Published online Jan 14, 2006. doi: 10.3748/wjg.v12.i2.331
Revised: June 28, 2005
Accepted: July 13, 2005
Published online: January 14, 2006
AIM: To evaluate the utility of local tumor therapy combined with percutaneous transhepatic biliary drainage (PTBD) for malignant obstructive biliary disease.
METHODS: A total of 233 patients with malignant biliary obstruction were treated in our hospital with PTBD by placement of metallic stents and/or plastic tubes. After PTBD, 49 patients accepted brachytherapy or extra-radiation therapy or arterial infusion chemotherapy. The patients were followed up with clinical and radiographic evaluation. The survival and stent patency rate were calculated by Kaplan-Meier survival analysis.
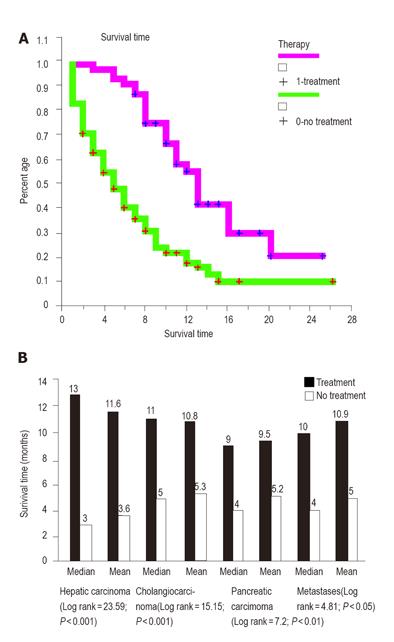
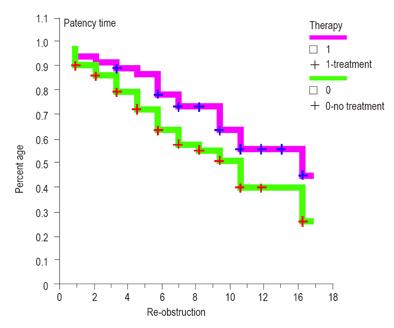
RESULTS: Twenty-two patients underwent chemotherapy (11 cases of hepatic carcinoma, 7 cases of pancreatic carcinoma, 4 cases of metastatic lymphadenopathy), and 14 patients received radiotherapy (10 cases of cholangiocarcinoma, 4 cases of pancreatic carcinoma), and 13 patients accepted brachytherapy (7 cases of cholangiocarcinoma, 3 cases of pancreatic carcinoma, 4 cases of metastatic lymphadenopathy). The survival rate of the local tumor treatment group at 1, 3, 6, and 12 months was 97.96%, 95.92%, 89.80%, and 32.59% respectively, longer than that of the non treatment group. The patency rate at 1, 3, 6, and 12 months was 97.96%, 93.86%, 80.93%, and 56.52% respectively. The difference of patency rate was not significant between treatment group and non treatment group.
CONCLUSION: Our results suggest that local tumor therapy could prolong the survival time of patients with malignant biliary obstruction, and may improve stent patency.
- Citation: Qian XJ, Zhai RY, Dai DK, Yu P, Gao L. Treatment of malignant biliary obstruction by combined percutaneous transhepatic biliary drainage with local tumor treatment. World J Gastroenterol 2006; 12(2): 331-335
- URL: https://www.wjgnet.com/1007-9327/full/v12/i2/331.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i2.331
Percutaneous transhepatic biliary drainage (PTBD) is a well-established interventional radiological procedure used in patients with malignant obstructive jaundice, especially in inoperable patients [1-4]. We treated 233 cases with PTBD from January 1995 to October 2002, 49 of these patients were further treated for local tumors after PTBD. The therapeutic results are reported here.
From January 1995 to October 2002, 233 consecutive patients (92 females and 141 males, age ranged from 29 to 91 years, mean age of 63.6 years) with malignant biliary obstruction were treated in our hospital with transhepatic placement of metallic stents and/or plastic tubes. The diagnosis and poor prognosis of the patients were established by various imaging methods (US, CT, MRI) and biliary brush cytology or puncture biopsy. Forty-four of these individuals were diagnosed with pancreatic carcinoma, 89 with cholangiocarcinoma, 54 with metastases originating from a variety of primary sites and the remaining 46 with hepatic carcinoma. The obstructing lesion predominantly involved both the right and left main hepatic ducts in 106 patients and the common hepatic and/or proximal common bile duct in 127 patients.
