Published online Mar 14, 2007. doi: 10.3748/wjg.v13.i10.1522
Revised: December 30, 2006
Accepted: February 25, 2007
Published online: March 14, 2007
AIM: To determine, for hepatocellular carcinoma (HCC), the patient demographic profile and costs of their admissions to the hospitals of the Portuguese National Health System from 1993 to 2005.
METHODS: The National Registry (ICD-9CM, Inter-national Classification of Diseases, 155.0) provided data from the 97 Hospitals in Portugal.
RESULTS: We studied 7932 admissions that progres-sively rose from 292 in 1993 to 834 in 2005, having a male predominance of 78% (6130/7932). The global rate of hospital admissions for HCC rose from 3.1/105 in 1993 to 8.3/105 in 2005. The average length of stay decreased from 17.5 ± 17.9 d in 1993 to 9.3 ± 10.4 d in 2005, P < 0.001. The average hospital mortality for HCC remained high over these years, 22.3% in 1993 and 26.7% in 2005. Nationally, hospital costs (in Euros - €) rose in all variables studied: overall costs from €533 000 in 1993, to €4 629 000 in 2005, cost per day of stay from €105 in 1993, to €597 in 2005, average cost of each admission from €1828 in 1993, to €5550 in 2005. In 2005, 1.8% (15/834) of hospital admissions for HCC were related to liver transplant, and responsible for a cost of about €1.5 million, corresponding to one third of the overall costs for HCC admissions in that same year.
CONCLUSION: From 1993 to 2005 hospital admissions in Portugal for HCC tripled. Overall costs for these admissions increased 9 times, with all variables related to cost analysis rising accordingly. Liver transplant, indicated in a small group of patients, showed a disproportionate increase in costs.
- Citation: Marinho RT, Giria J, Moura MC. Rising costs and hospital admissions for hepatocellular carcinoma in Portugal (1993-2005). World J Gastroenterol 2007; 13(10): 1522-1527
- URL: https://www.wjgnet.com/1007-9327/full/v13/i10/1522.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i10.1522
Hepatocellular carcinoma (HCC) is now a major public health problem. It is one of the most frequently occurring malignant tumors throughout the world, being the third cause of death from cancer in men.
The mortality of HCC is particularly elevated in Africa and Asia[1,2]. In the last years there has been an increasing mortality due to HCC in Western Europe,[3,4] the United States of America[5] and Japan[6,7].
In the great majority of cases, HCC appears in patients who have liver cirrhosis, especially in those regions of relatively low incidence as Western Europe. Liver cirrhosis is a chronic disease carrying a high oncogenic risk, with a rate of evolution to HCC at an annual incidence of 1%-4%[8]. HCC has a poor prognosis but the three main situations that cause it are amenable to prevention, i.e. hepatitis B[9,10] and C[11,12] infections, and excessive alcohol consumption[13]. Increasing rates of hepatitis C virus (HCV) infection could explain a proportion of the reported increase in HCC incidence during the last decade[14]. Liver transplant in selected cases is an effective option for patients with HCC. The percentage of HCC cases considered for liver transplant, for both on the waiting list and those already transplanted, has also been increasing, resulting in mounting costs to the health system for the management of these patients[15].
Databases of hospital admissions, obtained from patient classification systems that are based on principal diagnosis of discharge episode, may be used to measure the morbidity of the inpatient population and the demand that certain diseases make on health systems[16]. We used the Diagnosis-Related Groups (DRG)[17] database to classify inpatients according to epidemiological variables of sex, age, principal and associated diagnoses, technical procedures carried out for diagnosis, mortality, and location of hospital admission[18]. In addition, this database allows for the tracking of variables of resource consumption i.e. length of stay, costs per day according to the type of episode, and costs of episode of hospital admission. Economic analysis of chronic diseases is a prerequisite for planning a proper distribution of health care resources.
Using such data, the aim of this work was to determine the profile of patients with HCC, and the costs of their hospital admissions during the period between 1993 and 2005 to the 97 public hospitals of the National Health System of Portugal, serving now a population of about 10 million inhabitants.
