Published online Nov 7, 2005. doi: 10.3748/wjg.v11.i41.6466
Revised: April 8, 2005
Accepted: April 11, 2005
Published online: November 7, 2005
AIM: To investigate the effect of six bile salts: glycocholate (GC), glycochenodeoxycholate (GCDC), glycodeoxycholate (GDC), taurocholate (TC), taurochenodeoxycholate (TCDC), taurodeoxycholate (TDC), and their mixture on cultured human normal esophageal mucosal epithelial cells.
METHODS: Human normal esophageal mucosal epithelial cells were cultured with serum-free keratinocyte medium. 3-[4,5-Dimethylthiaolyl]-2,5-diphenyl-tetrazolium bromide assay was applied to the detection of cell proliferation. Apoptotic morphology was observed by phase-contrast video microscopy and terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling (TUNEL) assay. Sub-G1 DNA fragmentations and early apoptotic cells were assayed by flow cytometry (FCM) with propidium iodide (PI) staining and annexin V-FITC conjugated with PI staining. Apoptotic DNA ladders on agarose gel electrophoresis were observed.
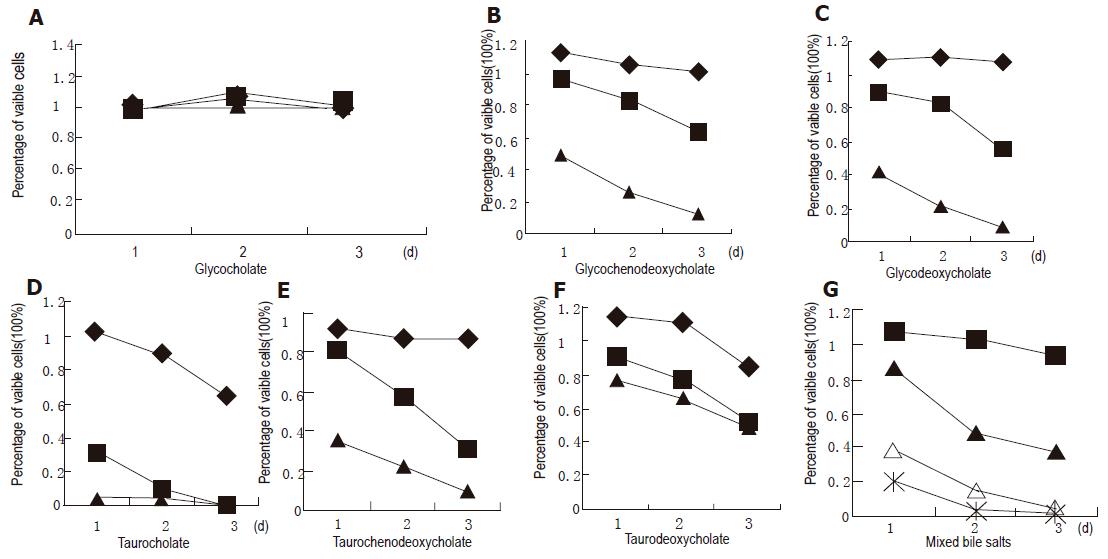
RESULTS: Except for GC, GCDC, GDC, TC, TCDC, TDC and their mixture could initiate growth inhibition of esophageal mucosal epithelial cells in a dose- and time-dependent manner. TUNEL and FCM assays demonstrated that the bile salts at 500 μmol/L and their mixture at 1 500 μmol/L induced apoptosis except for GC. The percentage of sub-G1 detected by FCM with PI staining was 83.5% in cells treated with 500 μmol/L TC for 2 h, and 19.8%, 20.4%, 25.6%, 13.5%, and 75.8% in cells treated with 500 μmol/L GCDC, TCDC, GDC, TDC, and 1 500 μmol/L mixture for 24 h, respectively, which were higher than that of the control (1.5%). The percentage was 1.4% in cells with 500 μmol/L GC for 24 h. DNA ladders on agarose gel electrophoresis were seen in cells treated with 500 μmol/L TC for 2 h and 1 500 μmol/L mixture for 24 h.