After routine percutaneous transhepatic cholangiography, the obstructing lesions were traversed using Terumo guide-wire techniques. If the guide wire could not pass the stricture, the external catheter was retained. Once the guide wire crossed the lesion and entered the bowel, we could deploy the stent or an internal-external catheter. When a stent was needed, a catheter with a side-arm sheath was employed to inject contrast material over the wire for accurate delineation of the upper and lower margins of the obstructing lesion. After the diagnostic catheter was removed, an 8-10F sheath with a side arm and a homeostasis valve was placed over the wire into the bile duct to allow retrieval of the stent in the event of malfunction of the stent delivery system. The side arm could provide a convenient portal for the injection of contrast material into opacity in the biliary ducts, which could facilitate stent positioning. Eight-millimeter balloons were used in most cases, but 10-mm balloons were required occasionally. Dilation before stent placement as a routine procedure was performed in most of the patients.
Transcatheter arterial chemoembolization (TACE) of all hepatic arteries, celiac and superior mesenteric arteries and their branches should be adequately opacified and all feeding arteries should be carefully identified. We performed TACE initially with infusion of 1000 mg 5-FU, 40~80 mg cisplatin or 200~400 mg carboplatin, 10~20 mg mitomycin or 20~60 mg pharmorubicin, sometimes added 5~15 mL lipiodol with 20~60 mg pirarubicin. We followed up the patients for one or two months with computer tomography, and made TACE 1-3 times.
External irradiation: Cobalt-60 source was used with a total integral dose of 6000cGy at the target length of 1cm, 200cGy per day for 30 d.
Intraluminal brachytherapy: After deployed the stent, we detained a coaxial guider located at the stenosis of endoprothesis to undergo after-loading treatment. The intraluminal brachytherapy using the high dose rate iridium-192 (192Ir) sources was performed to deliver an integral dose of 3000cGy, 500cGy each time, two times a day for 3 d, and standard points were established at 1.0 cm.
Follow-up of each patient was based on outpatient examinations and telephone interviews. The clinical symptoms, phantom change and laboratory examination were recorded. Survival was determined from the time of PTBD. The patent time was defined as the interval between PTBD and obstructive jaundice recurrence. If occlusion did not occur during a patient’s life time, the patent period was considered equal to the survival period. Jaundice recurrence was defined as the symptom of jaundice recurred after it subsided and met one of the followings: cholangiography, CT or US demonstrating redilation of bile duct and combined serum bilirubin concentration/total serum bilirubin concentration ≥ 35%, or serum bilirubin increased after its obvious drop (> 100μmol/L) or after it was lower than half of its original level. The survival and stent patency were calculated by Kaplan-Meier survival analysis. Analysis of data was performed with SPSS/PC version 8.0.
PTBD was successfully performed in all the patients. Stent placement was conducted in 136 cases. Of these 136 patients, 100 were treated with only 1 stent, 20 cases with 2 stents for bilateral drainage and 16 with 2 stents for long strictures. The other 97 patients received plastic catheters. The serum level of total bilirubin reduced from 349.2+/-155.6 μmol/l to 178.9+/-141.2 μmol/l after PTBD (t = 17.90, P = 0.000).
Forty-nine patients (16 females and 33 males, age ranged from 38 to 83 years, a mean age of 64.4 years) accepted local tumor treatment. Twenty-two patients underwent chemotherapy (11 cases of hepatic carcinoma, 7 cases of pancreatic carcinoma, 4 cases of metastasis), one patient died within 1 month because of re-obstruction in bile duct and poor conditions, others received two or three times of treatment for chemical infusion. Fourteen patients received external beam radiation therapy (10 cases of cholangiocarcinoma, 4 cases of pancreatic carcinoma), and 13 patients accepted brachytherapy (7 cases of cholangiocarcinoma, 3 cases of pancreatic carcinoma, 3 cases of metastatic lymphadenopathy). Obstruction occurred at the hilum in 20 cases while 14 cases received multi-drainage, and at the lower common bile duct in 29 cases. Among the 20 patients with obstruction at the hilum, 8 cases received chemotherapy, 6 external beam radiotherapy, and 6 intraluminar brachytherapy. Among the 29 patients with obstruction at the lower common bile duct, 14 cases received chemotherapy, 8 external beam radiotherapy, and 7 intraluminar brachytherapy.
Total serum bilirubin in those who received local tumor treatment reduced from 324.04+/-166.21 μmol/l (mean+/-SD) to 87.38+/-70.96 μmol/l (t = 11.54, P < 0.001). Total serum bilirubin reduced more than 50% in 42 patients and more than 25% in 7 patients. ALT was decreased from 129.3+/-112.8 IU/L to 54.0+/-48.5 IU/L (t = 4.01, P < 0.001), GGT was decreased from 576.4+/-396.9 IU/L to 238.8+/-235.4 IU/L (t = 5.58, P < 0.001) and ALP was decreased from 687.9+/-685.1 IU/L to 291.5+/-247.1 IU/L (t = 3.47, P = 0.001).