We studied the demographic data and resource consumption of hospital admissions for HCC to the 97 hospitals of the National Health System in Portugal during the period of 1993 to 2005.
The study is descriptive, based on the DRG database. We used the International Classification of Diseases, Ninth Revision, Clinical Modification, (ICD-9-CM), primary liver tumor (155.0), and evaluated the following variables: gender, age, mortality, length of stay, overall costs, costs per day and per episode of hospital admission, and costs related to liver transplant in HCC.
The population of Portugal and number of deaths for HCC were obtained from the “Instituto Nacional de Estatística (INE)”.
Specific rates for 100 000 were calculated by age group and gender.
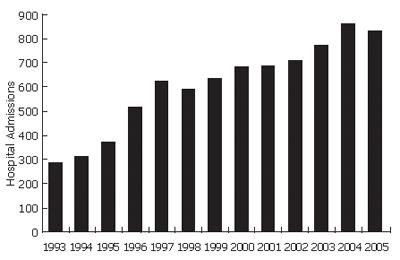
In the period 1993-2005, 7932 hospital admissions for HCC were registered in Portugal. A progressive 2.9 fold increase was verified in the period studied: 292 hospital admissions in 1993, 635 in 1999 and 834 in 2005 (Figure 1).
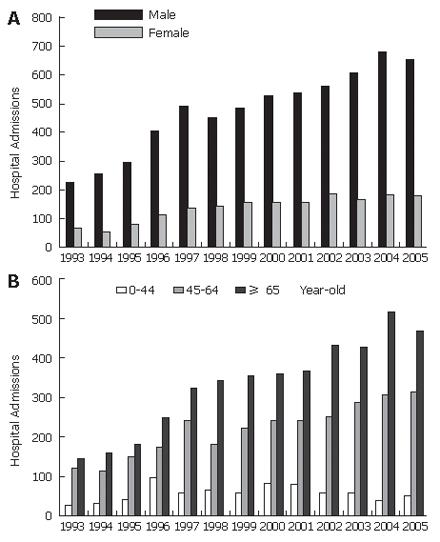
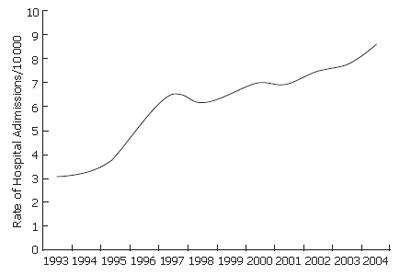
Gender distribution data showed a 77.6% (6155/7932) predominance of male patients, at a ratio of 3.4:1 in 1993, and 3.6:1 in 2005 (Figure 2A). This percentage has remained stable over the years: 77.1% in 1993, and 78.2% in 2005. The evolution of episodes of hospital admission per 100 000 inhabitants similarly showed a progressive increase from 3.1 × 105 (men 4.9, women 1.4) in 1993, to 8.6 × 105 in 2005 (13.4 in men and 3.5 in women) (Figure 3).
The average age for hospital admission was 62.0 ± 16.4 years in 1993, and 63.9 ± 13.3 in 2005. Most hospital admissions occurred in patients older than 64 years, increasing from 49.3% (144/292) in 1993 to 55.8% (466/834) in 2005, P = NS. Findings for all age groups showed that 54.5% (4319/7932) were older than 64 years, 36.0% (2853/7932) were between 45-64 years and only 9.6% (760/7932) were between 0-44 years. The rate of hospital admission per 100 000 in the age groups of 0-44, 45-64 and over 64-years was respectively 0.5, 5.5 and 10.4 in 1993 and 0.9, 12.5 and 26.7 in 2005 (Figure 2B).