CONCLUSION: All GCDC, GDC, TC, TCDC, TDC and their mixture can inhibit growth and induce apoptosis of cultured human normal esophageal mucosal epithelial cells, but GC is well tolerated by the cells.
- Citation: Zhang R, Gong J, Wang H, Wang L. Bile salts inhibit growth and induce apoptosis of culture human normal esophageal mucosal epithelial cells. World J Gastroenterol 2005; 11(41): 6466-6471
- URL: https://www.wjgnet.com/1007-9327/full/v11/i41/6466.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i41.6466
Duodenogastroesophageal reflux (DGER) causes various gastroesophageal reflux diseases (GERD), and is associated with some complications of GERD, such as reflux esophagitis, Barrett's esophagus, and esophageal carcinoma. It is well known that the incidence of adenocarcinoma of the esophagogastric junction has been increasing during the past decade in Western countries[1]. It was also reported that the incidence of GERD is increasing in the developing countries, such as China[2]. The potential contribution of gastroduodenal components to the development of Barrett's esophagus remains unclear. But bile acids, presenting especially frequently in the refluxate of Barrett's esophagus patients, are likely to influence the development and persistence of metaplasia[3-5]. On the other hand, bile salts can enter mucosal cells in their non-ionized lipophilic form, and cause injuries to cell membranes and tight junctions, thus leading to cell necrosis[6]. It has been reported recently that bile acids upregulate the expression of COX-2 in Barrett’s esophagus biopsy explant culture systems[7]. Overexpression of COX-2 inhibits apoptosis[8,9]. However, present studies about bile salt-caused cellular injury performed on hepatocytes[10] and colon cancer cell lines[11,12] showed that different bile salts can induce cell apoptosis. Direct oligomerization of the Fas receptor (CD95/Apo-1) has been suggested as the primary causative mechanism of bile salt-mediated hepatocyte apoptosis[13]. Therefore, it is necessary to investigate the injury mechanism of bile salts on human normal esophageal epithelial cells.
There are no studies about bile salt-induced apoptosis in normal human esophageal epithelial cells. In the present study, normal human esophageal epithelial cells were cultured successfully. We characterized the kinetics of different bile salt-inhibited growth and different bile salt-induced apoptosis in cultured normal human esophageal epithelial cells. The specificity of death induction by toxic bile salts was demonstrated.
Serum-free keratinocyte medium for culture of human keratinocytes (K-SFM) and dispase were purchased from GIBCO. DMEM was from Hyclone and trypsin was from Sigma, fetal bovine serum (FBS) from Hangzhou Jiangbin Biotechnology Co., Ltd. Glycocholate (GC), glycochenodeoxycholate (GCDC), glycodeoxycholate (GDC), taurocholate (TC), taurochenodeoxycholate (TCDC), and taurodeoxycholate (TDC) were from Sigma. Terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling (TUNEL) kits were purchased from Beijing Zhongshan Golden Bridge Biotechnology Co., Ltd. Annexin V-FITC apoptosis detection kit I was from BD Biosciences.
