Published online Apr 7, 2007. doi: 10.3748/wjg.v13.i13.1930
Revised: December 3, 2006
Accepted: December 20, 2006
Published online: April 7, 2007
Caroli’s disease is a rare congenital condition chara-cterized by non-obstructive saccular or fusiform dilatation of larger intrahepatic bile ducts. Cholangitis, liver cirrhosis, and cholangiocarcinoma are its potential complications. The diagnosis of Caroli’s disease depends on demonstrating that the cystic lesions are in continuity with the biliary tree which can be showed by ultrasonography, computerized tomography, endoscopic retrograde cholangiopancreatography, percutaneous transhepatic cholangiography or magnetic resonance cholangiopancreatography. Treatment of Caroli’s disease relies on the location of the biliary abnormalities. While localized forms confined to one lobe can be treated with surgery, liver transplantation is the only effective modality for diffuse forms. Although a rare disorder; Caroli’s disease should always be considered in the differential diagnosis of chronic cholestasis of unknown cause.
- Citation: Yonem O, Bayraktar Y. Clinical characteristics of Caroli’s disease. World J Gastroenterol 2007; 13(13): 1930-1933
- URL: https://www.wjgnet.com/1007-9327/full/v13/i13/1930.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i13.1930
Caroli’s disease (CD) was first described by Caroli as a congenital malformation of intrahepatic bile ducts, characterized by segmental cystic dilatation of the intrahepatic ducts; increased incidence of biliary lithiasis, cholangitis and liver abscesses; absence of cirrhosis and portal hypertension; and association of renal tubular ectasia or similar renal cystic disease[1]. Mode of inheritance is still unclear but in majority of cases it is transmitted in autosomal recessive fashion[2]. Review of the literature suggests that there are no large series of this disease[3]. Although present from birth, the disease usually remains asymptomatic during the first 20 years, and may also remain so throughout life. However when symptomatic, a significant number of these patients present significant loss in their quality of life and their clinical course frequently worsen due to the repeated episodes of cholangitis with the presence of intrahepatic calculi, intrahepatic abscesses and sepsis[4].
Until 1984, 162 cases of Caroli disease had been reported[1]. The estimated incidence of Caroli’s disease is 1 in 1 000 000 population[5]. Males and females are equally affected and more than 80% of patients present before 30 years of age[1].
The cause of CD is unknown but occasional familial clustering suggests that some cases are inherited, in particular when CD occurs with Polycystic kidney disease[6]. In one study liver biopsies of patients with Caroli’s disease were cytogenetically analyzed and an unbalanced translocation between chromosome 3 and 8 was detected and suggested that loss of distal 3p and/or gain of 8q could be of pathogenetic importance in CD[7]. The likely mechanism involves an in utero event that makes a derangement in the normal embryologic remodelling of ducts and causes varying degrees of destructive inflammation and segmental dilatation[8].
The clinical course can be asymptomatic for the first 5-20 years or symptoms can occur infrequently throughout the patient’s life[9]. Intrahepatic ductal ectasia predisposes to stagnation of the bile which may lead to the formation of stones and favour infections such as cholangitis, abscess or even septicaemia. However this disease is frequently noted by recurrent fever, jaundice and/or pain in the right hypochondrium. A literature review found recurrent acute cholangitis as the main mode of presentation in 64% of the patients[5]. The notion of isolated choledochal lithiasis in the absence of gallbladder lithiasis should lead us think about an intrahepatic lithogenic focus and, consequently about Caroli’s disease[4].
Patients with CD and congenital hepatic fibrosis can present with portal hypertension and its sequelae such as ascites and esophageal varice hemorrhage. Histological intra hepatic bile duct ectasia and proliferation are associated with severe periportal fibrosis. On physical examination the liver is frequently enlarged and the spleen becomes palpable as portal hypertension develops.
Laboratory studies typically show an elevation of serum alkaline phosphatase, direct bilirubin and a leucocytosis with a predominance of neutrophils. Hepatic synthetic function is well-preserved initially, but may be affected by progressive liver damage due to recurrent cholangitis and biliary obstruction. Coagulopathy from vitamin K malabsorbtion may occur in cholestatic patients[10].
