Published online Nov 7, 2005. doi: 10.3748/wjg.v11.i41.6557
Revised: April 27, 2005
Accepted: April 30, 2005
Published online: November 7, 2005
Internal herniation of the small bowel is a relatively rare cause of intestinal obstruction. Left paraduodenal hernia resulting from abnormal rotation of the midgut during embryonic development is the most common form of congenital internal hernia. We report our experience in the diagnosis and management of a young male with left paraduodenal hernia presenting as recurrent intestinal obstruction. Correct preoperative diagnosis of left paraduodenal hernia had been difficult due to non-specific clinical presentations, but the advent of modern imaging technology makes early and correct diagnosis possible. Due to the risk of obstruction and strangulation, surgical treatment is indicated; however, timely intervention increases the likelihood of a favorable outcome.
- Citation: Huang YM, Chou ASB, Wu YK, Wu CC, Lee MC, Chen HT, Chang YJ. Left paraduodenal hernia presenting as recurrent small bowel obstruction. World J Gastroenterol 2005; 11(41): 6557-6559
- URL: https://www.wjgnet.com/1007-9327/full/v11/i41/6557.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i41.6557
congenital internal hernias, paraduodenal hernias are the most common and account for 25%-53% of all cases[2]. Paraduodenal hernias result from abnormal rotation of the midgut during embryonic development and can be divided into two subtypes, left and right paraduodenal hernias, according to their distinct pathogenesis and the resultant anatomical derangement. Correct preoperative diagnosis of paraduodenal hernia was once difficult, because of its non-specific presentations; however, with the advent of modern imaging technology, more information can be gained regarding the anatomical characteristics of the underlying lesion and allow for better treatment planning. We present our experience in the diagnosis and management of a patient with left paraduodenal hernia presenting as recurrent intestinal obstruction, as well as a brief review of the literature.
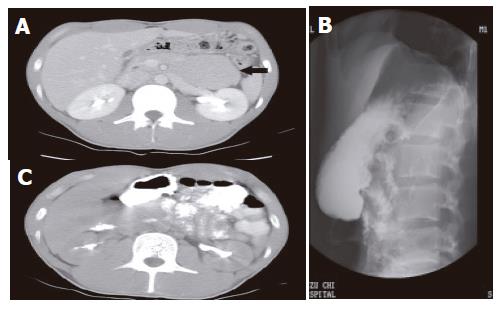
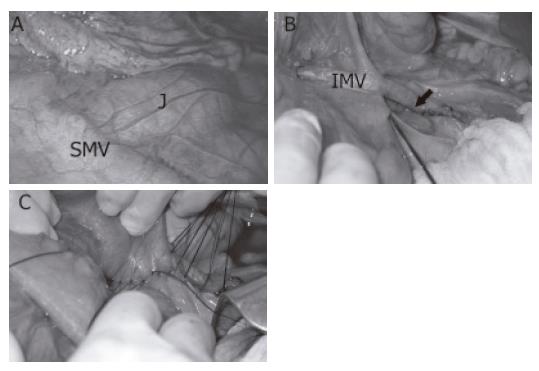
The patient was a slim 24-year-old male who visited our emergency room because of intermittent epigastric abdominal pain associated with bilious vomitus during the previous few hours. He had no history of previous abdominal surgery, but had a similar episode with pain and vomiting about 6 mo before. He had lost about 10 kg during that period. Physical examination revealed a non-tender, mildly distended abdomen with hyperactive bowel sounds. The only remarkable finding on plain abdominal film was loops of a dilated small bowel. Initial abdominal computed tomography (CT) revealed a mass lesion of soft tissue density located between the stomach, the pancreas, and the transverse colon (Figure 1A). For better elucidation of the character of the mass lesion, we performed an upper gastrointestinal series with small intestinal follow-through, which revealed loops of jejunum clumping over the left upper quadrant of the abdomen (Figure 1B). The mass lesion proved to be a cluster of jejunum on follow-up CT (Figure 1C). The patient underwent surgery with a tentative diagnosis of left paraduodenal hernia with small bowel obstruction. Exploratory laparoscopy and laparotomy revealed that the jejunum did not emerge from the usual position at the base of transverse mesocolon; instead, only loops of the small bowel were visualized behind a thin layer of peritoneum (Figure 2A). Further exploration revealed that the jejunum exited from an aperture of about 15 cm caudal to the usual location of Treitz’s ligament. The initial 10 cm of intraperitoneal jejunum ran parallel and was adherent to both the inferior mesenteric artery (IMA) and the inferior mesenteric vein (IMV), which constitute the anterior rim of the orifice (Figure 2B). A 25 cm long segment of jejunum had herniated through the orifice into the space behind the descending mesocolon. We manually reduced the herniated bowel loops after opening the anterior wall of the hernial sac by dividing the adhesion between the jejunum and the IMV. We then closed the orifice of the hernial sac around the jejunum with interrupted 3-0 silk sutures (Figure 2C). The patient tolerated the procedure well and recovery was uneventful postoperatively. Follow-up upper gastrointestinal series revealed the smooth passage of contrast medium without evidence of abnormal aggregation of the small bowel.