Human normal esophageal epithelial cells, cultured from normal esophageal epithelium, were obtained from the resected esophagus of a patient suffering from esophageal carcinoma. Tissue for culture was selected just near the edge of the surgical resection specimens and far away from carcinoma lesions. Tissues were confirmed to contain no macroscopic tumor tissue or histologically detectable metaplastic cells or cancer cells[14,15]. Written informed consent was obtained from the patient for surgery and for the usage of his resected samples. Tunica mucosa was separated from the tissues with forceps, and cut into 0.2 cm × 0.5 cm fragments, then the pieces were transferred to a petri dish containing 25 U/mL dispase[16] and incubated for 18-24 h at 4 °C. Epithelial sheets were separated from the full-thickness mucosa with forceps, pooled in PBS containing 0.25% trypsin/0.02% EDTA, and incubated at 37 °C for 15-20 min with gentle pipetting to dissociate aid cells. Trypsin activity was terminated by the addition of DMEM with 10% FBS. The dissociated cells were collected and grown in K-SFM (pH 7.4) in a humidified atmosphere consisting of 50 mL/L CO2/95% air at 37 °C. K-SFM contained 3 μL epidermal growth factor, and 0.438 g L-glutamine, 0.9 mL bovine pituitary extract per 500 mL, which was based, but modified on the media of esophageal cells[17] and skin keratinocytes[18,19]. The cells were subcultured and those in passages 3-6 were selected to be used in the study. In the following study, different bile salts were added into the K-SFM (pH 7.1-7.3).
3-[4,5-Dimethylthiaolyl]-2,5-diphenyl-tetrazolium bromide (MTT) assay was conducted to determine the cell proliferation. Cells were treated with six bile salts at the concentrations of 500, 250, and 50 μmol/L, and their mixture at the concentrations of 1 500, 1 000, 500, and 250 μmol/L at the ratio 2:2:1:2:2:1.
Cells were seeded on a 96-well plate (4-6×104 cells/well). After 24 h of seeding, cells were treated with different bile salts for 3 d and untreated cells served as a control. Prior to the determination, 10 μL of the 2.5 g/L stock solution of MTT was added to each well. After 4 h of incubation, the culture media were discarded followed by addition of 100 mL of DMSO to each well and vibration for 10 min. The absorbance (A) was measured at 492 nm with a microplate reader. The percentage of viable cells was calculated as follows: (A of experimental group/A of control group)×100%.
Cells from the medium supernatant and adherent cells treated with bile salts were collected and pelleted at 1 200 U/min. The harvested cells were fixed with 1 mL of 75% cold ethanol at -20 °C for a night, and then washed with PBS. Cell pellets were incubated with 10 μg/mL RNAse and stained with 50 μg/mL propidium iodide (PI) for 30 min in the dark. Samples were analyzed using a FACSCalibur flow cytometer (FCM) with an excitation wavelength of 488 nm. The resulting histograms were analyzed by the program CELLQuest. A total of 2 104 cells were detected by FCM in each of the samples.
Cells from the medium supernatant and adherent cells treated with bile salts were collected and pelleted at 1 200 U/min. Pellets were washed twice with cold PBS and then resuspended in a binding buffer at a concentration of 1×106 cells/mL, and two volumes of the 100 μL solution (1×105 cells) were transferred to two 5-mL culture tubes. Five microliters of annexin V-FITC and 5 μL of PI were added into each of the 100 μL solution, and the cells were gently vortexed and incubated for 15 min at room temperature in the dark. The samples, to which 400 μL of 1× binding buffer was added, were analyzed by FACSCalibur FCM within 1 h. A total of 2×104 cells were detected by FCM in each of the samples.
Apoptosis of cells was analyzed using an in situ cell apoptosis detection kit based on the TUNEL technique. Cells were grown on chamber glass culture slides and treated with bile salts. To avoid adherence of the apoptotic cells, the slides were coated with poly-lysine. In brief, after the cells were treated with or without bile salts for the indicated time, they were fixed overnight in 100 g/L formaldehyde, then treated with proteinase K and H2O2, labeled with dUTP in a humidified box at 37 °C for 1 h. The cells without addition of TdT enzyme were used as a negative control. The positive cells/the total cells were calculated using an image-analysis system. A mean of 20 adjacent fields, at a magnification of ×400, was analyzed for each section[21].