Histologically, the main macroscopic and microscopic features of CD are: non-obstructive, localized dilatation of the bile ducts, intraluminal bulbar protrusions of the ductal wall and intra ductal vascular tracts containing patent portal venous and hepatic arterial channels that traverse the true lumen and terminate within the lumen[11]. The diagnosis of CD therefore rests on demonstrating that the cystic lesions are in continuity with the biliary tree. It can be done by imaging studies such as abdominal USG, CT scan, and isotope scan, ERCP, PTC and MRCP. The classical finding of CD is finding of a cold area on 99 m TC sulphur colloid scan becoming hot on 99 m Tc DISIDA scan[12].
USG and CT studies may visualize liver cysts and possible intrahepatic lithiasis and provide information on the common bile duct, but differentiation from other liver cysts such as polycystic liver disease is often difficult[6].
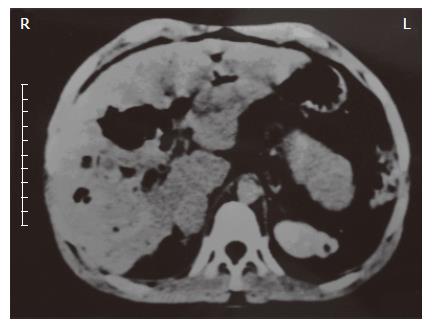
CT scan shows central dot signs in CD patients. The fibrovascular bundles containing portal vein radical and a branch of hepatic artery bridging the saccule appear as central dots or linear streak. This central dot sign described on CT scan is suggested as a pathognomic finding in CD and it can also be demonstrated on USG. ERCP is the method with the highest sensitivity in the diagnosis of CD. The cholangiographic features of Caroli’s disease are well established as saccular or fusiform dilatation of the intrahepatic bile ducts. These findings can also be seen on computed tomography (Figure 1). Irregular bile duct walls, strictures and stones may be present. Therefore, direct cholangiography is considered the method of choice for an accurate diagnosis of Caroli’s disease. However serious complications (sepsis, bile leak, bleeding and death) may occur with both ERCP and PTC, with an overall incidence of approximately 3%. MRCP is a noninvasive technique that has shown good correlation with ERCP in diagnosing biliary tract abnormalities without any of the risks seen with invasive procedures. The ability to demonstrate the intrahepatic ductal anatomy makes MRCP a reliable diagnostic tool in Caroli’s disease, providing that acceptable image quality can be maintained[13].
The differential diagnosis for patients exhibiting the symptoms of CD is broad and includes PSC, recurrent pyogenic cholangitis, polycystic liver disease, a choledochal cysts, biliary papillomotosis and occasionally obstructive biliary dilatation. PSC and recurrent pyogenic cholangitis may be associated with ductal dilatation, stenosis, intrahepatic calculi and malignancy. However the ductal dilatation in PSC is rarely saccular and is typically more isolated and fusiform, which is not characteristic of CD. Additionally 70% of white patients with PSC have coexisting inflammatory bowel disase. Patients with polycystic liver disease may present with both hepatic and renal cysts. However, the hepatic cysts of polycystic liver only rarely communicate with the bile ducts. These patients have typically intrinsically normal bile ducts.
Recurrent pyogenic cholangitis is the most difficult diagnosis to exclude because patients with pyogenic cholangitis present with sepsis and have intra- and extrahepatic biliary dilatation. The presence of saccular dilatation favors the diagnosis of Caroli’s disease because saccular dilatation is unusual in recurrent pyogenic cholangitis[8]. Both Caroli’s disease and choledochal cyst are inherited anomalies of the bile ducts but Caroli’s disease involves the congenital dilation of the segmental intrahepatic biliary tree, whereas choledochal cysts involve the cystic dilation of the common bile duct[1].