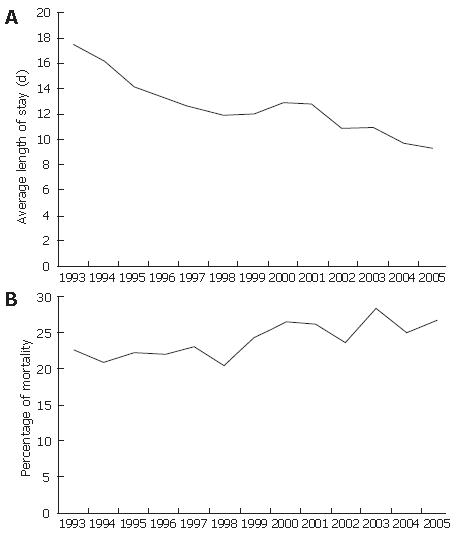
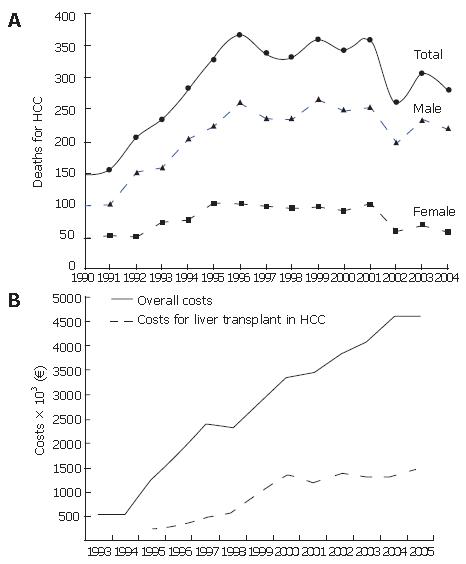
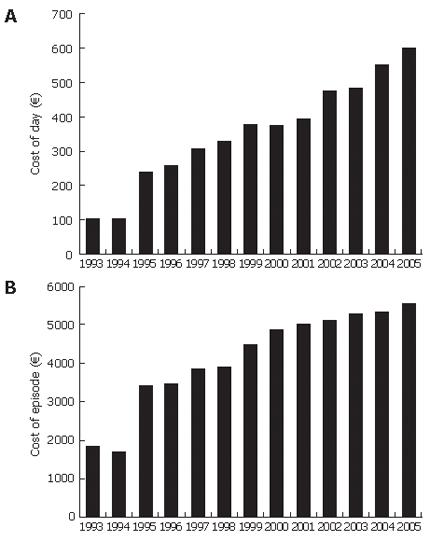
The average length of stay for HCC was higher than the national average (9.0 d in 1993 and 7.7 d in 2005) but it has shown a decrease from 17.5 d in 1993 to 9.3 d in 2005, P < 0.05 (Figure 4A). Hospital mortality for HCC remained very high, 22.6% in 1993 and 26.7% in 2005 (Figure 4B). As would be expected, the mortality was higher in older patients, 12.5% in the group 0-44 years-old, 27.3% in 45-64 years, and 28.3% in patients older than 64 years. In addition, the figures given by the National Institute of Statistics for inpatient and outpatient mortality for HCC in Portugal showed an increase, from 149 deaths in 1990, to 280 in 2004 (Figure 5A). In determining the costs for hospital admissions for HCC in the Portuguese Health System, we found a significant increase for all economic variables studied. The overall costs of hospital admissions increased 8.7 times, from €533 000 in 1993, to €4 629 000 in 2005 (Figure 5B). In the same period the average cost of each day of hospital admission 5.7 times from €105 in 1993, to €597 in 2005 (Figure 6A). The average cost of each stay in hospital for HCC increased 3 times from €1828 in 1993, to €5550 in 2005 (Figure 6B)
Liver transplants in Portugal began in 1992. Of all liver transplants performed between 1992 and 2005, 7.2% (117/1619) were liver transplants for HCC. But, this percentage almost tripled from 3.3% in 1993 (1/30) to 9.0% in 2005 (15/166), P = NS. Today, costs for hospital admissions for patients transplanted with the indication of HCC are 32.5% of the total costs for all hospital admissions for HCC (Figure 5A).