A total of 106-107 cells treated with bile salts were collected and low molecular weight DNA was extracted using a cell apoptosis DNA ladder extraction kit (Beijing Dingguo Biotechnology Co., Ltd). Standard loading buffer was added, 20 μL DNA samples was run on an 1% agarose gel containing 0.1% ethidium bromide in TAE buffer (40 mmol/L Tris, 20 mmol/L sodium acetate, and 1 mmol/L EDTA, pH 8.0).
All values were expressed as mean±SD. Statistical differences between means were calculated by the Student's t-test and the χ2 test. P < 0.05 was considered statistically significant.
Human normal esophageal mucosal epithelial cells were cultured with serum-free keratinocyte medium successfully without contamination of fibroblasts, and could be passaged for more than 20 times without senescence. Cells in passages 3-6 were selected for the following research.
The cell viability was determined by MTT assay (Figure 1). Except for GC, the other five bile salts and their mixture inhibited the growth of normal human esophageal mucosal epithelial cells in a dose- and time-dependent manner. The mixture at 1 500 μmol/L had an inhibitory effect of 79% on esophageal mucosal epithelial cells after 24-h treatment. Cell growth was suppressed by 96% after 24-h treatment with TC at 500 μmol/L, higher than that after being treated with other bile salts at the same concentration (P < 0.01). Cell growth was suppressed by 51%, 58%, 65%, and 24% after 24-h treatment with GCDC, GDC, TCDC, and TDC at 500 μmol/L, respectively.
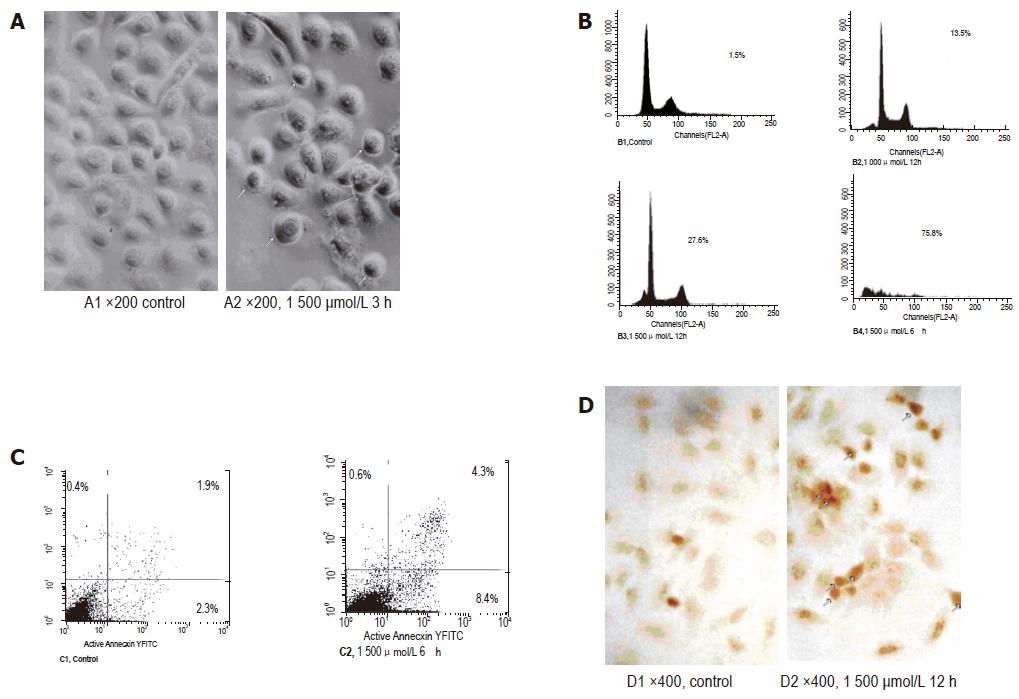
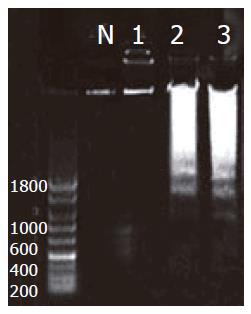
The mixture of bile salts induced apoptosis of cultured human normal mucosal epithelial cells. Morphological criteria of cell apoptosis, such as membrane blebbing, cell shrinkage, and nuclear condensation, were assessed 3 h after the addition of the mixture at the concentrations of 1 500 μmol/L by phase-contrast video microscopy (Figure 2A). FCM assays with only PI staining showed that 27.6% and 75.8% of the cells treated with 1 500 μmol/L bile salt mixture for 12 and 24 h, respectively, were in sub-G1, which were higher than that of the control (1.5%, P<0.01), and 13.5% of the cells treated with 1 000 μmol/L bile salt mixture for 12 h were in sub-G1 (Figure 