Caroli’s disease often coexists with congenital hepatic fibrosis and is then designated Caroli’s syndrome. Both result from malformations of the embryonic ductal plate at different levels of the biliary tree[14]. If the defective remodelling involves the larger intrahepatic ducts Caroli’s disease develops, but when the entire intrahepatic bilary tree is involved the condition is Caroli’s syndrome[15]. Incidence of Caroli’s syndrome is more than Caroli’s disease[2]. In addition, various renal disorders may be ssen in conjunction with these hepatic diseases, including autosomal polycystic kidney disease (both dominant and recessive forms), medullary sponge kidney and medullary cystic disease[7]. Between the times 1971-2005 we have followed-up 10 patients with Caroli’s disease. Of these, 4 had isolated Caroli’s disease while the remaining 6 patients had Caroli’s syndrome. Among the patients with Caroli’s syndrome; 2 patients had Cavernomatous transformation of portal vein and 2 had polycystic kidney disease as an associated condition. One of these patients died due to sepsis and two of them underwent liver transplantation because of the development of secondary biliary cirrhosis[16].
Despite the advances made in medical, endoscopic and surgical treatments over the last 3 decades, they have not yet been sufficiently effective to allow sustained recovery from the symptoms of CD. The evolution of CD is dominated by the occurrence of repetitive bouts of cholangitis, the frequency of which may vary importantly from one patient to another. In case of frequent episodes of cholangitis, the long term prognosis is poor and these patients graduately lose their quality of life at a usually productive age[6]. Caroli’s disease can be complicated by the formation of liver abscesses, intra- and extrahepatic lithiasis and even cholangiocarcinoma[17].
The incidence of cancer associated with congenital cysts of bile ducts has been reported to be between 2.5% and 16% and appears to be associated with biliary stasis, the action of the carcinogenic substances contained in the bile and chronic inflammation of the biliary epithelium, leading to dysplastic diseases[4]. Amyoidosis is also described as another complication of Caroli’s disease. Death is related to septicaemia and hepatic abscesses[18].
The treatment of CD depends on the clinical features and the location of the biliary abnormalities. The localized forms, which involve the whole of the left half of the liver, or the right half of the liver, are curable by surgery. They should be treated by hemi-hepatectomy with associated treatment of any problem affecting the common duct[19]. Diffuse involvement of both lobes can be treated with conservative management, (Appropriate antibiotics for cholangitis and ursodeoxycolic acid therapy for litholysis in case of intrahepatic cholelithiasis), endoscopic therapy (sphincterotomy for clearance of intrahepatic stones) and internal biliary bypass procedure[15].
Surgery can offer a definite therapy, with an acceptable morbidity in localized CD[20]. Symptomatic relief after partial hepatectomy is often complete and permanent. Bilateral disease complicated by recurrent cholangitis, cirrhosis or both do not find the same solution and is often difficult to manage. Emergency surgery in the presence of acute cholangitis and deteriorating liver function is associated with high mortality (20%-40%) and morbidity (44%-80%). So it seems that liver transplantation is the only and ultimate management option for these patients even if they are asymptomatic[6]. Survival after liver transplantation was found to be poor in patients with congenital hepatic fibrosis (Caroli’s syndrome) and in those who had cholangitis at the time of the ortotopic liver transplantation in one study[21].
The role of liver transplantation for cholangiocarcinoma whether associated with CD or not is controversial. Because of the high rate of recurrence published previously, most centers have abandoned cholangiocarcinoma as an indication for liver transplantation[6].
As a result CD is an inherited disorder which may cause severe, life threatening cholangitis or which may lead to hepatobiliary degeneration[17]. But CD can be misdiagnosed due to the lack of experience in low volume hospitals where the symptoms of this disease have been repeatedly treated and where many of the diverse modern imaging techniques are unavailable. For this reason despite its rare incidence; Caroli’s disease should not be forgotten in the differential diagnosis of recurrent cholangitis.