These means, in effect, that the costs for 15 patients with HCC transplanted in Portugal in 2005 represent one third of the costs for all 834 hospital admissions for HCC in that same year.
The number of patients diagnosed with HCC has been increasing in Japan[19], the United States[20,21], and Europe[22]. HCC particularly affects patients who have liver cirrhosis. The characteristics of liver cirrhosis that lead to HCC, namely its frequent complications and instability, are associated with multiple episodes of hospital admissions[23], mainly in the phase of decompensation (ascites, jaundice, spontaneous peritonitis and encephalopathy).
Our work revealed a 2.9 fold increase in hospital admissions for HCC in Portugal over the twelve years studied (1993-2005), reaching 834 hospital admissions in 2005 (8.6/105). As some patients are admitted to hospital several times each year, these figures do not correspond to the real incidence of HCC. A recent study in United States has documented a similar increase in the hospital admissions for HCC[24].
Male gender has also been documented as a risk factor for HCC, and the male/female ratio is usually 2 to 3:1[25]. Our data is in accord with this ratio: 78% of hospital admissions were for male patients, and in spite of the increase in numbers for both genders, the male/female ratio was 3.5:1 in the period studied.
HCC has been found to be more frequent in indivi-duals in their sixties[26]. The average age of patients admitted to hospitals in Portugal for HCC was 61.2 ± 16.7 years in 1993, and 63.9 ± 13.5 years-old in 2005. More than half of hospital admissions now occur in patients older than 64, increasing from 49.3% (144/292) in 1993, to 55.8% (466/834) in 2005, P = NS. When we analyzed the rate of hospital admissions per 100.000 inhabitants, the higher rates were found to be more elevated in patients older than 64 (26.7/105 in 2005). This rate is higher than the group 45 to 64-years-old (12.5/105). The rarity in younger ages is evident: in the group 0-44 years-old was 0.9/105 in 2005. The rate of hospital admissions increased in all groups of patients, but more in the older ones: 1.8 times more (0.5/105 in 1999 to 0.9/105 in 2005), 2.3 times more (5.5/105 to 12.5/105) and 2.6 times more (10.4/105 to 26.7/105) respectively, in patient groups 0-44, 45-64 and over 64-year-old in 1993 and in 2005. Several studies, notably in Scotland, Denmark, France, and Japan have found the same tendency, corroborating our findings that HCC occurs mainly in patients older than 65 years-old[27,28].
The demographic data and rate of mortality (Ministry of Health 2003) by Chronic Liver Disease and Cirrhosis (ICD-9-CM:347) are similar to that for HCC admissions. In effect, of the 1599 deaths registered in Portugal for cirrhosis, 73.2% (1172/1599) were male, and the age group with the most number of deaths was that over 65 years-old, having 40% of the total (638/1599). A higher rate of mortality was verified in persons between 65 and 74 years old with 39.5/105 (men 66.9/105 and women 17.4/105), compared to the national rate of 15.3/105[29].
In addition, the data provided by the National Registry of Deaths, which included mortality both for inpatients and outpatients, showed that deaths due to HCC (ICD 9:155.0 ICD 10:C220) almost doubled, from 149 in 1990 to 280 in 2004.
One of the most important indexes of health resource consumption, the average length of stay[30], was found to be higher in HCC patients when compared to the national average of 7.7 d; albeit, there was a tendency towards decrease from 17.5 d in 1993 to 9.3 d in 2005, P < 0.05, a trend that can be explained by the improvement of medical management for these groups of patients.
HCC is now the third cause of death by malignant tumors in males throughout the world[31]. Hepatocellular carcinoma is a disease with high mortality; one quarter of patients admitted to hospitals in Portugal for HCC died.
The overall mortality during hospitalization did not change over time, 26.7% in 2005 closely following the percentage of twelve years ago of 22.6% (1993). In addition, considering the figures of national mortality for HCC, the increase is more pronounced in the male sex, representing a 2.2 fold increase between 1990-2004, compared to females at 1.2 times. The same has been found by other authors[32]. The rate of mortality adjusted for age, 3.7/105 in men and 0.7/105 in women, being less than that generally found in other Mediterranean countries (5-12/105 in Spain, France, Italy)[3], suggests that the real number, in Portugal because of insufficient diagnosis, might be higher.