2B). Early apoptotic cells, detected by FCM with annexin-V conjugated with PI staining, reached 8.4%, 6 h after being treated with 1 500 μmol/L bile salt mixture, higher than that of the control (2.3%, P < 0.01, Figure 2C). TUNEL assay also proved that bile salt mixture induced cell apoptosis, because the number of positively stained nuclei was (30 ± 8)% in cells after being treated with 1 500 μmol/L bile salt mixture for 12 h, which was significantly higher than that of the control (3% ± 2%, P < 0.01, Figure 2D). DNA laddering, a typical sign of apoptosis, was detectable after being treated with 1 500 μmol/L bile salt mixture for 24 h (Figure 3).
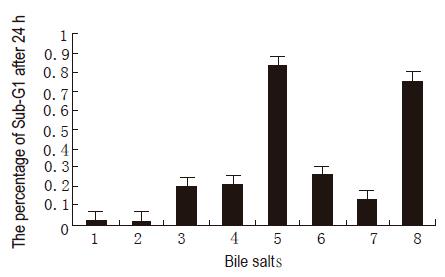
The assays of the six bile salts revealed that the other five bile salts, except for GC, induced apoptosis of esophageal mucosal epithelial cells. The percentages of sub-G1 in cells treated with different bile salts for 24 h are shown in Figure 4. The bile salts induced apoptosis in a time-dependent manner, 83.5% of cells were in sub-G1 treated with 500 μmol/L TC for 2 h, and the percentages were 19.8%, 20.4%, 25.6%, and 13.5% in cells treated with 500 μmol/L GCDC, TCDC, GDC, and TDC for 24 h, respectively. FCM with annexin-V conjugated with PI staining showed that early apoptotic cells reached 24.6% in cells treated with 500 μmol/L TC for 30 min, and 6.8%, 7.6%, 8.3%, and 5.1% in cells treated with 500 μmol/L GCDC, GDC, TCDC, and TDC for 6 h, respectively. They were all higher than that of the control (1.9%, P < 0.05). The TUNEL assay also revealed that GC did not induce apoptosis, but the other five bile salts did. The positively stained nuclei were (53 ± 8)%, (2 ± 2)%, (20 ± 4)%, (18± 3)%, (24 ± 6)%, and (16 ± 3)% in cells treated with 500 μmol/L TC for only 1 h, and 500 μmol/L GC, GCDC, GDC, TCDC, and TDC for 24 h, respectively. Except for GC, all the others were significantly higher than that of the control (3 ± 2)%, P < 0.01). DNA fragments were detected in cells treated with TC at 500 μmol/L for 2 h (Figure 3).
The injury mechanism of reflux duodenal components underlying DGER is still controversial. Bile acids and bile salts play a most important role[6]. But the causative mechanism of bile salts has not yet been elucidated in detail.