S- Editor Wang J L- Editor Lutze M E- Editor Che YB
| 1. | Lu SC, Debian KA. Cystic diseases of the biliary tract. Textbook of Gastroenterology. Philadelphia: Lippincott Williams and Wilkins 2003; 2225-2233. |
| 2. | Gupta AK, Gupta A, Bhardwaj VK, Chansoria M. Caroli's disease. Indian J Pediatr. 2006;73:233-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Madjov R, Chervenkov P, Madjova V, Balev B. Caroli's disease. Report of 5 cases and review of literature. Hepatogastroenterology. 2005;52:606-609. [PubMed] |
| 4. | Waechter FL, Sampaio JA, Pinto RD, Alvares-da-Silva MR, Cardoso FG, Francisconi C, Pereira-Lima L. The role of liver transplantation in patients with Caroli's disease. Hepatogastroenterology. 2001;48:672-674. [PubMed] |
| 5. | Giovanardi RO. Monolobar Caroli's disease in an adult. Case report. Hepatogastroenterology. 2003;50:2185-2187. [PubMed] |
| 6. | Kassahun WT, Kahn T, Wittekind C, Mössner J, Caca K, Hauss J, Lamesch P. Caroli's disease: liver resection and liver transplantation. Experience in 33 patients. Surgery. 2005;138:888-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 75] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Parada LA, Hallén M, Hägerstrand I, Tranberg KG, Johansson B. Clonal chromosomal abnormalities in congenital bile duct dilatation (Caroli's disease). Gut. 1999;45:780-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Levy AD, Rohrmann CA, Murakata LA, Lonergan GJ. Caroli's disease: radiologic spectrum with pathologic correlation. AJR Am J Roentgenol. 2002;179:1053-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 90] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Wu KL, Changchien CS, Kuo CM, Chuah SK, Chiu YC, Kuo CH. Caroli's disease - a report of two siblings. Eur J Gastroenterol Hepatol. 2002;14:1397-1399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Suchy FJ. Caroli's disease. Uptodate 2006 Version 14.1. . |
| 11. | Keramidas DC, Kapouleas GP, Sakellaris G. Isolated Caroli's disease presenting as an exophytic mass in the liver. Pediatr Surg Int. 1998;13:177-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Sharma R, Mondal A, Taneja V, Rawat HS. Radionuclide scintigraphy in Caroli's disease. Indian J Pediatr. 1997;64:105-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Asselah T, Ernst O, Sergent G, L'herminé C, Paris JC. Caroli's disease: a magnetic resonance cholangiopancreatography diagnosis. Am J Gastroenterol. 1998;93:109-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Sherlock S, Dooley J. Diseases of the liver and billiary system. 11th ed. Milano: Blackwell Sci Pub 2002; 583. |
| 15. | Desmet VJ. Pathogenesis of ductal plate malformation. J Gastroenterol Hepatol. 2004;19:S356-S360. [DOI] [Full Text] |
| 16. | Yönem O, Ozkayar N, Balkanci F, Harmanci O, Sökmensüer C, Ersoy O, Bayraktar Y. Is congenital hepatic fibrosis a pure liver disease. Am J Gastroenterol. 2006;101:1253-1259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | De Kerckhove L, De Meyer M, Verbaandert C, Mourad M, Sokal E, Goffette P, Geubel A, Karam V, Adam R, Lerut J. The place of liver transplantation in Caroli's disease and syndrome. Transpl Int. 2006;19:381-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 61] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Patil S, Das HS, Desai N, Manjunath SM, Thakur BS, Sawant P. Caroli's syndrome--a rare cause of portal hypertension. J Assoc Physicians India. 2004;52:261. [PubMed] |
| 19. | Yilmaz S, Kirimlioglu H, Kirimlioglu V, Isik B, Coban S, Yildirim B, Ara C, Sogutlu G, Yilmaz M. Partial hepatectomy is curative for the localized type of Caroli's disease: a case report and review of the literature. Surgeon. 2006;4:101-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Bockhorn M, Malagó M, Lang H, Nadalin S, Paul A, Saner F, Frilling A, Broelsch CE. The role of surgery in Caroli's disease. J Am Coll Surg. 2006;202:928-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Habib S, Shakil O, Couto OF, Demetris AJ, Fung JJ, Marcos A, Chopra K. Caroli's disease and orthotopic liver transplantation. Liver Transpl. 2006;12:416-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 49] [Article Influence: 2.6] [Reference Citation Analysis (0)] |