The reasons for the increase in these figures are not well understood, but several hypotheses can be put forth:[33] the increase in diagnostic yield, the increase of liver cirrhosis associated with hepatitis C infection resulting from intravenous drug addiction and blood transfusions in the sixties[34], the improvement of average survival in patients with liver cirrhosis due to better management[35].
A significant increase in the costs of hospital admissions for HCC was verified for all variables: over-all costs, cost per episode, and costs per day of hospital admission. The over-all costs increased 8.7 times since 1993 (€533 000), reaching the figure of €4 629 000 for the year 2005. In the twelve years studied, the average cost per day increased 5.7 times, from €105 to €597, and the average cost per episode increased 3.0 times, from €1828 to €5551.
It is important to emphasize that liver transplantation in HCC, indicated in around 7% of cases only, is the kind of therapy most effective in the long term[36,37], but carries a very high cost. The relative percentage of costs for transplantation in HCC in relation to the overall costs of hospital admission for HCC in Portugal has been increasing significantly, from 14.3% in 1993 for one transplant, to 32.5% (€1 505 669) in 2005 for 15 liver transplants. Put in another way, in 2005, 1.8% (15/834) of hospital admissions for HCC, i.e. related with liver transplant, were responsible for a cost of about €1.5 million, corresponding to one third of the over-all costs all hospital admissions for HCC in that same year.
These data suggest that patients with HCC must be strictly selected for liver transplant[38] because the cost of a liver transplant for HCC appears to exceed in effect the lower long-term survival rate when compared with other indications[39] deemed significant to a health system.
In conclusion, HCC, from the point of view of hospital admissions, promises to significantly impact the Portuguese Public Health System Hospitals, due to the steady increase in the number of hospital admissions, 2.9 times over the period 1993 to 2005. The mortality for HCC in hospitals has been steadily rising, affecting a quarter of hospital admissions; thus HCC is a disease that is consuming a growing share of resources. The over-all costs for HCC increased dramatically, 8.7 times in the 12 years studied, 5.7 times for the average length of hospital stay, and 3 times for the cost of each day. HCC is indicated for liver transplant in a small number of cases only, remains a therapeutic option with high relative costs for the health care system. So, liver transplant for HCC, albeit potentially curative in selective cases, must be strictly indicated.
S- Editor Liu Y L- Editor Alpini GD E- Editor Chin GJ
| 1. | Pisani P, Parkin DM, Ferlay J. Estimates of the worldwide mortality from eighteen major cancers in 1985. Implications for prevention and projections of future burden. Int J Cancer. 1993;55:891-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 380] [Cited by in RCA: 371] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 2. | The World Health Report 2003. World Health Organization, Switzerland. . |
| 3. | Deuffic S, Poynard T, Valleron AJ. Correlation between hepatitis C virus prevalence and hepatocellular carcinoma mortality in Europe. J Viral Hepat. 1999;6:411-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | La Vecchia C, Lucchini F, Franceschi S, Negri E, Levi F. Trends in mortality from primary liver cancer in Europe. Eur J Cancer. 2000;36:909-915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 75] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Kim WR, Brown RS, Terrault NA, El-Serag H. Burden of liver disease in the United States: summary of a workshop. Hepatology. 2002;36:227-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 425] [Cited by in RCA: 411] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 6. | El-Serag HB, Davila JA, Petersen NJ, McGlynn KA. The continuing increase in the incidence of hepatocellular carcinoma in the United States: an update. Ann Intern Med. 2003;139:817-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 714] [Cited by in RCA: 684] [Article Influence: 31.1] [Reference Citation Analysis (0)] |