Bile acids constitute 67% of the normal bile, and are conjugated with glycine or taurine. The normal bile acids consist of 40% cholic acids, 40% chenodeoxycholic acid, and 20% deoxycholic acids, and a minor fraction of lithocholic acid and ursodeoxycholic acid[22]. In the present study, we investigated the effect of GC, GCDC, GDC, TC, TCDC, and TDC in esophageal epithelial cells. In order to speculate the effect of bile in the duodenoesophageal reflux in vivo, we also observed the effect of the mixture of these six bile salts. Moreover, the concentrations of bile salts in our study were selected from 25 to 500 μmol/L in the different bile salts and from 50 to 1 500 μmol/L in the mixture. This is because the total bile acid concentration in esophagus of patients suffering from reflux esophagitis is 0.89 mg/mL[23].
MTT assay in this report demonstrated that five bile salts and the mixture, except for GC, could inhibit the growth of cultured human normal esophageal mucosal epithelial cells in a dose- and time-dependent manner. The induced cell death was a major reason for the cell growth inhibition. GCDC, GDC, TC, TCDC, TDC and the mixture caused typical apoptotic alterations including the morphological changes assessed by phase-contrast video microscopy and TUNEL assay, positive cells stained with annexin-V assessed by FCM, apoptotic sub-G1 peak assessed by FCM with PI staining, and DNA fragmentation by agarose gel electrophoresis assay. However, these apoptosis changes were not seen in cells treated with GC.
Differences in the effect of bile salts on cultured normal human esophageal mucosal epithelial cells and hepatocytes and colon cancer cell line death were identified in this study. Studies performed on hepatocytes showed that glycine-conjugated bile acids, such as glycocholic and glycochenodeoxycholic acids, induce hepatocyte apoptosis in vitro[24], whereas taurine-conjugated bile acids, such as taurocholic and taurochenodeoxycholic acids, are well tolerated by hepatocytes[25,26]. Cell apoptosis is specifically induced by toxic (hydrophobic) bile salts such as deoxycholate and dihydroxy bile salt, whereas the conjugated bile salt GDC and the trihydroxy bile salt and its conjugate GC do not induce apoptosis of colorectal cancer cell lines[11], which are not in accordance with our results. Conversely, hepatocyte-cytotoxic glycine-conjugated bile acids such as GC, which induce hepatocyte apoptosis in vitro[24], do not induce apoptosis in esophageal mucosal epithelial cells. Whereas the hepatocyte-tolerated TC and TCDC[25,26] could induce apoptosis of esophageal mucosal epithelial cells. Our results also showed that TC was the most toxic to esophageal mucosal epithelial cells compared to the other four bile salts. We speculate that the mechanisms of the bile salts-induced apoptosis in human esophageal epithelial cells are different from those in hepatocytes or colorectal cancer cell lines. It was reported that direct oligomerization of the Fas receptor could be suggested as the primary causative mechanism of bile salt-mediated hepatocyte apoptosis[13,27,28]. Some hydrophobic bile acids such as TC could activate PI3K-dependent survival pathways, which prevent their otherwise inherent toxicity in hepatocytes[10,29]. As opposed to hepatocyte death mediated by bile acids, bile salt-induced apoptosis of human colon cancer cell lines involves the mitochondrial transmembrane potential but not the CD95 (Fas/Apo-1) receptor[11,30]. Studies are needed to gain further insight into the effect of bile salts on human esophageal mucosal epithelial cells.
In conclusion, GCDC, GDC, TC, TCDC, and TDC and their mixture inhibit the growth and induce apoptosis of cultured human normal esophageal mucosal epithelial cells in a dose- and time-dependent manner. But GC is not cytotoxic to the esophageal mucosal epithelial cells. Studies are needed to gain further insight into the effect of bile salts on human esophageal mucosal epithelial cells.
We thank Dr. Bingheng Zhang and Dr. Xiaoge Zhao, Central Laboratory for Biomedical Research of Xi’an Jiaotong University Medical School, for their help on the FCM assays.