Left paraduodenal hernia is about three times more frequent than its right counterpart, and is reported to occur three times more often in men[3]. As mentioned previously, left paraduodenal hernia usually results from abnormal rotation of the midgut. In the 5th wk of embryonic development, the rapidly elongating midgut herniates into the umbilical cord. Later, the herniated midgut undergoes a counter clockwise rotation of 90° around the superior mesenteric artery (SMA), leaving the prearterial limb on the left side. The herniated intestinal loop, first the prearterial then the postarterial limb, returns to the abdominal cavity by the 10th week. During this process, the intestinal loop undergoes another 180° countercloc kwise rotation. In the end, the prearterial limb lies left to the SMA and the postarterial limb lies superior and right to the SMA[4]. Under normal circumstances, fusion of the mesocolon with the peritoneum of the body wall follows this process. Failure of the fusion to take place in time leaves a potential space (the fossa of Landzert) behind the mesocolon. A leftparaduodenal hernia results from invagination of the small intestine into this unsupported area through an opening bound anteriorly by the IMV and is established as the descending colon that seeks its normal attachment[2].
Although the left paraduodenal hernia is congenital, most patients are recognized between the 4th and 6th decades of life, and the mean age at the time of diagnosis is 38.5 years[3]. The most common presentations are those associated with small bowel obstruction and are nonspecific[5], ranging in severity from recurrent vague abdominal pain, nausea, and vomiting in partial, reversible obstruction to acute abdomen in cases of incarceration and strangulation.
Physical examination is usually unrevealing except for such nonspecific findings as abdominal tenderness, distension, and the occasional presence of a mass. Correct preoperative diagnosis has been difficult in the past, due to these ambiguous presentations; therefore, it is mandatory to maintain a high index of suspicion in patients with pertinent unexplained complaints. Under emergent settings, diagnosis is only possible at the time of surgery. In the absence of an abdominal emergency, however, a variety of diagnostic tools is available to help establish the correct diagnosis before surgery. Because of the ambiguous clinical presentation of this disease, a CT scan may be the initial tool of investigation. A characteristic finding is a cluster of small bowel loops between the stomach and pancreas[6,7]. In case that the trapped loops are collapsed and oral contrast is not used, the hernia contents may be mistaken for a soft tissue mass. A high index of suspicion is again required to avoid inadvertent invasive diagnostic procedures such as CT-guided biopsy, which may be disastrous under such circumstances. An upper gastrointestinal series with small bowel follow-through demonstrates contrast-filled loops of small bowel clustering over the left upper aspect of the abdomen, as is seen in our patient. Abdominal ultrasonography might also aid in the diagnosis of paraduodenal hernia. Suggestive findings include a cluster of bowel loops or a well-defined mass. Peristalsis of the bowel loops can be appreciated and made more obvious with the ingestion of water[8].
In earlier reports, the diagnosis and treatment of left paraduodenal hernia tended to be delayed and the result of treatment seemed to be less satisfactory[5]. With the diagnostic tools available today, correct diagnoses are possible even in the absence of acute symptoms, and treatment can commence promptly. Once diagnosed, left paraduodenal hernia should be surgically repaired because 50% of them cause intestinal obstruction[5,9]. The procedure consists of a manual reduction of the hernia contents followed by repair of the defect. If the herniated intestine is difficult to reduce because of its bulky size or adhesions within the sac, an incision can be made in the avascular portion of the hernial sac to the right of the inferior mesenteric vessels to enlarge the opening[2]. During this procedure, it is important to consider the relationship of the inferior mesenteric vessels to the sac opening and to take care to avoid injury to these structures. Although Bartlett indicated that these vessels can be divided without compromising blood supply to the colon[1], they should be preserved whenever possible. Intestinal resection is necessary in cases of strangulation and gangrene. In addition to the conventional “open” approach, successful laparoscopic repair of left paraduodenal hernia has been reported by Uematsu et al[10].
In conclusion, although relatively uncommon, left paraduodenal hernia should be included in the differential diagnosis of small bowel obstruction in patients who are relatively young, who have repetitive attacks, and who lack any history of previous abdominal surgery. The combination of a high index of suspicion, familiarity with this disease entity, and modern imaging technology make preoperative diagnosis easier today. Timely surgical intervention effectively relieves the patient’s complaints and prevents further complications.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Bartlett MK, Wang C, Williams WH. The surgical management of paraduodenal hernia. Ann Surg. 1968;168:249-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 62] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Brigham RA, Fallon WF, Saunders JR, Harmon JW, d'Avis JC. Paraduodenal hernia: diagnosis and surgical management. Surgery. 1984;96:498-502. [PubMed] |
| 4. | Berardi RS. Paraduodenal hernias. Surg Gynecol Obstet. 1981;152:99-110. [PubMed] |
| 5. | Newsom BD, Kukora JS. Congenital and acquired internal hernias: unusual causes of small bowel obstruction. Am J Surg. 1986;152:279-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 155] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Olazabal A, Guasch I, Casas D. Case report: CT diagnosis of nonobstructive left paraduodenal hernia. Clin Radiol. 1992;46:288-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Warshauer DM, Mauro MA. CT diagnosis of paraduodenal hernia. Gastrointest Radiol. 1992;17:13-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 38] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Wachsberg RH, Helinek TG, Merton DA. Internal abdominal hernia: diagnosis with ultrasonography. Can Assoc Radiol J. 1994;45:223-224. [PubMed] |
| 9. | Isabel L, Birrell S, Patkin M. Paraduodenal hernia. Aust N Z J Surg. 1995;65:64-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Uematsu T, Kitamura H, Iwase M, Yamashita K, Ogura H, Nakamuka T, Oguri H. Laparoscopic repair of a paraduodenal hernia. Surg Endosc. 1998;12:50-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 2.1] [Reference Citation Analysis (0)] |