| 7. | Taura N, Yatsuhashi H, Hamasaki K, Nakao K, Daikoku M, Ueki T, Yano K, Matsumoto T, Ishibashi H, Eguchi K. Increasing hepatitis C virus-associated hepatocellular carcinoma mortality and aging: Long term trends in Japan. Hepatol Res. 2006;34:130-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Chiaramonte M, Stroffolini T, Vian A, Stazi MA, Floreani A, Lorenzoni U, Lobello S, Farinati F, Naccarato R. Rate of incidence of hepatocellular carcinoma in patients with compensated viral cirrhosis. Cancer. 1999;85:2132-2137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 9. | Beasley RP, Hwang LY, Lin CC, Chien CS. Hepatocellular carcinoma and hepatitis B virus. A prospective study of 22 707 men in Taiwan. Lancet. 1981;2:1129-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1838] [Cited by in RCA: 1758] [Article Influence: 40.0] [Reference Citation Analysis (0)] |
| 10. | Donato F, Boffetta P, Puoti M. A meta-analysis of epidemiological studies on the combined effect of hepatitis B and C virus infections in causing hepatocellular carcinoma. Int J Cancer. 1998;75:347-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 11. | Fattovich G, Giustina G, Degos F, Tremolada F, Diodati G, Almasio P, Nevens F, Solinas A, Mura D, Brouwer JT. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology. 1997;112:463-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1013] [Cited by in RCA: 957] [Article Influence: 34.2] [Reference Citation Analysis (0)] |
| 12. | Perz JF, Armstrong GL, Farrington LA, Hutin YJ, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2006;45:529-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1764] [Cited by in RCA: 1844] [Article Influence: 97.1] [Reference Citation Analysis (0)] |
| 13. | Villa E, Baldini GM, Pasquinelli C, Melegari M, Cariani E, Di Chirico G, Manenti F. Risk factors for hepatocellular carcinoma in Italy. Male sex, hepatitis B virus, non-A non-B infection, and alcohol. Cancer. 1988;62:611-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 14. | Davila JA, Morgan RO, Shaib Y, McGlynn KA, El-Serag HB. Hepatitis C infection and the increasing incidence of hepatocellular carcinoma: a population-based study. Gastroenterology. 2004;127:1372-1380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 354] [Cited by in RCA: 338] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 15. | Befeler AS, Hayashi PH, Di Bisceglie AM. Liver transplantation for hepatocellular carcinoma. Gastroenterology. 2005;128:1752-1764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 95] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | Rosina F, Alaria P, Castelli S, Dirindin N, Rocca G, Actis GC, Borelli R, Ciancio AL, De Bernardi W, Fornasiero S. Effect of patient characteristics on hospital costs for cirrhosis: implications for the disease-related group (DRG) reimbursement system. Ital J Gastroenterol. 1996;28:401-405. [PubMed] |
| 17. | Muñoz E, Greenberg R, Faust G, Goldstein JD, Bank S, Wise L. Gastroenterology, diagnosis-related groups, and age. J Clin Gastroenterol. 1989;11:421-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Vestberg K, Thulstrup AM, Sørensen HT, Ottesen P, Sabroe S, Vilstrup H. Data quality of administratively collected hospital discharge data for liver cirrhosis epidemiology. J Med Syst. 1997;21:11-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 74] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Okuda K, Fujimoto I, Hanai A, Urano Y. Changing incidence of hepatocellular carcinoma in Japan. Cancer Res. 1987;47:4967-4972. [PubMed] |
| 20. | El-Serag HB, Mason AC. Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med. 1999;340:745-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2221] [Cited by in RCA: 2140] [Article Influence: 82.3] [Reference Citation Analysis (0)] |