Patients with obstruction at the lower common bile duct had more chances to receive local tumor therapy. Stent deployment made it possible for patients to receive further treatment (Table 1).
| Group | n | Treatment | Chi-square | P-value |
| 184 | 49 | |||
| Hepatic carcinoma | 35 | 11 | ||
| Cholangiocarcinoma | 72 | 17 | ||
| Pancreatic carcinoma | 30 | 14 | ||
| Metastases | 47 | 7 | ||
| Hilar | 107 | 20 | 4.69 | 0.03 |
| CBD | 77 | 29 | ||
| M | 108 | 33 | 1.212 | 0.271 |
| F | 76 | 16 | ||
| Younger than 70 | 132 | 30 | 2.019 | 0.155 |
| Over 70 | 52 | 19 | ||
| Stent | 100 | 36 | 5.822 | 0.016 |
| Catheter | 84 | 13 | ||
| No | 122 | 43 | 8.615 | 0.003 |
| Have | 62 | 6 |
No severe complication occurred after the procedures. One patient with stent placement died within 1 month because of bile duct re-obstruction and poor conditions. Five patients were still alive during follow-up, and the survival time was 10.5 months (median), and the 1-, 3-, 6- and 12- month survival rate was 97.96%, 95.92%, 89.80%, 32.59%, respectively. Twelve patients who received chemotherapy had re-obstruction during follow-up. Eight patients subsequently developed occluded stents that were treated with one or more additional interventions such as placement of additional stents (n = 2) or placement of temporal external drainage (n = 6). Four patients who received catheter drainage had replacement of the plastic catheter. One patient appeared to have distal tumor overgrowth and one exhibited both proximal overgrowth and intraluminal filling defects and three patients developed sludge and debris within the stent. Seven patients who developed an intraluminal filling defect in stent or catheter did not have any cytological or histological evidence. Two patients who received intraluminal brachytherapy and 2 who received external irradiation had re-obstruction during follow-up, which was eliminated by balloon dilation. The patent time was 14 mo (median). The patency rate at 1, 3, 6, and 12 mo was 97.96%, 93.86%, 80.93%, and 56.52%, respectively. While the 1-, 3-, 6- and 12- mo survival rate of non-therapy group was 84.24%, 56.97%, 26.40%, and 5.52% respectively, and the patency rate at 1, 3, 6, and 12 months was 94.15%, 84.89%, 66.29%, and 35.73% respectively. The median survival time was significantly longer in the local treatment group than in the no-adjuvant therapy group respectively (Log rank = 46.34, P < 0.001) (Figure 1). Though the patency rate of treatment group was higher than that of non-therapy group, there was no significant difference between these two groups (Log rank = 2.38, P = 0.123, Figure 2)
Surgical therapy of malignant obstructive jaundice includes a curative resection or a palliative operation of the tumor. Unfortunately, the surgical cure rate of pancreatic, bile duct and gall bladder carcinoma, and hepatic carcinoma is lower than 5%[5,6]. Since the resectability of pancreatic cancer remains below 30%[7], palliative treatment is recommended for patients with unresectable tumor.
Interventional radiologists play an important role in the management of patients with malignant biliary obstruction. Biliary drainage is usually used as the initial treatment because of overt cholangitis. All procedures were performed using fluoroscopic guidance alone in our study. Early and effective biliary drainage might be necessary in this group of patients with limited hepatic function to improve the prognosis[8]. PTBD for inoperable malignant obstructive jaundice is a widely used palliative procedure [1-3].
Yan[9] pointed out that bile drainage as a palliative therapy for malignant obstructive jaundice could not prolong the survival time, but can improve life quality. Successful biliary drainage after biliary decompression is associated with improvement in quality of life[10]. However, PTBD could provide access to the intrahepatic and extrahepatic bile ducts[11-13].
Since PTBD alleviates icterus and improves liver reserve function, patients with tumor could have more chances to receive chemotherapy or radiotherapy or photodynamic therapy [14] or radiofrequency ablation[15]. But how to choose system chemotherapy and artery infusion chemotherapy may be a question. Xia and Wang[16] reported that intra-artery treatment is more effective than system chemotherapy. Also radiotherapy can improve the survival[17]. Huang et al [18] demonstrated that radiotherapy is an effective adjuvant strategy in those who have a limited response to TACE or have a poor liver reserve function.