Co-first-authors: Ru Zhang and Jun Gong
Co-correspondence: Ru Zhang
Science Editor Wang XL Language Editor Elsevier HK
| 1. | Cameron AJ, Lomboy CT, Pera M, Carpenter HA. Adenocarcinoma of the esophagogastric junction and Barrett's esophagus. Gastroenterology. 1995;109:1541-1546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 280] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 2. | Li ZS, Xu GM, Liu Q. Epidemiology of gastroesophageal reflux disease in Shanghai adults part I: Suggestive symptoms and influencing factors. Jiefangjun Yixue Zazhi. 1997;22:259-2623. |
| 3. | Jankowski JA, Anderson M. Review article: management of oesophageal adenocarcinoma-control of acid, bile and inflammation in intervention strategies for Barrett's oesophagus. Aliment Pharmacol Ther. 2004;20:71-80 discussion 95-96. |
| 4. | Kondo K, Kojima H, Akiyama S, Ito K, Takagi H. Pathogenesis of adenocarcinoma induced by gastrojejunostomy in Wistar rats: role of duodenogastric reflux. Carcinogenesis. 1995;16:1747-1751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Miwa K, Miyashita T, Hattori T. Reflux of duodenal or gastroduodenal contents induces esophageal carcinoma in rats. Nihon Rinsho. 2004;62:1433-1438. [PubMed] |
| 6. | Stein HJ, Kauer WK, Feussner H, Siewert JR. Bile acids as components of the duodenogastric refluxate: detection, relationship to bilirubin, mechanism of injury, and clinical relevance. Hepatogastroenterology. 1999;46:66-73. [PubMed] |
| 7. | Shirvani VN, Ouatu-Lascar R, Kaur BS, Omary MB, Triadafilopoulos G. Cyclooxygenase 2 expression in Barrett's esophagus and adenocarcinoma: Ex vivo induction by bile salts and acid exposure. Gastroenterology. 2000;118:487-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 313] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 8. | Tsujii M, DuBois RN. Alterations in cellular adhesion and apoptosis in epithelial cells overexpressing prostaglandin endoperoxide synthase 2. Cell. 1995;83:493-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1569] [Cited by in RCA: 1565] [Article Influence: 52.2] [Reference Citation Analysis (0)] |
| 9. | Sawaoka H, Kawano S, Tsuji S, Tsujii M, Gunawan ES, Takei Y, Nagano K, Hori M. Cyclooxygenase-2 inhibitors suppress the growth of gastric cancer xenografts via induction of apoptosis in nude mice. Am J Physiol. 1998;274:G1061-G1067. [PubMed] |
| 10. | Torchia EC, Stolz A, Agellon LB. Differential modulation of cellular death and survival pathways by conjugated bile acids. BMC Biochem. 2001;2:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Schlottman K, Wachs FP, Krieg RC, Kullmann F, Schölmerich J, Rogler G. Characterization of bile salt-induced apoptosis in colon cancer cell lines. Cancer Res. 2000;60:4270-4276. [PubMed] |
| 12. | Milovic V, Teller IC, Faust D, Caspary WF, Stein J. Effects of deoxycholate on human colon cancer cells: apoptosis or proliferation. Eur J Clin Invest. 2002;32:29-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 73] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Sodeman T, Bronk SF, Roberts PJ, Miyoshi H, Gores GJ. Bile salts mediate hepatocyte apoptosis by increasing cell surface trafficking of Fas. Am J Physiol Gastrointest Liver Physiol. 2000;278:G992-G999. [PubMed] |
| 14. | Washington K, Gottfried MR, Telen MJ. Tissue culture of epithelium derived from Barrett's oesophagus. Gut. 1994;35:879-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Kawabe A, Shimada Y, Soma T, Maeda M, Itami A, Kaganoi J, Kiyono T, Imamura M. Production of prostaglandinE2 via bile acid is enhanced by trypsin and acid in normal human esophageal epithelial cells. Life Sci. 2004;75:21-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | David AJ, Paul JB, Darrin DB. Culture of human keratinocytes in defined serum-free mudium. FOCUS of GIBCO. 1997;19:2-5. |