| 21. | Davis GL, Albright JE, Cook SF, Rosenberg DM. Projecting future complications of chronic hepatitis C in the United States. Liver Transpl. 2003;9:331-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 442] [Cited by in RCA: 404] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 22. | Taylor-Robinson SD, Foster GR, Arora S, Hargreaves S, Thomas HC. Increase in primary liver cancer in the UK, 1979-94. Lancet. 1997;350:1142-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 383] [Cited by in RCA: 370] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 23. | Afessa B, Kubilis PS. Upper gastrointestinal bleeding in patients with hepatic cirrhosis: clinical course and mortality prediction. Am J Gastroenterol. 2000;95:484-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 24. | Kulkarni K, Barcak E, El-Serag H, Goodgame R. The impact of immigration on the increasing incidence of hepatocellular carcinoma in the United States. Aliment Pharmacol Ther. 2004;20:445-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Bosch FX, Ribes J. Epidemiology of liver cancer in Europe. Can J Gastroenterol. 2000;14:621-630. [PubMed] |
| 26. | Stroffolini T, Andreone P, Andriulli A, Ascione A, Craxi A, Chiaramonte M, Galante D, Manghisi OG, Mazzanti R, Medaglia C. Characteristics of hepatocellular carcinoma in Italy. J Hepatol. 1998;29:944-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 114] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 27. | De Vos Irvine H, Goldberg D, Hole DJ, McMenamin J. Trends in primary liver cancer. Lancet. 1998;351:215-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Makimoto K, Higuchi S. Alcohol consumption as a major risk factor for the rise in liver cancer mortality rates in Japanese men. Int J Epidemiol. 1999;28:30-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Health Ministry of Portugal. Risk of dying in Portugal 2003. Available from: http://www.dgs.pt/upload/membro.id/ficheiros/i008249.pdf on 12 February 2007. |
| 30. | Munoz E, Greenberg R, Chalfin D, Bank S, Mulloy K, Wise L. Hospital costs, resource characteristics, and the dynamics of death for hospitalized gastroenterology patients. Am J Gastroenterol. 1988;83:957-962. [PubMed] |
| 31. | Parkin M, Bray F, Ferlay J, Pisani P. Global Cancer Statistics 2002. CA Cancer J Clin. 2005;55:74-108. [RCA] [DOI] [Full Text] [Cited by in Crossref: 13286] [Cited by in RCA: 13558] [Article Influence: 677.9] [Reference Citation Analysis (1)] |
| 32. | Benhamiche AM, Faivre C, Minello A, Clinard F, Mitry E, Hillon P, Faivre J. Time trends and age-period-cohort effects on the incidence of primary liver cancer in a well-defined French population: 1976-1995. J Hepatol. 1998;29:802-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 33. | Tanaka Y, Hanada K, Mizokami M, Yeo AE, Shih JW, Gojobori T, Alter HJ. A comparison of the molecular clock of hepatitis C virus in the United States and Japan predicts that hepatocellular carcinoma incidence in the United States will increase over the next two decades. Proc Natl Acad Sci USA. 2002;99:15584-15589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 229] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 34. | Haydon GH, Jarvis LM, Simmonds P, Harrison DJ, Garden OJ, Hayes PC. Association between chronic hepatitis C infection and hepatocellular carcinoma in a Scottish population. Gut. 1997;40:128-132. [PubMed] |
| 35. | Trinchet JC, Beaugrand M. Increased incidence of hepatocellular carcinoma in western countries: the reasons and the consequences. Gastroenterol Clin Biol. 1999;23:1286-1288. [PubMed] |
| 36. | Ryder SD. Guidelines for the diagnosis and treatment of hepatocellular carcinoma (HCC) in adults. Gut. 2003;52 Suppl 3:iii1-iii8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 220] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 37. | Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, Burroughs AK, Christensen E, Pagliaro L, Colombo M, Rodés J. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol. 2001;35:421-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3252] [Cited by in RCA: 3244] [Article Influence: 135.2] [Reference Citation Analysis (0)] |
| 38. | Freeman RB. Transplantation for hepatocellular carcinoma: The Milan criteria and beyond. Liver Transpl. 2006;12:S8-S13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 39. | Llovet JM, Beaugrand M. Hepatocellular carcinoma: present status and future prospects. J Hepatol. 2003;38 Suppl 1:S136-S149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 172] [Article Influence: 7.8] [Reference Citation Analysis (0)] |