Occlusion of the stent by overgrowth of proximal or distal ends can be easily demonstrated and identified. In some cases, the defects consist of desquamated cells, mucus, and sludge. It has been speculated that these defects may be caused by tumor ingrowth through the meshes of the stent[19]. Drug infusion via supplying artery and embolization therapy have been used in clinical practice as an effective way of suppressing the growth of malignant tumors[20-23]. Further tumor therapy may improve the patency of stent and survival[24-26].
TACE therapy could increase common bile duct obstruction due to tumor thrombi[27]. External beam radiation therapy may be beneficial in some patients with unresectable icteric-type HCC[28,29]. When combined with other conventional therapies (such as TACE), radiation therapy may play an important role in the treatment of HCC[30,31].
In conclusion, PTBD is an effective palliative procedure for improving malignant obstructive jaundice.
S- Editor Wang XL and Guo SY L- Editor Elsevier HK E- Editor Wu M
| 1. | Nakamura T, Kitagawa M, Takehira Y, Yamada M, Kawasaki T, Nakamura H. Polyurethane-covered Wallstents to recanalize Wallstents obstructed by tumor ingrowth from malignant common bile duct obstruction. Cardiovasc Intervent Radiol. 2000;23:161-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Cheng YF, Lee TY, Sheen-Chen SM, Huang TL, Chen TY. Treatment of complicated hepatolithiasis with intrahepatic biliary stricture by ductal dilatation and stenting: long-term results. World J Surg. 2000;24:712-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Zhai R, Qian X, Dai D, Yu P. Malignant biliary obstruction: treatment with interventional radiology. Chin Med J (Engl). 2003;116:888-892. [PubMed] |
| 4. | Schoder M, Rossi P, Uflacker R, Bezzi M, Stadler A, Funovics MA, Cejna M, Lammer J. Malignant biliary obstruction: treatment with ePTFE-FEP- covered endoprostheses initial technical and clinical experiences in a multicenter trial. Radiology. 2002;225:35-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 73] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Parker SL, Tong T, Bolden S, Wingo PA. Cancer statistics, 1997. CA Cancer J Clin. 1997;47:5-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1494] [Cited by in RCA: 1410] [Article Influence: 50.4] [Reference Citation Analysis (0)] |
| 6. | Lau W, Leung K, Leung TW, Liew CT, Chan MS, Yu SC, Li AK. A logical approach to hepatocellular carcinoma presenting with jaundice. Ann Surg. 1997;225:281-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Gudjonsson B. Pancreatic cancer. The need for critical reassessment. J Clin Gastroenterol. 1996;23:2-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Lee JW, Han JK, Kim TK, Choi BI, Park SH, Ko YH, Yoon CJ, Yeon KM. Obstructive jaundice in hepatocellular carcinoma: response after percutaneous transhepatic biliary drainage and prognostic factors. Cardiovasc Intervent Radiol. 2002;25:176-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Yan LN, Complex therapy of malignant obstruction jaundice. Zhongguo Shiyong Waike Zazhi. 2001;21:473. |
| 10. | Abraham NS, Barkun JS, Barkun AN. Palliation of malignant biliary obstruction: a prospective trial examining impact on quality of life. Gastrointest Endosc. 2002;56:835-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 124] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Jung GS, Huh JD, Lee SU, Han BH, Chang HK, Cho YD. Bile duct: analysis of percutaneous transluminal forceps biopsy in 130 patients suspected of having malignant biliary obstruction. Radiology. 2002;224:725-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 39] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Rossi M, Cantisani V, Salvatori FM, Rebonato A, Greco L, Giglio L, Guido G, Pagliara E, David V. Histologic assessment of biliary obstruction with different percutaneous endoluminal techniques. BMC Med Imaging. 2004;4:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Savader SJ, Prescott CA, Lund GB, Osterman FA. Intraductal biliary biopsy: comparison of three techniques. J Vasc Interv Radiol. 1996;7:743-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Suzuki S, Inaba K, Yokoi Y, Ohata K, Ota S, Azuma M, Tanaka T, Konno H, Baba S, Hirano T. Photodynamic therapy for malignant biliary obstruction: a case series. Endoscopy. 2004;36:83-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Zhang FJ, Wu PH, Gu YK, Zhao M, Fan WJ, Xiao XS. [Clinical value of brachytherapy of malignant biliary obstruction after implanting expandable metallic biliary endoprothesis (EMBE)]. Ai Zheng. 2004;23:1567-1571. [PubMed] |
| 16. | Xia JD, Wang DM. Treatment of Malignate Biliary Obstruction by Double Interventional Radiology: 18 cases experience. Zhongguo Shiyong Neike Zazhi. 2001;21:113-114. |
| 17. | Kim GE, Shin HS, Seong JS, Loh JJ, Suh CO, Lee JT, Roh JK, Kim BS, Kim WH, Kim MW. The role of radiation treatment in management of extrahepatic biliary tract metastasis from gastric carcinoma. Int J Radiat Oncol Biol Phys. 1994;28:711-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Huang JF, Wang LY, Lin ZY, Chen SC, Hsieh MY, Chuang WL, Yu MY, Lu SN, Wang JH, Yeung KW. Incidence and clinical outcome of icteric type hepatocellular carcinoma. J Gastroenterol Hepatol. 2002;17:190-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 64] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Isayama H, Komatsu Y, Tsujino T, Yoshida H, Tada M, Shiratori Y, Kawabe T, Omata M. Polyurethane-covered metal stent for management of distal malignant biliary obstruction. Gastrointest Endosc. 2002;55:366-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 123] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 20. | Yoshida H, Onda M, Tajiri T, Akimaru K, Uchida E, Arima Y, Mamada Y, Taniai N, Yamamoto K, Kaneko M. New techniques: splenic artery embolization followed by intraarterial infusion chemotherapy for the treatment of pancreatic cancer. Hepatogastroenterology. 1999;46:2024-2027. [PubMed] |
| 21. | Yoshida H, Onda M, Tajiri T, Uchida E, Arima Y, Mamada Y, Yamamoto K, Kaneko M, Terada Y, Kumazaki T. Experience with intraarterial infusion of styrene maleic acid neocarzinostatin (SMANCS)-lipiodol in pancreatic cancer. Hepatogastroenterology. 1999;46:2612-2615. [PubMed] |
| 22. | Naka T, Ashida K, Takahashi S, Kaneko T, Mizusawa K, Kaibara N. Effective TAE therapy using Lipiodol with epirubicin for liver metastases of nonfunctioning islet cell carcinoma of the pancreas. J Hepatobiliary Pancreat Surg. 1998;5:108-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Kröger JC, Bergmeister H, Hoffmeyer A, Ceijna M, Karle P, Saller R, Schwendenwein I, von Rombs K, Liebe S, Günzburg WH. Intraarterial instillation of microencapsulated cells in the pancreatic arteries in pig. Ann N Y Acad Sci. 1999;880:374-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Miura Y, Endo I, Togo S, Sekido H, Misuta K, Fujii Y, Kubota T, Tanaka K, Nagahori K, Shimada H. Adjuvant therapies using biliary stenting for malignant biliary obstruction. J Hepatobiliary Pancreat Surg. 2001;8:113-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Eschelman DJ, Shapiro MJ, Bonn J, Sullivan KL, Alden ME, Hovsepian DM, Gardiner GA. Malignant biliary duct obstruction: long-term experience with Gianturco stents and combined-modality radiation therapy. Radiology. 1996;200:717-724. [PubMed] |
| 26. | Kuvshinoff BW, Armstrong JG, Fong Y, Schupak K, Getradjman G, Heffernan N, Blumgart LH. Palliation of irresectable hilar cholangiocarcinoma with biliary drainage and radiotherapy. Br J Surg. 1995;82:1522-1525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 78] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | Qin LX, Tang ZY. Hepatocellular carcinoma with obstructive jaundice: diagnosis, treatment and prognosis. World J Gastroenterol. 2003;9:385-391. [PubMed] |
| 28. | Chen SC, Lian SL, Chang WY. The effect of external radiotherapy in treatment of portal vein invasion in hepatocellular carcinoma. Cancer Chemother Pharmacol. 1994;33 Suppl:S124-S127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Liu MT, Li SH, Chu TC, Hsieh CY, Wang AY, Chang TH, Pi CP, Huang CC, Lin JP. Three-dimensional conformal radiation therapy for unresectable hepatocellular carcinoma patients who had failed with or were unsuited for transcatheter arterial chemoembolization. Jpn J Clin Oncol. 2004;34:532-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 71] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 30. | Wu DH, Chen LH. [Efficacy of 3-dimensional conformal hypofractionated single high-dose radiotherapy combined with transcatheter arterial chemoembolization for portal vein tumor thrombus in patients with hepatocellular carcinoma]. Ai Zheng. 2004;23:825-828. [PubMed] |
| 31. | Guo WJ, Yu EX, Liu LM, Li J, Chen Z, Lin JH, Meng ZQ, Feng Y. Comparison between chemoembolization combined with radiotherapy and chemoembolization alone for large hepatocellular carcinoma. World J Gastroenterol. 2003;9:1697-1701. [PubMed] |