| 17. | Fitzgerald RC, Farthing MJ, Triadafilopoulos G. Novel adaptation of brush cytology technique for short-term primary culture of squamous and Barrett's esophageal cells. Gastrointest Endosc. 2001;54:186-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Font J, Braut-Boucher F, Pichon J, Noel-Hudson MS, Muriel MP, Bonnet M, Wepierre J, Aubery M. A new three-dimensional culture of human keratinocytes: optimization of differentiation. Cell Biol Toxicol. 1994;10:353-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Harvima IT, Lappalainen K, Hirvonen MR, Mättö M, Kivinen PK, Hyttinen M, Pelkonen J, Naukkarinen A. Heparin modulates the growth and adherence and augments the growth-inhibitory action of TNF-alpha on cultured human keratinocytes. J Cell Biochem. 2004;92:372-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Lecoeur H, Prévost MC, Gougeon ML. Oncosis is associated with exposure of phosphatidylserine residues on the outside layer of the plasma membrane: a reconsideration of the specificity of the annexin V/propidium iodide assay. Cytometry. 2001;44:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 21. | Coppola D, Schreiber RH, Mora L, Dalton W, Karl RC. Significance of Fas and retinoblastoma protein expression during the progression of Barrett's metaplasia to adenocarcinoma. Ann Surg Oncol. 1999;6:298-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Guoming X, Meiyun K, Jinyan L. Bile acid reflux related disease. Shanghai Science and Technology Press. 2002;9:24. |
| 23. | Stein HJ, Feussner H, Kauer W, DeMeester TR, Siewert JR. Alkaline gastroesophageal reflux: assessment by ambulatory esophageal aspiration and pH monitoring. Am J Surg. 1994;167:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 79] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Agellon LB, Torchia EC. Intracellular transport of bile acids. Biochim Biophys Acta. 2000;1486:198-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Torchia EC, Agellon LB. Bile acid-induced morphological changes in hepatoma cells with elevated sodium-dependent bile acid uptake capacity. Eur J Cell Biol. 1997;74:190-196. [PubMed] |
| 26. | Roberts LR, Kurosawa H, Bronk SF, Fesmier PJ, Agellon LB, Leung WY, Mao F, Gores GJ. Cathepsin B contributes to bile salt-induced apoptosis of rat hepatocytes. Gastroenterology. 1997;113:1714-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 131] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 27. | Faubion WA, Guicciardi ME, Miyoshi H, Bronk SF, Roberts PJ, Svingen PA, Kaufmann SH, Gores GJ. Toxic bile salts induce rodent hepatocyte apoptosis via direct activation of Fas. J Clin Invest. 1999;103:137-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 420] [Cited by in RCA: 411] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 28. | Qiao L, Studer E, Leach K, McKinstry R, Gupta S, Decker R, Kukreja R, Valerie K, Nagarkatti P, El Deiry W. Deoxycholic acid (DCA) causes ligand-independent activation of epidermal growth factor receptor (EGFR) and FAS receptor in primary hepatocytes: inhibition of EGFR/mitogen-activated protein kinase-signaling module enhances DCA-induced apoptosis. Mol Biol Cell. 2001;12:2629-2645. [RCA] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 183] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 29. | Rust C, Karnitz LM, Paya CV, Moscat J, Simari RD, Gores GJ. The bile acid taurochenodeoxycholate activates a phosphatidylinositol 3-kinase-dependent survival signaling cascade. J Biol Chem. 2000;275:20210-20216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 144] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 30. | Wachs FP, Krieg RC, Rodrigues CM, Messmann H, Kullmann F, Knüchel-Clarke R, Schölmerich J, Rogler G, Schlottmann K. Bile salt-induced apoptosis in human colon cancer cell lines involves the mitochondrial transmembrane potential but not the CD95 (Fas/Apo-1) receptor. Int J Colorectal Dis. 2005;20:103-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |