Published online Aug 21, 2005. doi: 10.3748/wjg.v11.i31.4879
Revised: January 23, 2005
Accepted: January 26, 2005
Published online: August 21, 2005
AIM: To evaluate the seroprevalence of hepatitis B surface antigen (HBsAg) in 13 581 women at reproductive age and the hepatitis B e antigen (HBeAg)/anti-HBe status as well as serum hepatitis B virus (HBV)-DNA levels in a subgroup of HBsAg(+) pregnant women at labor in Greece.
METHODS: Serological markers were detected using enzyme immunoassays. Serum HBV-DNA was determined by a sensitive quantitative PCR assay. Statistical analysis of data was based on parametric methodology.
RESULTS: Overall, 1.156% of women were HBsAg(+) and the majority of them (71.3%) were Albanian. The prevalence of HBsAg was 5.1% in Albanian women, 4.2% in Asian women and 1.14% in women from Eastern European countries. The prevalence of HBsAg in African (0.36%) and Greek women (0.29%) was very low. Only 4.45% of HBsAg(+) women were also HBeAg(+) whereas the vast majority of them were HBeAg(-)/anti-HBe(+). Undetectable levels of viremia (<200 copies/mL) were observed in 32.26% of pregnant women at labor and 29.03% exhibited extremely low levels of viral replication (<400 copies/mL). Only two pregnant women exhibited extremely high serum HBV-DNA levels (>10 000 000 copies/mL), whereas 32.26% exhibited HBV-DNA levels between 1 500 and 40 000 copies/mL.
CONCLUSION: The overall prevalence of HBsAg is relatively low among women at reproductive age in Greece but is higher enough among specific populations. The HBeAg(-)/anti-HBe(+) serological status and the extremely low or even undetectable viral replicative status in the majority of HBsAg(+) women of our study population, suggest that only a small proportion of HBsAg(+) women in Greece exhibit a high risk for vertical transmission of the infection.
- Citation: Elefsiniotis IS, Glynou I, Magaziotou I, Pantazis KD, Fotos NV, Brokalaki H, Kada H, Saroglou G. HBeAg negative serological status and low viral replication levels characterize chronic hepatitis B virus-infected women at reproductive age in Greece: A one-year prospective single center study. World J Gastroenterol 2005; 11(31): 4879-4882
- URL: https://www.wjgnet.com/1007-9327/full/v11/i31/4879.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i31.4879
Worldwide, about 350 million people are chronically infected with hepatitis B virus (HBV)[1]. Vertical transmission of the infection occurs usually in peri-natal period and is the major cause of HBV transmission in endemic countries of the world. Mother to infant transmission represents a basic factor in maintaining chronic HBV infection and usually depends on the degree of maternal infectivity, especially in peri-natal period[2]. Vertical transmission of the infection is mainly seen in infants born from hepatitis B e antigen (HBeAg)(+) mothers with very high levels of viremia and maternal serum HBV-DNA levels are positively associated with immunoprophylaxis failure[2,3].
Hepatitis B has long been a serious public health problem in Greece. Historically, Greece has had the highest burden of HBV infection in the European Union and unfortunately a hepatitis B prevention program aimed at high-risk groups in 1982, had little impact on disease incidence or prevalence[4]. In recent years, HBV vaccination programs, demographic and socio-economic changes, medical precautions and screening of blood donors have resulted in a significant decline in chronic HBV infection in our country[4,5]. However, the entrance of a great number of refugees, especially from endemic countries of HBV infection in the last decade, has possibly led to alteration of the epidemiological data, so these data have to be re-evaluated.
In our study we examined the seroprevalence of hepatitis B surface antigen (HBsAg) in a large multinational group of women at reproductive age and evaluated the presence of HBeAg, antibody to HBeAg (anti-HBeAg) as well as antibody to hepatitis C virus (anti-HCV) in HBsAg(+) individuals. Moreover we measured the serum HBV-DNA levels in a subgroup of HBsAg(+)/anti-HCV(-) pregnant women at labor, in order to gain information about maternal viral load at this important period, a factor positively correlated with vertical transmission of the infection.
Between August 2003 and August 2004, a total of 13 581 women at reproductive age (range 16-45 years) were prospectively evaluated at the Department of Obstetrics and Gynecology of the Maternal Hospital ‘Helena Venizelou’ of Athens, Greece. HBsAg, HBeAg, anti-HBeAg, and antibody to hepatitis B core antigen (anti-HBcAg) as well as anti-HCV were detected by routine commercially available enzyme immunoassays (Abbott Laboratories, Abbott Park, IL, USA). All women of the study were screened for HBsAg whereas the rest of the serological markers were evaluated only in HBsAg(+) ones. Antibody to hepatitis D virus (anti-HDV) and antibody to HIV (anti-HIV) were not detected. Serum HBV-DNA was determined by a sensitive, commercially available quantitative PCR assay (COBAS-Amplicor HBV Monitor, Version 2, Roche, Basel, Switzerland), with a lower limit of quantification of 200 copies/mL in a subgroup of HBsAg(+)/anti-HCV(-) pregnant women of the study population, with available serum samples, at labor.
Statistical analysis of data was based on parametric methodology. Student’s t-test and χ2 test were used. P<0.05 was statistically significant. The study was reviewed and approved by the local ethics committee. The study protocol conforms to the ethical guidelines of the Declaration of Helsinki.
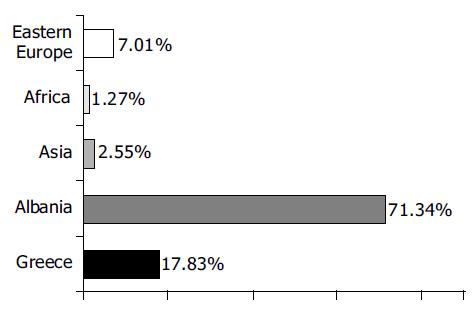
The majority of the study population came from Greece (70.31%) whereas 15.96% came from Albania, 7.06% from Eastern European countries (Russia, Romania, and Bulgaria), 4.09% from African countries, 0.69% from Asian countries, 0.99% from countries of Northwestern Europe, 0.46% from Australia and 0.43% from North American countries. Overall, 157 of 13 581 females (1.156%) were HBsAg(+) and the vast majority of them (112/157, 71.3%) were Albanian. The participation of each national group in HBsAg(+) cases of the study population is presented in Figure 1. None of the females from countries of North America, Northwestern Europe, and Australia (countries of low prevalence of HBV infection) was HBsAg(+).
The seroprevalence of HBsAg was 5.1% in women from Albania, representing the higher seroprevalence rate among the national groups of the study population, followed by 4.2% in Asian women and 1.14% in women from Eastern European countries. The seroprevalence of HBsAg in African (0.36%) and Greek women (0.29%) was very low, compared to the mean seroprevalence rate of the study population (P<0.05). Overall, only 4.45% of HBsAg(+) women were also HBeAg(+) whereas the vast majority of them were HBeAg(-)/anti-HBeAg(+). HBeAg(+) cases represented 10.7% and 3.6% of Greek and Albanian HBsAg(+) women respectively, whereas 92.9% of Greek and Albanian HBsAg(+) women, 90.9% of Eastern European countries HBsAg(+) women and all Asian/African HBsAg(+) women were HBeAg(-)/anti-HBeAg(+). Only 3 of 157 women (1.91%) with chronic HBV infection were HBV/HCV coinfected.
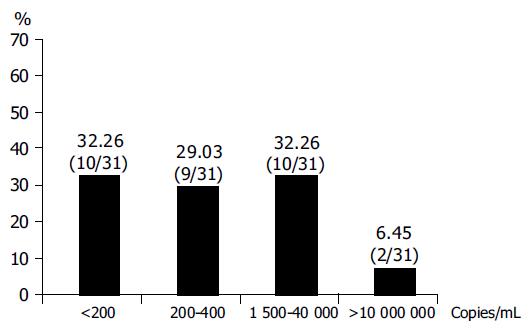
Serum HBV-DNA was quantified in 31 HBsAg(+)/anti-HCV(-) pregnant women of our study population with available serum samples at labor. Only one of them was HBeAg(+) whereas the vast majority of them were HBeAg(-)/anti-HBeAg(+), as it was the majority of HBsAg(+) cases of the study population. Twenty-two of them were Albanian (22/31, 70.96%), six of them (6/31, 19.35%) were Greek and the rest three were from an Eastern European, an Asian and an African country, respectively. Undetectable levels of serum HBV-DNA (<200 copies/mL) were observed in 10 of 31 (32.26%) pregnant women at labor and 9 of 31 (29.03%) pregnant women exhibited extremely low levels of viral replication (lower than 400 copies/mL) during this important period. Only two, one HBeAg(-) and one HBeAg(+), of 31 pregnant women (6.45%) evaluated for HBV viral load, exhibited extremely high serum HBV-DNA levels (19 800 000 and 85 500 000 copies/mL, respectively) whereas the rest of the 10 women evaluated (32.26%) exhibited HBV-DNA levels between 1 500 and 40 000 copies/mL. Serum HBV-DNA levels in this subgroup of our study population are presented in Figure 2. As we can see from this figure, the majority (61.29%) of chronic HBV-infected pregnant women evaluated for serum HBV-DNA levels at labor by a very sensitive PCR assay, exhibited undetectable (<200 copies/mL) or extremely low (<400 copies/mL) levels.
Epidemiological data on the prevalence of serological markers of HBV infection in women at reproductive age in Greece are limited. It is estimated from previous studies that in Greece, the HBsAg carrier rate in pregnant women is 2.8-3.0%[6]. In our study we found that the mean prevalence of HBsAg in 13 581 women at reproductive age from multinational origin, was relatively low (1.156%) and the vast majority of HBsAg-positive women (71.3%) came from Albania, representing the 5.1% of the Albanian women of the study population.
Although the seroprevalence rate of HBsAg in Albanian (5.1%) and Asian (4.2%) women was significantly higher than in Greek women (0.29%, P<0.001), which was significantly lower than the mean rate of the study population (1.156%, P<0.05), suggesting that there is a significant decline in seroprevalence of HBsAg in the refugees living in Greece in the last decade. In 1995 Malamitsi-Puchner et al[7], reported that 13.4% of 500 Albanian pregnant women evaluated in a Greek Maternal Hospital are HBsAg(+) and 7.5% of them are also HBeAg(+), representing an endemic and highly infective group of HBV infection. Significant socio-economic changes, specific precautions due to the knowledge of the modes of transmission of the infection and HBV vaccination programs may have possibly led to this decline observed nowadays in these specific populations.
Maternal HBeAg-positivity in peri-natal period is of great importance for the vertical transmission of HBV infection resulting in extremely higher rates of mother to infant transmission compared to infant born from HBeAg(-) mothers[2,3,8]. In our study, the vast majority (>90%) of HBsAg(+) women were HBeAg(-)/anti-HBeAg(+), resulting possibly in the low rates of peri-natal transmission of HBV infection and passive/active immunoprophylaxis failure observed in our country, a finding that needs further investigation. Moreover, maternal serum HBV-DNA at labor was undetectable or extremely low in the majority of pregnant women of the study population evaluated, by a sensitive PCR assay. The predominance of HBeAg(-)/anti-HBeAg(+) serological status in combination with the low levels of viremia observed in the majority of chronic HBV-infected women of our study population, suggests that chronic HBV-infected women at reproductive age in Greece represent a group of low infectivity, resulting possibly in low vertical transmission and passive/active immunoprophylaxis failure rates.
Intra-uterine/transplacental transmission of HBV infection in infants born from HBsAg(+) mothers observed in endemic countries is positively correlated to HBeAg(+) maternal serological status and high levels of maternal serum HBV-DNA. It is believed that transplacental transmission of HBV infection is a major cause of immunoprophylaxis failure and this mode of transmission can be effectively reduced by administration of hepatitis B immune globulin (HBIG) or lamivudine in the third trimester of HBsAg(+) pregnant women[9]. It seems that this problem is not of clinical significance in our country, because of the relatively low seroprevalence rates of HBsAg observed in our study population, and the serological and virological data of chronic HBV-infected women at reproductive age in Greece, as previously noted.
In Greece, both active (HBV vaccine) and passive (HBIG) immunoprophylaxis are the current clinical practice in newborns from HBsAg(+) mothers, irrespective of maternal serological (HBeAg(+) or HBeAg(-)) and/or virological status. Studies from hyper-endemic countries of HBV infection suggest that there is no clear benefit of passive-active vs active immunization alone for chronic HBV infection in infants born from HBsAg(+)/HBeAg(-) mothers[10]. The estimated efficacy of HBV vaccination alone without HBIG is 84% in infants born from HBeAg(+) mothers and 100% in those born from HBeAg(-) ones, according to a study from endemic Vietnam[11]. The high cost of HBIG and the serological and virological data of women at reproductive age in our study, may suggest that passive-active immunoprophylaxis of infants born from chronic HBV-infected mothers in our country, possibly represents an over-protection strategy, at least in a signif-icant proportion of them, especially from HBeAg(-)/anti-HBeAg(+) mothers with HBV-DNA <400 copies/mL at labor. This possibility needs further investigation in large-scale clinical trials. Moreover, more than one third (38.7%) of HBsAg(+)/anti-HBeAg(+) women of our study population exhibited active viral replication at labor and some of them exhibited extremely high viral load levels, representing possibly an infection with a mutant HBV variant (precore mutant), a finding that needs further investigation.
In conclusion, the overall seroprevalence rate of HBsAg is relatively low in women at reproductive age in Greece but is rather higher in specific populations (Albanian, Asian) who need screening, vaccination, and immunoprophylaxis programs in order to decline further the rates of peri-natally acquired HBV infection. The HBeAg(–)/anti-HBeAg(+) serological status and the extremely low or even undetectable viral replicative status in the majority of HBsAg(+) women suggest that only a small proportion of HBsAg(+) women in Greece exhibit an extremely high risk for vertical transmission of the infection.
Science Editor Wang XL and Guo SY Language Editor Elsevier HK
| 1. | The World Health Report. WHO 1998. . |
| 2. | Söderström A, Norkrans G, Lindh M. Hepatitis B virus DNA during pregnancy and post partum: aspects on vertical transmission. Scand J Infect Dis. 2003;35:814-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 94] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Wang Z, Zhang J, Yang H, Li X, Wen S, Guo Y, Sun J, Hou J. Quantitative analysis of HBV DNA level and HBeAg titer in hepatitis B surface antigen positive mothers and their babies: HBeAg passage through the placenta and the rate of decay in babies. J Med Virol. 2003;71:360-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 134] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 4. | Papaevangelou G. Hepatitis B immunization programme: lessons learnt in Greece. Vaccine. 1998;16 Suppl:S45-S47. [PubMed] |
| 5. | Stamouli M, Gizaris V, Totos G, Papaevangelou G. Decline of hepatitis B infection in Greece. Eur J Epidemiol. 1999;15:447-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Papaevangelou G, Farmaki G, Kada H. Hepatitis B maternal-fetal transmission in Southern Europe. Intervirology. 1998;41:197-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Malamitsi-Puchner A, Papacharitonos S, Sotos D, Tzala L, Psichogiou M, Hatzakis A, Evangelopoulou A, Michalas S. Prevalence study of different hepatitis markers among pregnant Albanian refugees in Greece. Eur J Epidemiol. 1996;12:297-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Stevens CE, Neurath RA, Beasley RP, Szmuness W. HBeAg and anti-HBe detection by radioimmunoassay: correlation with vertical transmission of hepatitis B virus in Taiwan. J Med Virol. 1979;3:237-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 188] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 9. | van Zonneveld M, van Nunen AB, Niesters HG, de Man RA, Schalm SW, Janssen HL. Lamivudine treatment during pregnancy to prevent perinatal transmission of hepatitis B virus infection. J Viral Hepat. 2003;10:294-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 184] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 10. | Yang YJ, Liu CC, Chen TJ, Lee MF, Chen SH, Shih HH, Chang MH. Role of hepatitis B immunoglobulin in infants born to hepatitis B e antigen-negative carrier mothers in Taiwan. Pediatr Infect Dis J. 2003;22:584-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Milne A, West DJ, Chinh DV, Moyes CD, Poerschke G. Field evaluation of the efficacy and immunogenicity of recombinant hepatitis B vaccine without HBIG in newborn Vietnamese infants. J Med Virol. 2002;67:327-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |