988;83:398-403. |
| 4. | Sabba C, Ferraioli G, Genecin P, Colombato L, Buonamico P, Lerner E, Taylor KJ, Groszmann RJ. Evaluation of postprandial hyperemia in superior mesenteric artery and portal vein in healthy and cirrhotic humans: An operator blind echo-Doppler study. Hepatology. 1991;13:714-718. |
| 5. | Berzigotti A, Dapporto S, Angeloni L, Ramilli S, Bianchi G, Morelli MC, Magalotti D, Zoli M. Postprandial splanchnic haemodynamic changes in patients with liver cirrhosis and patent paraumbilical vein. Eur J Gastroenterol Hepatol. 2004;16:1339-1345. |
| 6. | Bartsch S, Bruning A, Reimann FM, Ludwig D. Haemodynamic effects of dopexamine on postprandial splanchnic hyperaemia. Eur J Clin Invest. 2004;34:268-274. |
| 7. | Sabba C, Buonamico P, Vendemiale G, Berardi E, Antonica G, Palmieri V, Merkel C, Palasciano G. Haemodynamic effects of propranolol, octreotide and their combination during fasting and postprandial splanchnic hyperaemia in patients with cirrhosis. Eur J Gastroenterol Hepatol. 2001;13:163-169. |
| 8. | Ludwig D, Schadel S, Bruning A, Schiefer B, Stange EF. 48-hour hemodynamic effects of octreotide on postprandial splanchnic hyperemia in patients with liver cirrhosis and portal hypertension: double-blind, placebo-controlled study. Dig Dis Sci. 2000;45:1019-1027. |
| 9. | Albillos A, Banares R, Gonzalez M, Catalina MV, Pastor O, Gonzalez R, Ripoll C, Bosch J. The extent of the collateral circulation influences the postprandial increase in portal pressure in patients with cirrhosis. Gut. 2007;56:259-264. |
| 10. | Bellis L, Berzigotti A, Abraldes JG, Moitinho E, Garcia-Pagan JC, Bosch J, Rodes J. Low Doses of isosorbide mononitrate attenuate the postprandial increase in portal pressure in patients with cirrhosis. Hepatology. 2003;37:378-384. |
| 11. | Sabba C, Ferraioli G, Buonamico P, Mahl T, Taylor KJ, Lerner E, Albano O, Groszmann RJ. A randomized study of propranolol on postprandial portal hyperemia in cirrhotic patients. Gastroenterology. 1992;102:1009-1016. |
| 12. | Mottet C, Sieber CC, Nauer A, Drewe J, Fried R, Larsen F, Beglinger C. Hemodynamic effects of the somatostatin analog lanreotide in humans: placebo-controlled, cross-over dose-ranging Echo-Doppler study. Hepatology. 1998;27:920-925. |
| 13. | Ludwig D, Terai S, Bruning A, Stange EF. Long-term haemodynamic effects of octreotide on postprandial splanchnic hyperemia in humans: a placebo-controlled echo-doppler study. Aliment Pharmacol Ther. 1999;13:1119-1129. |
| 14. | Sakurabayashi S, Koh KC, Chen L, Groszmann RJ. Octreotide ameliorates the increase in collateral blood flow during postprandial hyperemia in portal hypertensive rats. J Hepatol. 2002;36:507-512. |
| 15. | Albillos A, Banares R, Gonzalez M, Catalina MV, Pastor O, Gonzalez R, Ripoll C, Bosch J. The extent of the collateral circulation influences the postprandial increase in portal pressure in patients with cirrhosis. Gut. 2007;56:259-264. |
| 16. | Schiedermaier P, Koch L, Mojon A, Hermida R, Layer G, Sauerbruch T. Circadian rhythm of fasting and postprandial portal blood flow in cirrhosis. Scand J Gastroenterol. 2006;41:826-832. |
| 17. | Iwao T, Oho K, Nakano R, Yamawaki M, Sakai T, Sato M, Miyamoto Y, Sakai K, Sata M, Toyonaga A. Upright posture blunts postprandial splanchnic hyperemia in patients with cirrhosis and portal hypertension. J Gastroenterol. 1999;34:359-365. |
| 18. | Iwao T, Toyonaga A, Sato M, Oho K, Sakai T, Tayama C, Nakano R, Tanikawa K. Effect of posture-induced blood volume expansion on systemic and regional hemodynamics in patients with cirrhosis. J Hepatol. 1997;27:484-491. |
| 19. | Bernardi M, Fornalè L, Di Marco C, Trevisani F, Baraldini M, Gasbarrini A, De Collibus C, Zacà F, Ligabue A, Colantoni A. Hyperdynamic circulation of advanced cirrhosis: a re-appraisal based on posture-induced changes in hemodynamics. J Hepatol. 1995;22:309-318. |
| 20. | Moller S, Nørgaard A, Henriksen JH, Frandsen E, Bendtsen F. Effects of tilting on central hemodynamics and homeostatic mechanisms in cirrhosis. Hepatology. 2004;40:811-819. |